Abstract
Purpose
To evaluate postoperative outcomes and visual performance in intermediate distance after implantation of a +1.5 diopters (D) addition, aspheric, rotational asymmetric multifocal intraocular lens (MIOL).
Methods
Patients underwent bilateral cataract surgery with implantation of an aspheric, asymmetric MIOL with +1.5 D near addition. A complete ophthalmological examination was performed preoperatively and 3 months postoperatively. The main outcome measures were monocular and binocular uncorrected distance visual acuity (UDVA), corrected distance visual acuity (CDVA), uncorrected intermediate visual acuity (UIVA), distance corrected intermediate visual acuity (DCIVA), uncorrected near visual acuity (UNVA) and distance corrected keratometry, and manifest refraction. The Salzburg Reading Desk was used to analyze unilateral and bilateral functional vision with uncorrected and corrected reading acuity, reading distance, reading speed, and the smallest log-scaled print size that could be read effectively at near and intermediate distances.
Results
The study comprised 60 eyes of 30 patients (mean age, 68.30 ± 9.26 years; range, 34 to 80 years). There was significant improvement in UDVA and CDVA. Mean UIVA was 0.01 ± 0.09 logarithm of the minimum angle of resolution (logMAR) and mean DCIVA was -0.02 ± 0.11 logMAR. In Salzburg Reading Desk analysis for UIVA, the mean subjective intermediate distance was 67.58 ± 8.59 cm with mean UIVA of -0.02 ± 0.09 logMAR and mean word count of 96.38 ± 28.32 words/min.
Patient expectations regarding refractive outcomes and spectacle independence have increased substantially in the recent past, and cataract patients have the same demands as refractive patients. For ophthalmologists, this means that the final goal is to achieve accurate target refraction with less than ±0.5 diopters (D) postoperatively [1].
Recent advances in microsurgery and the latest developments in intraocular lenses (IOLs) have allowed surgeons to achieve more accurate and predictable postoperative refractive results. Still, society focuses more on intermediate tasks than actual near activities.
Regarding uncorrected intermediate visual acuity (UIVA), great variability in results has been observed with the use of different multifocal IOL models. Improvement in intermediate vision is still needed to increase the level of patient satisfaction. In the last few years, more multifocal intraocular lens (MIOL) models have been developed to create improved intermediate focus for patients [234567].
The present study evaluated bilateral implantation of the Lentis-313MF15 (Oculentis, Berlin, Germany), a new aspheric, rotational asymmetric MIOL with +1.5 D near addition. To our knowledge, this is the first study to focus on intermediate performance of a MIOL designed to improve this certain distance.
The purpose of this study was to evaluate functional results and intermediate performance after implantation of this type of low-add MIOL. Surgical complications during follow-up and subjective patient questionnaires regarding patient satisfaction were also evaluated.
This prospective, non-comparative, non-randomized clinical study enrolled 30 patients. Patients with bilateral cataract and those seeking spectacle independence in intermediate distances were included. Exclusion criteria were history of glaucoma or retinal detachment, corneal disease, regular corneal astigmatism greater 0.75 D, irregular corneal astigmatism, abnormal iris, macular degeneration or retinopathy, neurophthalmic disease, history of ocular inflammation or previous ocular surgery, and expected postoperative corrected distance visual acuity (CDVA) of ≤0.3 logarithm of the minimum angle of resolution (logMAR). In all cases, binocular cataract surgery with implantation of an aspheric, asymmetric MIOL was performed. All patients were adequately informed and signed consent forms. The study adhered to tenets of the Declaration of Helsinki and was approved by the local ethics committee.
A complete ophthalmological examination was performed before surgery, including manifest refraction, keratometry, uncorrected distance visual acuity (UDVA), CDVA, Goldmann applanation tonometry, slit lamp examination, corneal topography, biometry (IOL Master v.4.3; Carl Zeiss Meditec, Jena, Germany), and funduscopy. Postoperatively, patients were examined the day after surgery as well as at 3 months (range, 2 to 4 months) after surgery of the second eye. The postoperative examination protocol was identical to the preoperative protocol, with additional evaluation of the UIVA and distance corrected intermediate visual acuity (DCIVA) at 66 cm, uncorrected near visual acuity (UNVA), and distance corrected near visual acuity (DCNVA) at 40 cm. The reading performance for near and intermediate distance was measured using the Salzburg Reading Desk (SRD) [8]. This device allows measurement of the reading acuity at near and intermediate distances in a predetermined or subjectively preferred reading position. In the current study, SRD (SRD Vision, New York, NY, USA) was used to test reading performance. It consists of a reading desk with a high-resolution monitor and a laptop computer that displays the operating software. Two video cameras continuously measure reading distance by stereo photometry. Reading speed and time are recorded with a microphone implemented into the SRD monitor. Log-scaled Colenbrander sentences are presented on the monitor in progressively smaller print sizes. A sentence is accepted if it can be read with a minimum speed of 80 words per minute (wpm). At the end of each reading period, the following parameters are visualized at the user interface: reading time in seconds, reading distance in cm, reading speed in wpm, reading acuity in log-MAR, inclination of the reading board in degrees, and smallest print size. Reading performance was evaluated considering a fixed prescribed distance at 40 and 80 cm, and a freely chosen reading distance. Furthermore, the smallest log-scaled print size that could be read effectively (>80 wpm) was assessed. All examinations were performed under standardized conditions at standard illumination of 500 lux according to the European norm DIN EN 12464-1. Patients were asked about their satisfaction with surgery results as well as about the perception of photic phenomena, such as glare or halos.
In all cases, the Haigis formula was used to calculate IOL power according to the measurements of corneal power, axial length, and anterior chamber depth obtained with the IOL Master v4.3 (Carl Zeiss Meditec) system. Target refraction was closest to emmetropia in all cases.
As described previously [7], the Lentis-313MF15 is a single-piece, aspheric, rotational asymmetric, refractive MIOL with an add power of 1.5 D on the lens plane. It has a 6.0-mm biconvex optic and overall length of 11.0 mm. Based on the same platform as the other LS-313 models [7910], it is a foldable hydrophilic acrylate IOL with hydrophobic surface properties [4]. The near add is +1.5 D. The 360° sharp optic edges reduce the risk of posterior capsule opacification. Moreover, the haptic design provides high rotational stability. The reduced add power was developed to increase intermediate visual acuity and decrease optical phenomena. Following the EN/ISO 11979-2 (ISO11979), the Lentis-313MF15 is considered a monofocal intraocular lens due to the low near add power in the IOL plane. Increased intermediate focus results in reduced near focus compared to other multifocal IOLs with higher add powers.
All surgeries were performed using a standard technique of sutureless 2.2-mm phacoemulsification. All incisions were made on the steep axis of the cornea. Topical anesthesia with 2% xylocain gel and mydriatic drops were instilled in all cases prior to the surgical procedure. After capsulorhexis creation with a forceps under cohesive ocular viscosurgical device protection, phacoemulsification and bimanual cortex peeling with capsule polishing was performed. The IOLs were inserted into the capsular bag using a VISCOJECT-BIO injector (Medicel, Wolfhalden, Switzerland) through the main incisions and constant balanced salt solution (Alcon, Fort Worth, TX, USA) irrigation. Postoperative therapy based on a combination of topical antibiotic and steroid was prescribed for application four times daily for 2 weeks.
SPSS ver. 15.0 (SPSS, Chicago, IL, USA) was used for statistical analysis. The Kolmogorov-Smirnov test was used to verify the normality of data distribution. When parametric analysis was possible, a Student's t-test for paired data was performed for all parameter comparisons between preoperative and postoperative examinations as well as between consecutive postoperative visits. When parametric analysis was not possible, the Mann-Whitney test was applied to assess the significance of differences between consecutive examinations. In all cases, the same level of significance (p < 0.05) was considered. The eye operated on first was chosen for statistical analysis and monocular comparison.
This study enrolled 60 eyes of 30 patients, of which 46% were male and 54% were female. The mean patient age was 68.30 ± 9.26 years (range, 34 to 80 years).
Preoperative measurements were mean axial length 23.448 ± 0.416 mm, mean anterior chamber depth 3.038 ± 0.497 mm, flattest meridian 7.759 ± 0.206 mm, and steepest meridian 7.667 ± 0.202 mm. Mean implanted IOL power was 20.038 ± 1.22 D.
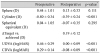
Table 1 and Fig. 1 show the refractive results in all patients over time. There were significant reductions in cylinder but not in sphere and spherical equivalent (SE). The postoperative SE was -0.07 ± 0.35 D, with a range of -1.0 to +0.625 D and 90% of patients with ±0.50 D. In the comparison between right eye and left eye, there was no statistical significant difference between refractive outcome (p = 0.857).
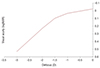
Table 1 and Fig. 1 show visual acuities. Mean UDVA increased to 0.00 logMAR with a CDVA of -0.08 logMAR. There was statistically significant improvement between preoperative and 3 months postoperative in UDVA (p <0.001) and CDVA (p <0.001). As expected with a near addition of +1.5 D at the IOL level, mean UNVA at 40 cm was 0.41 logMAR while mean UIVA at 80 cm was 0.01 logMAR. Fig. 2 shows the cumulative binocular visual acuity for UDVA and UIVA, with 100% reaching <0.2 logMAR. The defocus curve shows a wide range of functional visual acuity of greater than 0.3 logMAR over a range of more than 2 D (Fig. 3).
In the evaluation of reading acuity with SRD, similar results have been found (Tables 2 and 3, Figs. 4 and 5). Mean UIVA at 80 cm was 0.00 logMAR compared to subjective UIVA at 67.58 cm of -0.02 logMAR. Mean DCIVA at 80 cm was -0.02 logMAR compared to subjective DCIVA at 66.09 cm of -0.10 logMAR. There was no statistically significant difference between visual acuities, letter size, WPM, characters per minute, and reading time in set distances (near = 40 cm, intermediate = 80 cm) compared to the subjective distance that patients chose themselves (Tables 2 and 3, Figs. 4 and 5). For UNVA, UIVA, and DCIVA, the subjective chosen distance differed with statistical significance from the set distances (Tables 2 and 3).
In binocular functional vision analysis, mean binocular UNVA at 40 cm was 0.36 ± 0.14 logMAR compared to mean subjective UNVA of 0.29 ± 0.18 logMAR at 47 ± 9.22 cm. Mean binocular UIVA was -0.08 ± 0.03 logMAR compared to a mean subjective UIVA of -0.12 ± 0.03 logMAR at 68 ± 7.76 cm. Mean DCNVA at 40 cm was 0.32 ± 0.23 logMAR compared to mean subjective DCNVA of 0.29 ± 0.22 logMAR at 44 ± 1.73 cm. Mean binocular DCIVA was -0.12 ± 0.07 logMAR compared to mean subjective DCIVA of -0.12 ± 0.10 logMAR at 68 ± 4.10 cm.
Subjective questionnaires were used to investigate patient satisfaction after surgery. All patients answered that nighttime driving was possible without any complications. For intermediate tasks such as shopping and reading with computer distance <60 cm, only four patients needed additional spectacle support. For computer work performed at >60 cm, no patients required spectacles. Regarding satisfaction rate, use of the same IOL, and possible recommendation of this specific IOL, all patients were very satisfied without any exceptions and would pick the same IOL model again or recommend it to a friend or relative. None of the 30 patients reported halo or glare, even if asked directly.
Multifocal IOLs were designed to improve vision at different distances by increasing the field depth in the eye [11]. This approach differs depending on the particular IOL model. However, the principal goal is to provide the best levels of spectacle independence [12]. As intermediate focus has become more important for daily life activities, new optical designs try to fulfill those needs. Developments in optical designs have been made for refractive, diffractive, or combinations of both. One approach is to reduce the add power of MIOLs to shift the focal point closer to an intermediate direction, resulting in loss of spectacle dependency in the near and intermediate areas [1314]. More recently, accommodating IOL models are being tested and new technologies are being developed [7]. Another technical approach to define true intermediate vision has been the development of trifocal IOLs [2356151617]. The third focal point induced by a second diffractive structure also reduces the loss of light compared to other diffractive bifocal IOLs by offering true intermediate visual acuity [18]. The approach for reducing add power shows greater improvement in intermediate visual acuity by keeping functional vision in near distances <0.5 logMAR [1314]. This range of vision for near visual acuity is enough to read bigger print sizes, yet it is not possible to read regular small print, resulting in a need for reading aids.
To our knowledge, this is the first study to analyze functional vision regarding reading performance with the SRD after implantation of this IOL model. In the present study, there was improvement in UDVA and CDVA compared to preoperative values (Table 1). These results are consistent with the refractive values obtained. All values were within the interval of -1.0 to +1.0 D SE 3 months after surgery. The UDVA results were notable, with a mean value of 0.00 monocular (Table 1 and Fig. 1). The near add of +1.5 D offers good results for intermediate vision with monocular UIVA of 0.01 and near functional visual acuity with monocular UNVA of 0.41. These results concurred with those of SRD in the same distance measured with Early Treatment Diabetic Retinopathy Study (ETDRS)-charts, as well as with the subjective chosen distances (Tables 2 and 3, Figs. 4 and 5).
Alio et al. [7] have published the only report of this type of MIOL. Here, intermediate visual acuity was not an outcome parameter. In fact, better results were achieved for UDVA with a mean value of 0.00 logMAR compared to 0.22 logMAR, CDVA with a mean value of -0.08 logMAR compared to 0.10 logMAR, and UNVA with a mean value of 0.41 logMAR compared to 0.44 logMAR [7]. Venter et al. [19] performed the largest study of the rotational asymmetric Lentis-313MF30 based on the same lens platform. The UDVA in our study concurred with their 3-month outcomes. As expected with a reduced near addition of +1.5 D, the UNVA in our study was less than those of other studies with LS-313MF30 and its +3.0 D add power [91019]. Still, the results for intermediate visual acuity with LS313-MF15 are remarkably better compared to the same MIOL platform with 3.0 D near addition.
In a recent study of a trifocal MIOL model (AT LISA tri 839MP, Carl Zeiss Meditec), Mojzis et al. [4] reported mean monocular UDVA and CDVA of -0.04 ± 0.10 and -0.06 ± 0.09, respectively, which are similar to our results with the asymmetric low-add MIOL (Table 1). Comparing results for intermediate visual acuity, the AT LISA tri had slightly worse performance with UIVA and DCIVA of 0.11 ± 0.10 and 0.10 ± 0.09, respectively [4], compared to our results. The lack of a true near distance with the LS-313MF15 shows reduced near visual function compared to the AT LISA tri.
Gundersen and Potvin [20] compared the visual function of a monofocal IOL and two MIOLs with a near add of +2.5 and +3.0 D. Although they used a different setup to measure the preferred distances, they clearly demonstrated that the best intermediate distance for a +2.5 add MIOL is at approximately 60 cm, while the near visual function is reduced compared to a +3.0 D MIOL. Our data shows that the preferred intermediate distance for a +1.5 D MIOL is at approximately 66.0 to 67.00 cm (Table 3). By comparing the preferred reading distances, Gunderson and Potvin [20] found a preferred near distance of around 55 cm for the +2.5 D add MIOL and 43 cm for the +3.0 add MIOL. Although the LS-313MF15 does not provide a true near focus, the preferred reading distance in our study was 46.76 cm for UNVA a nd 43.18 c m for DCNVA, offering a visual acuity of 0.336 and 0.316 logMAR, respectively (Table 3).
Comparisons of different multifocal IOL designs or the same IOL type should be performed cautiously because of differences in measuring visual acuity for near and intermediate distances. In most studies, conventional single character reading charts (Snellen, Jaeger, Zeiss, and ETDRS) are used to assess reading visual acuity. For detailed testing of reading performance, modern log-scaled reading charts have been introduced to measure reading acuity, reading speed, and critical character size [21]. It is important to evaluate near and intermediate function after multifocal IOL implantation because these are the leading predictors o f d aily a ctivity tasks, such a s reading a nd computer work. One standardized tool for measuring reading performance, using sentences instead of single optotypes, is the SRD [8]. This device reflects the physiological reading process by considering reading speed, reading distance, and smallest print size that can be effectively read.
In the literature, there are only a few publications analyzing the reading performance of different multifocal IOLs with SRD. Alio et al. [22] compared the bilateral reading performance of four intraocular lens models (monofocal, apodized multifocal, diffractive multifocal, and refractive multifocal) in terms of reading acuity, reading speed, and distance. Multifocal IOLs with diffractive optical design provided better near visual performance than monofocal and refractive multifocal IOLs [22]. Rasp et al. [23] found similar results in a prospective randomized clinical trial comparing five different IOL. We did not find any publications evaluating the reading performance of a zonal refractive asymmetric multifocal IOL with reduced near addition of +1.5 D. Mean monocular uncorrected near reading acuity of 0.336 logMAR was observed at a predefined reading distance of 46.761 cm. The best results for monocular and binocular uncorrected and distance corrected reading acuity are achieved at an individual preferred reading distance of 43 to 47 cm (Tables 2 and 3, Figs. 4 and 5). Regarding intermediate reading acuity, the situation is quite different. The IOL performed well for intermediate vision, with mean monocular UIVA of 0.00 logMAR at a f ixed distance of 80 cm. After choosing a subjectively convenient intermediate distance, the monocular uncorrected intermediate acuity increased to -0.02 logMAR with WPM increasing from 94.456 to 96.375. The subjective preferred uncorrected and corrected intermediate distances were between 66 and 68 cm (Table 3). However, there were no significant differences in terms of monocular or binocular uncorrected and corrected intermediate reading acuity and reading speed between the predefined distance of 80 cm and the individually preferred distance. This finding is explained by the fact that reading acuity is dependent on reading distance and speed. When diminishing the reading distance from 80 to 67 cm, visual acuity can decrease or remain stable.
A limitation of our study is the small amount of subjects included. This study was also non-comparative and not randomized, and the results show the expected effect on intermediate visual acuity with a +1.5 D add power. Further prospective studies comparing the results of this type of IOL to a monovision approach would be helpful to identifying more individual parameters to treat presbyopia.
The results of the current study indicate the importance of testing reading and intermediate performance at a subjectively convenient reading distance.
In conclusion, the LS-313MF15 IOL successfully restored distance and intermediate visual function after cataract surgery and refractive lens exchange. Even bifocal IOLs provide functional results for reading performance at near distances. Our results also indicate that the following four parameters are necessary for standardized evaluation of reading performance: reading acuity, reading speed, reading distance, and smallest readable print size. Standardization of reading performance is important for future studies to effectively compare different types of multifocal IOLs after presbyopic correction.
Figures and Tables
 | Fig. 1Postoperative visual acuities. UDVA = uncorrected distance visual acuity; CDVA = corrected distance visual acuity; UNVA = uncorrected near visual acuity; DCNVA = distance corrected near visual acuity; UIVA = uncorrected intermediate visual acuity; DCIVA = distance corrected intermediate visual acuity. |
 | Fig. 2Cumulative binocular visual acuity for distance and intermediate. UDVA = uncorrected distance visual acuity; logMAR = logarithm of the minimum angle of resolution; UIVA = uncorrected intermediate visual acuity. |
 | Fig. 4Uncorrected visual acuity for near and intermediate distance evaluated with Salzburg Reading Desk. logMAR = logarithm of the minimum angle of resolution; sc = sine correctione (unccoreccted). |
 | Fig. 5Distance corrected visual acuity for near and intermediate distance evaluated with Salzburg Reading Desk. logMAR = logarithm of the minimum angle of resolution; dc = distance corrected. |
Acknowledgements
The David J Apple International Laboratory for Ocular Pathology received research grants from the Klaus Tschira Foundation.
References
1. Olsen T, Funding M. Ray-tracing analysis of intraocular lens power in situ. J Cataract Refract Surg. 2012; 38:641–647.
2. Cochener B, Vryghem J, Rozot P, et al. Visual and refractive outcomes after implantation of a fully diffractive trifocal lens. Clin Ophthalmol. 2012; 6:1421–1427.
3. Gatinel D, Houbrechts Y. Comparison of bifocal and trifocal diffractive and refractive intraocular lenses using an optical bench. J Cataract Refract Surg. 2013; 39:1093–1099.
4. Mojzis P, Pena-Garcia P, Liehneova I, et al. Outcomes of a new diffractive trifocal intraocular lens. J Cataract Refract Surg. 2014; 40:60–69.
5. Sheppard AL, Shah S, Bhatt U, et al. Visual outcomes and subjective experience after bilateral implantation of a new diffractive trifocal intraocular lens. J Cataract Refract Surg. 2013; 39:343–349.
6. Voskresenskaya A, Pozdeyeva N, Pashtaev N, et al. Initial results of trifocal diffractive IOL implantation. Graefes Arch Clin Exp Ophthalmol. 2010; 248:1299–1306.
7. Alio JL, Plaza-Puche AB, Montalban R, Javaloy J. Visual outcomes with a single-optic accommodating intraocular lens and a low-addition-power rotational asymmetric multifocal intraocular lens. J Cataract Refract Surg. 2012; 38:978–985.
8. Dexl AK, Schlogel H, Wolfbauer M, Grabner G. Device for improving quantification of reading acuity and reading speed. J Refract Surg. 2010; 26:682–688.
9. Khoramnia R, Auffarth GU, Rabsilber TM, Holzer MP. Implantation of a multifocal toric intraocular lens with a surface-embedded near segment after repeated LASIK treatments. J Cataract Refract Surg. 2012; 38:2049–2052.
10. Thomas BC, Auffarth GU, Philips R, et al. Clinical results after implantation of a new segmental refractive multifocal intraocular lens. Ophthalmologe. 2013; 110:1058–1062.
11. Bellucci R. Multifocal intraocular lenses. Curr Opin Ophthalmol. 2005; 16:33–37.
12. Toto L, Falconio G, Vecchiarino L, et al. Visual performance and biocompatibility of 2 multifocal diffractive IOLs: six-month comparative study. J Cataract Refract Surg. 2007; 33:1419–1425.
13. Kretz FT, Gerl M, Gerl R, et al. Clinical evaluation of a new pupil independent diffractive multifocal intraocular lens with a +2.75 D near addition: a European multicentre study. Br J Ophthalmol. 2015; 99:1655–1659.
14. Kretz FT, Koss MJ, Auffarth GU. ZLB00 Study Group. Intermediate and near visual acuity of an aspheric, bifocal, diffractive multifocal intraocular lens with +3.25 D near addition. J Refract Surg. 2015; 31:295–299.
15. Lesieur G. Outcomes after implantation of a trifocal diffractive IOL. J Fr Ophtalmol. 2012; 35:338–342.
16. Lichtinger A, Rootman DS. Intraocular lenses for presbyopia correction: past, present, and future. Curr Opin Ophthalmol. 2012; 23:40–46.
17. Kretz FT, Attia MA, Linz K, Auffarth GU. Level of binocular pseudoaccommodation in patients implanted with an apodised, diffractive and trifocal multifocal intraocular lens. Klin Monbl Augenheilkd. 2015; 232:947–952.
18. Gatinel D, Pagnoulle C, Houbrechts Y, Gobin L. Design and qualification of a diffractive trifocal optical profile for intraocular lenses. J Cataract Refract Surg. 2011; 37:2060–2067.
19. Venter JA, Pelouskova M, Collins BM, et al. Visual outcomes and patient satisfaction in 9366 eyes using a refractive segmented multifocal intraocular lens. J Cataract Refract Surg. 2013; 39:1477–1484.
20. Gundersen KG, Potvin R. Comparative visual performance with monofocal and multifocal intraocular lenses. Clin Ophthalmol. 2013; 7:1979–1985.
21. Radner W, Obermayer W, Richter-Mueksch S, et al. The validity and reliability of short German sentences for measuring reading speed. Graefes Arch Clin Exp Ophthalmol. 2002; 240:461–467.
22. Alio JL, Grabner G, Plaza-Puche AB, et al. Postoperative bilateral reading performance with 4 intraocular lens models: six-month results. J Cataract Refract Surg. 2011; 37:842–852.
23. Rasp M, Bachernegg A, Seyeddain O, et al. Bilateral reading performance of 4 multifocal intraocular lens models and a monofocal intraocular lens under bright lighting conditions. J Cataract Refract Surg. 2012; 38:1950–1961.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download