Abstract
Purpose
To evaluate visual outcomes following implantation of a trifocal diffractive intraocular lens (IOL) and to analyze their correlation with patient satisfaction and ease of performing daily tasks.
Methods
This was a prospective study enrolling 100 eyes of 50 patients undergoing cataract surgery with implantation of trifocal IOL AT LISA tri 839MP. Visual and refractive outcomes were evaluated during a 3-month follow-up. Postoperatively, a questionnaire was used to evaluate patient satisfaction with regard to surgical outcome, spectacle independence, perception of photic phenomena, and ease of performing some vision-related activities.
Results
A total of 91%, 87%, and 79% of eyes achieved a monocular uncorrected distance, near, and intermediate visual acuity of 0.1 logarithm of the minimum angle of resolution or better, respectively. After the surgery, 96% of the patients could perform their daily activities without problems. The mean spectacle independence scores for reading, doing computer work, and for distance were 10.33 ± 12.47, 5.71 ± 11.90, and 3.92 ± 9.77, respectively (scale: 0 = no spectacles needed; 40 = spectacles always needed). No correlation was found between spectacle independence and visual outcome (-0.101 ≤ r ≤ 0.244, p ≥ 0.087). Mean scores (0 = no symptoms; 40 = strong symptoms) for glare at night, ghost images, and halos were 15.15 ± 12.02, 4.49 ± 7.92, and 13.34 ± 10.82, respectively. No correlation was found between photic phenomena and visual outcome (-0.199 ≤ r ≤ 0.209, p ≥ 0.150). A total of 80% of patients reported satisfaction with the surgery outcome, and 86% would recommend the surgery to friends and family.
Trifocal diffractive intraocular lenses (IOLs) distribute light to distant, intermediate, and near foci without a clinically significant deterioration in visual quality [12]. Consequently, trifocal IOLs provide significantly better intermediate vision compared to conventional bifocal diffractive IOLs [3]. One of the currently available trifocal IOLs is the AT LISA tri 839MP IOL from Carl Zeiss Meditec (Jena, Germany), which combines a central 4.3-mm trifocal area with a bifocal diffractive surface between 4.3 and 6 mm in diameter [4]. Previous studies have demonstrated that this IOL is able to provide good visual contrast sensitivity and optical quality outcomes [3456]. Likewise, Law et al. [6] evaluated a sample of 60 eyes of 30 patients implanted with the AT LISA tri 839MP IOL to determine the level of patient satisfaction with regard to surgical out-come and the impact of the surgery on daily vision-related activities. These authors found that 76.7% of patients were entirely satisfied with the visual outcome and had no difficulties in watching TV or driving 6 months after surgery [6]. Moderate difficulties were reported by a limited percentage of patients in this same study for performing some near and intermediate vision tasks, such as reading the newspaper or working on the computer [6]. Multifocal IOLs have been demonstrated to have an impact on patient quality of life, and this impact has been shown to depend on visual outcome [78]. The current study aimed to investigate the correlations between visual outcome obtained with the trifocal diffractive IOL AT LISA tri 839MP and patient satisfaction, spectacle independence, and ease in performing vision-related tasks.
In this prospective study, 100 eyes of 50 patients were enrolled. The included patients had cataract or presbyopia/pre-presbyopia suitable for refractive lens exchange and were seeking spectacle independence. Excluded were patients had a history of glaucoma or retinal detachment, corneal disease, irregular corneal astigmatism, abnormal iris, macular degeneration or retinopathy, neurophthalmic disease, history of ocular inflammation, or previous ocular surgery or corneal astigmatism of 1.25 diopter (D) or greater. In all cases, bilateral cataract surgery was performed with implantation of the trifocal IOL AT LISA tri 839MP (Carl Zeiss Meditec). All patients were adequately informed about the study and signed a consent form. The study adhered to the tenets of the Declaration of Helsinki and was approved by the local ethics committee.
A complete preoperative ophthalmological examination was performed, including manifest refraction, keratometry, monocular uncorrected distance visual acuity (UDVA) and corrected distance visual acuity (CDVA), Goldmann applanation tonometry, slit lamp examination, corneal topography, biometry (IOL Master v.4.3, Carl Zeiss Meditec), and funduscopy. In all cases, the SRK-T formula was used to calculate the IOL power for implantation based on measurements of corneal power, axial length (AL), and anterior chamber depth, obtained with the IOL Master system. Target refraction was emmetropia in all cases.
Patients were examined the day after surgery and at 1 and 3 months after surgery. At 3 months postoperatively, the examination protocol was identical to the preoperative protocol with the additional evaluation of binocular UDVA, monocular and binocular uncorrected intermediate visual acuity (UIVA) (66 cm), and monocular and binocular uncorrected near visual acuity (UNVA) (40 cm). In addition, all patients completed a self-developed questionnaire including questions about the level of patient satisfaction with regard to surgical outcome, level of spectacle independence, and difficulty performing vision-related activities after surgery. Specifically, patients were asked about difficulty performing the following activities (scale: 1 = no difficulty; 2 = moderately difficult; 3 = difficult; and 4 = unable to perform): reading the newspaper, reading a book, watching TV, driving a car during the day, driving a car at night, shopping, doing computer work, working in the house or garden, and doing handicraft work. In addition, patients were asked about the intensity of the following symptoms using a scale from 0 (not at all) to 40 (very strong): glare during the day; glare at night; ocular burning or pain; halos; ghost images; visual problems under bright, normal, and low light conditions; irritation from halos in traffic situations; and irritation from halos during daily activities. The spectacle independence scores for reading, doing computer work, and for distance were also evaluated on a 0 to 40 scale (not at all/complete dependence). Finally, the following questions about satisfaction with the surgery were asked: "Have you been able to perform your daily activities since surgery?" (yes/partly/no), "Are you happy with the outcome of the surgery?" (yes/partly/no), "Would you choose the same IOL model again?" (yes/no), "Were you able to complete this questionnaire without glasses?" (yes/no), and "Would you recommend the surgery and IOL?" (yes/no).
Experienced surgeons performed all surgeries using a standard, sutureless, micro-coaxial 2.2-mm phacoemulsification technique. All incisions were made at the steep axis of the cornea. Topical anesthesia and mydriatic drops were instilled prior to the surgical procedure in all cases. After capsulorrhexis creation and phacoemulsification, the IOLs were inserted into the capsular bag through the main incision using the BLUEMIXS 180 injector (Carl Zeiss Meditec). A postoperative topical therapy of combined antibiotic and steroid (tobramycin 0.3%, dexamethasone 0,1%; Tobradex, Alcon, Fort Worth, TX, USA) was prescribed to be applied four times daily for 1 week.
SPSS ver. 15.0.1 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. The Kolmogorov-Smirnov test was used to determine the normality of the data distribution. When parametric analysis was possible, Student's t-test for paired data was performed for all parameter comparisons between preoperative and postoperative examinations, and Student's t-test for unpaired data was performed for comparisons between independent groups. When parametric analysis was not possible, the Wilcoxon rank sum test was applied to assess the differences between consecutive examinations, and the Mann-Whitney test was used to evaluate differences between independent groups. The correlations between different clinical variables were investigated with the Pearson or Spearman correlation coefficient depending on whether the normality condition could be assumed. In all cases, a p-value <0.05 was considered statistically significant. The chi-square test was used to assess differences in categorical variables.
The study enrolled a total of 100 eyes of 50 patients with a mean age of 57.5 years. The mean preoperative AL was 23.92 mm, ranging from 21.43 to 28.59 mm, and the mean preoperative anterior chamber depth was 3.24 mm, ranging from 2.28 to 3.95 mm. The mean preoperative flattest (K1) and steepest (K2) corneal radii of curvature were 7.91 mm (range, 7.30 to 9.11 mm) and 7.75 mm (range, 7.12 to 8.94 mm), respectively. The mean IOL power was 21.3 D and ranged from 5 to 29 D. During the follow-up period, no significant posterior capsule opacification was detected.
Table 1 summarizes the preoperative and postoperative visual and refractive data obtained from our study sample. As shown, significant improvement was observed in monocular logarithm of the minimum angle of resolution (logMAR) UDVA and CDVA (p < 0.001). Likewise, significant change was observed in manifest sphere (p < 0.001) and cylinder (p = 0.001) after surgery. A total of 86% and 99% of eyes had postoperative spherical equivalents within 0.50 and 1.00 D of emmetropia, respectively.
Fig. 1 displays the distribution of postoperative monocular and binocular uncorrected, intermediate and near distance visual outcomes in the analyzed sample. As shown, a total of 91%, 87%, and 79% of eyes had monocular UDVA, UNVA, and UIVA of 0.1 logMAR or better, respectively. Likewise, a total of 99%, 99% and 94% of eyes achieved UDVA, UNVA, and UIVA of 0.20 logMAR or better, respectively (Fig. 1). As expected, binocular values of UDVA (p = 0.036), UNVA (p < 0.001), and UIVA (p = 0.001) were significantly better when measured under binocular conditions compared to monocular conditions.
No significant correlation was found between IOL power and postoperative spherical equivalent (r = 0.131, p = 0.193). There were no significant correlations between postoperative spherical equivalent and AL (r = 0.148, p = 0.141), K1 (r = -0.066, p = 0.514), K2 (r = 0.014, p = 0.887), or anterior chamber depth (r = 0.147, p = 0.144). In contrast, a statistically significant correlation was found between binocular UDVA and UIVA (r = 0.635, p < 0.001) (Fig. 2), as well as between binocular UIVA and UNVA (r = 0.453, p = 0.001). Preoperative spherical equivalent did not correlate significantly with any measures of uncorrected postoperative visual acuity (UDVA: r = 0.169, p = 0.094; UIVA: r = 0.126, p = 0.210; UNVA: r = -0.027, p = 0.793). Likewise, no significant correlation was found between preoperative and postoperative spherical equivalents (r = -0.171, p = 0.089). Furthermore, no significant correlations were found between postoperative spherical equivalent and visual outcomes at different distances (UDVA: r = -0.155, p = 0.100; UIVA: r = -0.101, p = 0.317; UNVA: r = 0.156, p = 0.122).
Concerning the level of impact of residual astigmatism on vision, postoperative manifest cylinder did not correlate significantly with postoperative monocular UDVA (r = -0.058, p = 0.575), UIVA (r = 0.056, p = 0.590), or UNVA (r = 0.104, p = 0.312). It should be noted that only four eyes (4%) showed a postoperative cylinder greater than 1 D. Preoperative cylinder showed a poor but significant correlation with monocular postoperative UNVA (r = -0.224, p = 0.037), and it showed a correlation with monocular postoperative at the limit of statistical significance UIVA (r = -0.206, p = 0.05). No significant correlation was found between preoperative cylinder and postoperative monocular UDVA (r = -0.102, p = 0.348).
After surgery, a total of 96% of patients were able to perform their daily activities without any problems. Only two patients (4%) reported that they could only partly perform their daily activities following surgery. Fig. 3 shows the distribution of the answers when patients were asked about difficulty in performing daily activities. No statistically significant differences in binocular logMAR UNVA were found between patients reporting no difficulty or partial difficulty in reading a newspaper (p = 0.290), reading a book (p = 0.755), doing computer work (p = 0.084), or doing handicraft work (p = 0.385). A difference near the limit for statistical significance was found in binocular logMAR UIVA between patients reporting no difficulty or partial difficulty in doing computer work (0.01 ± 0.07 vs. 0.06 ± 0.08, p = 0.060). No statistically significant difference in binocular logMAR UDVA was found between patients reporting no difficulty or partial difficulty in driving at night ( p = 0.346). When the results were compared based on preoperative refractive status, no statistically significant differences were found with regard to the difficulty levels of performing daily activities evaluated among myopes and hyperopes (p ≥ 0.299).
Mean spectacle independence scores (range, 0 to 40) for reading, doing computer work, and for distance were 10.33 ± 12.47, 5.71 ± 11.90, and 3.92 ± 9.77, respectively. Binocular UDVA did not correlate significantly with spectacle independence score for reading (r = -0.073, p = 0.619), doing computer work (r = 0.097, p = 0.505), or for distance (r = -0.101, p = 0.484). A similar finding was obtained for binocular UIVA (reading: r = 0.172, p = 0.237; computer work: r = 0.244, p = 0.091; distance: r = 0.016, p = 0.910) and UNVA (reading: r = 0.005, p = 0.974; computer work: r = 0.247, p = 0.087; distance: r = 0.084, p = 0.561). A total of 43 patients (86%) were able to complete the questionnaire without the use of any additional optical correction. No significant differences among myopes and hyperopes were found in the levels of spectacle independence for reading (p = 0.597), doing computer work (p = 0.947), or for distance (p = 0.265).
The mean intensity scores were: for glare during the day 10.15 ± 9.08 (range, 0 to 30), glare at night 15.15 ± 12.02 (range, 1 to 39), ocular burning or pain 6.51 ± 9.28 (range, 0 to 37), halos 13.34 ± 10.82 (range, 0 to 37), ghost images 4.49 ± 7.92 (range, 0 to 36), visual problems under bright light 10.34 ± 10.36 (range, 0 to 37), visual problems under normal light 4.88 ± 7.73 (range, 0 to 30), visual problems under dim light 13.90 ± 10.58 (range, 0 to 39), irritation from halos in traffic 12.32 ± 11.21 (range, 0 to 39), and irritation from halos during daily activities 7.24 ± 8.69 (range, 0 to 35), respectively. No significant correlations between binocular UDVA and the subjective grades of evaluated disturbances were found (glare during the day: r = 0.037, p = 0.803; glare at night: r = 0.008, p = 0.957; ocular burning or pain: r = -0.022, p = 0.882; halos: r = -0.109, p = 0.166; ghost images: r = -0.199, p = 0.166; visual problems under bright light: r = -0.133, p = 0.359; visual problems under normal light: r = 0.003, p = 0.981; visual problems under dim light: r = -0.113, p = 0.433; irritation from halos in traffic: r = 0.097, p = 0.518; irritation from halos during daily activities: r = -0.191, p = 0.203). Likewise, binocular UIVA (glare during the day: r = 0.045, p = 0.760; glare at night: r = 0.108, p = 0.469; ocular burning or pain: r = 0.030, p = 0.837; halos: r = -0.013, p = 0.930; ghost images: r = -0.169, p = 0.241; visual problems under bright light: r = -0.003, p = 0.984; visual problems under normal light: r = 0.113, p = 0.435; visual problems under dim light: r = -0.133, p = 0.356; irritation from halos in traffic: r = 0.108, p = 0.472; irritation from halos during daily activities: r = 0.040, p = 0.790) and UNVA (glare during the day: r = 0.182, p = 0.211; glare at night: r = 0.083, p = 0.579; ocular burning or pain: r = -0.043, p = 0.770; halos: r = 0.209, p = 0.150; ghost images: r = -0.141, p = 0.328; visual problems under bright light: r = 0.046, p = 0.749; visual problems under normal light: r = 0.128, p = 0.374; visual problems under dim light: r = -0.022, p = 0.881; irritation from halos in traffic: r = 0.083, p = 0.578; irritation from halos during daily activities: r = 0.145, p = 0.337) did not correlate with the subjective grade of evaluated symptoms. No significant postoperative differences in the levels of the different photic phenomena were found between myopes and hyperopes (p ≥ 0.073).
A total of 80% of patients reported to be completely happy with the surgical outcome, and 16% reported to be moderately happy. Only two patients (4%) reported to be unhappy with the results of cataract surgery. A total of 44 patients (88%) would choose the same IOL again, and 43 patients (86%) would recommend the surgery and IOL. No significant differences between myopic and hyperopic patients were found with regard to patient satisfaction with the surgery (p = 0.120).
The trifocal IOL evaluated in the current study combines a bifocal and trifocal diffractive pattern on the anterior surface of the lens in order to provide an asymmetrical light distribution generating distant, intermediate, and near foci [3456]. Several studies have confirmed the good performance of this IOL in terms of visual and refractive outcomes [3456], but there is still limited evidence on the impact of this multifocal IOL on patient satisfaction, spectacle independence, and patient ability to perform common daily activities, such as reading or driving. For this reason, this study has evaluated these aspects by means of a self-developed questionnaire and evaluation of visual and refractive outcomes.
In our sample, mean monocular postoperative logMAR UDVA ranged from -0.10 to 0.30, with a mean value of 0.06. This confirms the efficacy of the evaluated IOL in successfully restoring distant vision after lensectomy. Likewise, an excellent binocular logMAR UDVA was found in our sample, with a mean value of 0.04 and a range from -0.10 to 0.20. Our results are consistent with those reported by most authors evaluating the same and other trifocal IOLs [34569101112131415]. Table 2 summarizes the visual and refractive outcomes reported by other authors evaluating trifocal IOLs and other types of multifocal IOLs [34671011121315161718192021222324]. Somewhat worse UDVA outcomes have been reported by Alio et al. [10] and Sheppard et al. [11] and for trifocal IOLs that combine two bifocal diffractive patterns (FineVision IOL from PhysIOL). The studies reported mean postoperative logMAR UDVA values of 0.19 ± 0.09 and 0.18 ± 0.13, respectively. Differences in sample size, patient characteristics, follow-up, and visual acuity testing can explain the differences between the same types of IOL. Voskresenskaya et al. [15] also reported slightly worse postoperative UDVA outcomes with another trifocal IOL model (mean, 0.13) compared to those obtained in our series (Table 2). In comparison with other types of diffractive multifocal IOLs, our results were either comparable [16171819202122] or better (Table 2) [23]. When our results were compared to those obtained with other refractive multifocal IOLs, the superiority of the evaluated diffractive IOL was obvious [71824]. This can be easily explained by the greater amount of higher-order aberrations induced by refractive multifocal IOLs compared to diffractive models [724]. Specifically, rotationally asymmetric refractive multifocal IOLs are known to induce significant amounts of primary coma, which can limit the visual acuity achieved with the implant [724].
The good uncorrected visual outcome found in our series was consistent with the significant changes in magnitude of the manifest refraction components. A mean postoperative spherical equivalent of +0.08 D (range, -1.38 to +0.75 D) was found in our series, which is similar to values reported by other authors evaluating the same trifocal IOL [3456] and other trifocal [9121314] and multifocal IOLs (Table 2) [1623]. In contrast, a myopic residual refractive error trend was reported with the trifocal MIOL-Record, which exhibited a mean postoperative spherical equivalent of -0.41 ± 0.49 D [15]. This might be due to the use of a non-optimized A-constant for this specific type of trifocal IOL or to the selection of an inadequate refractive target. It should be noted that some residual myopia is intended when monofocal IOLs are implanted; however, this does not apply to trifocal IOLs, which are very susceptible to minimal residual refractive error. In our sample, a significant correlation was found between binocular postoperative UDVA and UIVA and also between UIVA and UNVA. Specifically, the worse was the postoperative binocular UDVA, the worse was the postoperative binocular UIVA, and vice versa. This confirms that the presence of residual refractive error significantly contributes to simultaneous degradation of distant, intermediate, and near visual foci. Furthermore, a trend of worse near visual outcome in cases of higher preoperative astigmatism was found, which confirms the need for a toric trifocal IOL in such cases.
The near visual outcomes obtained in our series were excellent, with 87% of eyes achieving a logMAR UNVA of 0.1 or better, 99% of eyes achieving 0.2 or better, and all eyes achieving 0.3 or better. The mean postoperative logMAR UNVA was 0.06 when measured at 40 cm. This result is equivalent to that reported by Mojzis et al. [4] with the same type of trifocal IOL (0.07 ± 0.09 measured at 33 cm) and slightly better than the UNVA outcome reported by the same authors in another study [3] (0.20 ± 0.12 measured at 33 cm) and by Law et al. [6] (0.16 ± 0.07 binocularly measured at 40 cm). Several factors might account for this discrepancy, such as differences in patient samples (e.g., age, AL), surgical procedure, or examination protocol. The results of various authors evaluating the FineVision IOL also showed some discrepancies with regard to UNVA outcome. Mean logMAR values of 0.00 ± 0.04 (measured at 35 cm), 0.26 ± 0.15 (measured at 40 cm), 0.11 ± 0.12 (measured at 35 cm), and 0.01 ± 0.06 (measured at 35 cm) have been reported by Cochener et al. [9], Alio et al. [10], Vryghem and Heireman [12], and Cochener et al. [13], respectively. As previously stated, this variability in evaluation of the same type of IOL might be attributed to discrepancies in clinical protocol and sample selection. In any case, all reported mean values showed that trifocal IOLs are a good option for restoration of near visual function after cataract surgery. With the binary in phase trifocal IOL MIOL-Record, a mean logMAR UNVA of 0.07 was measured at the patient's preferred distance [15]. In comparison with bifocal diffractive IOLs, the evaluated trifocal IOL provides similar near visual outcomes (Table 2) [1617181920212223]. In contrast, worse UNVA outcomes have been reported with rotationally asymmetric refractive multifocal IOLs [724]. Ramon et al. [7] and Alio et al. [24] reported mean UNVA values of 0.19 ± 0.42 (measured at 40 cm) and 0.30 ± 0.21 (measured at 40 cm), respectively. As shown for distant visual outcomes, the increase in higher-order aberrations with the Mplus IOL limits the near visual acuity that can be achieved [724].
The intermediate visual outcomes obtained in our series were also very good, with 79% of eyes achieving a logMAR UIVA of 0.1 or better, 94% of eyes achieving 0.2 or better, and all eyes achieving 0.3 or better. The mean postoperative logMAR UIVA was 0.09 when measured at 66 cm. Similar UIVA outcomes have been reported by other authors for the same trifocal IOL [3456] and for other types of trifocal IOLs (Table 1) [9121314]. Only a slightly worse mean UIVA (0.20 ± 0.11, measured at 80 cm) was obtained in the study by Alio et al. [10]. As previously stated, differences in sample size, patient characteristics, follow-up, and visual acuity testing might have contributed to this discrepancy. In a comparative study of the bifocal and trifocal AT LISA IOLs conducted by Mojzis et al. [3], a significantly better UIVA was obtained in the group of eyes implanted with the trifocal IOL (bifocal 0.24 ± 0.16 vs. 0.03 ± 0.08, 80 cm, p < 0.01). With regard to the binary in phase trifocal MIOL-Record, a poorer UIVA was reported by Voskresenskaya et al. [15] (mean value of approximately 0.20 logMAR measured at 50 cm) when compared to the FineVision and AT LISA trifocal IOLs. As expected, the outcomes reported by different authors evaluating diffractive bifocal IOLs were more limited than those obtained by our research group for the AT LISA trifocal IOL and by other authors for the FineVision and AT LISA trifocal IOLs [320212223].
The level of spectacle independence achieved with implantation of the evaluated trifocal IOL was high, exhibiting low mean spectacle dependence scores. Specifically, the mean spectacle independence scores for reading, doing computer work, and for distance were 10.33 ± 12.47, 5.71 ± 11.90, and 3.92 ± 9.77, respectively. This result is consistent with that obtained by Sheppard et al. [11] using the Near Activity Visual Questionnaire to assess patient satisfaction with uncorrected near vision after cataract surgery and implantation of the trifocal IOL FineVision. The authors found that a good mean Near Activity Visual Questionnaire Rasch score for near vision satisfaction (15.9 ± 10.7 logits) [11]. In our series, no correlation was found between level of spectacle independence and binocular distant, intermediate, or near visual outcome. This can be easily explained, as most patients achieved binocular UDVA, UNVA, and UIVA close to 0.00 logMAR with a lack of significant residual refractive errors. This confirms the excellent performance of the trifocal IOL in terms of visual rehabilitation. Indeed, most patients reported no difficulty in performing tasks such as reading a newspaper, reading a book, driving a car at night, doing computer work, or doing handicraft work. Law et al. [6] used a self-developed questionnaire to evaluate the level of difficulty in performing vision-related tasks after cataract surgery with implantation of the same trifocal IOL that was evaluated in our series. They found no patients reporting difficulties in watching TV or driving [6]. Likewise, as in our study, moderate difficulty was reported by a limited percentage of patients for performing some near and intermediate visual tasks, such as reading the newspaper or working with the computer [6]. In our series, 96% of postoperative patients were able to perform their daily activities without any problems, and only two patients reported partial ability in performing their daily activities. As can be expected, a non-significant trend of a more limited binocular UIVA was found in patients reporting partial difficulty in doing computer work. According to these findings, the evaluated trifocal IOL has a positive impact on vision-related daily activities and allows them to be performed with minimal or no difficulty. Alio et al. [8] concluded in a comparative study that patients with bifocal full diffractive IOLs were able to better perform several daily tasks at near and intermediate distances compared to patients with apodized multifocal or monofocal IOLs.
Patients also graded the levels of photic phenomena using a subjective scale ranging from 0 (not at all) to 40 (very strong). Mean scores between 5 and 15 were obtained for glare during day, glare at night, halos, ghost images, bothersome halos in traffic, and bothersome halos during the day. This confirms a low occurrence of such potentially disabling disturbances. Furthermore, the perceptions of photic phenomena or visual disturbances did not correlate with binocular distant, intermediate, or near visual outcome. This seems logical, as the presence of photic phenomena with diffractive multifocal IOLs seems to be related to the diffractive component rather than residual refractive error. According to theoretical simulations, a double-halo formation due to two non-focused powers can be expected with the trifocal IOL evaluated in the current study [25]. Law et al. [6] found that the halos associated with this IOL were well-tolerated, and their perception was reduced over time. Therefore, difficulties associated with perception decreased from 80% at 1 month to 40% at 6 months after IOL implantation. These authors also confirmed gradual reduction in the difficulties associated with glare perception. The percentage of patients experiencing these difficulties decreased from 73.3% at 1 month to 13.3% at 6 months after surgery [6]. Vryghem and Heireman [12] investigated the rate of halo perception after implantation of the FineVision trifocal IOL and concluded that 68% of patients did not perceive them as significant or disabling. Sheppard et al. [11] used halometry to measure the angular sizes of monocular and binocular photopic scotomas arising from a glare source after FineVision trifocal IOL implantation and found a mean scotoma size similar to that of previous studies on multifocal and accommodating IOLs.
The good visual and refractive outcomes, high level of spectacle independence, and low level of visual disturbances obtained in our series led to high levels of patient satisfaction. We found that 80% of patients reported complete satisfaction with the surgical outcome, and 16% reported to be moderately satisfied. Likewise, 88% of patients would choose the same IOL again, and 86% of patients would recommend the surgery and IOL to others. These results are consistent with those reported for other types of multifocal IOLs. Lubinski et al. [26] found that mean overall patient satisfaction was 9.19 ± 1.20 (scale from 1 to 10, with 10 being the best score) at 6 months after implantation of an aspheric bifocal diffractive IOL.
As with any scientific study, our clinical study has several limitations that should be acknowledged. First, corrected near and intermediate visual acuity were not measured or recorded. These parameters are important for determining the potential interference of residual refractive error on final visual outcome. Another limitation was the use of a non-validated questionnaire to evaluate patient satisfaction, spectacle independence, and photic phenomena [6]. Future studies should be conducted using validated questionnaires in order to assess these parameters. This study can be considered an initial approach in evaluating the impact of AT LISA trifocal IOL implantation on patient daily activities.
In conclusion, cataract surgery with implantation of the AT LISA tri 839 MP IOL provides excellent distant, intermediate, and near visual outcomes. It is also associated with a high level of refractive correction predictability, a minimal level of disturbing photic phenomena, a positive impact on performance of vision-related daily activities, and high levels of postoperative patient satisfaction.
Figures and Tables
 | Fig. 1Distribution of monocular and binocular postoperative uncorrected distant, intermediate, and near visual outcomes in the analyzed sample. UDVA = uncorrected distance visual acuity; UIVA = uncorrected intermediate visual acuity; UNVA = uncorrected near visual acuity. |
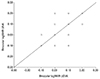 | Fig. 2Scatterplot showing the relationship between postoperative binocular logarithm of the minimum angle of resolution (logMAR) uncorrected distance visual acuity (UDVA) and uncorrected intermediate visual acuity (UIVA). |
 | Fig. 3Distribution of patient responses regarding difficulty performing the following activities (scale: 1 = yes, 2 = partly, 3 = no, and 4 = no assessable): reading the newspaper, reading a book, watching TV, driving a car during the day, driving a car at night, shopping, doing computer work, working in the house or garden, and doing handicraft work. |
Table 1
Summary of the preoperative and postoperative visual and refractive data in the analyzed sample

Table 2
Comparison of our monocular outcomes to those obtained by previous authors using different multifocal IOL modalities

IOL = intraocular lens; AL = axial length; logMAR = logarithm of the minimum angle of resolution; UDVA = uncorrected distance visual acuity; CDVA = corrected distance visual acuity; UNVA = uncorrected near visual acuity; CNVA = corrected near visual acuity; UIVA = uncorrected intermediate visual acuity; CIVA = corrected intermediate visual acuity.
References
1. Gatinel D, Pagnoulle C, Houbrechts Y, Gobin L. Design and qualification of a diffractive trifocal optical profile for intraocular lenses. J Cataract Refract Surg. 2011; 37:2060–2067.
2. Valle P, Oti J, Canales V, Cagigal M. Visual axial PSF of diffractive trifocal lenses. Opt Express. 2005; 13:2782–2792.
3. Mojzis P, Kukuckova L, Majerova K, et al. Comparative analysis of the visual performance after cataract surgery with implantation of a bifocal or trifocal diffractive IOL. J Refract Surg. 2014; 30:666–672.
4. Mojzis P, Pena-Garcia P, Liehneova I, et al. Outcomes of a new diffractive trifocal intraocular lens. J Cataract Refract Surg. 2014; 40:60–69.
5. Marques EF, Ferreira TB. Comparison of visual outcomes of 2 diffractive trifocal intraocular lenses. J Cataract Refract Surg. 2015; 41:354–363.
6. Law EM, Aggarwal RK, Kasaby H. Clinical outcomes with a new trifocal intraocular lens. Eur J Ophthalmol. 2014; 24:501–508.
7. Ramon ML, Pinero DP, Perez-Cambrodi RJ. Correlation of visual performance with quality of life and intraocular aberrometric profile in patients implanted with rotationally asymmetric multifocal IOLs. J Refract Surg. 2012; 28:93–99.
8. Alio JL, Plaza-Puche AB, Pinero DP, et al. Quality of life evaluation after implantation of 2 multifocal intraocular lens models and a monofocal model. J Cataract Refract Surg. 2011; 37:638–648.
9. Cochener B, Vryghem J, Rozot P, et al. Clinical outcomes with a trifocal intraocular lens: a multicenter study. J Refract Surg. 2014; 30:762–768.
10. Alio JL, Montalban R, Pena-Garcia P, et al. Visual outcomes of a trifocal aspheric diffractive intraocular lens with microincision cataract surgery. J Refract Surg. 2013; 29:756–761.
11. Sheppard AL, Shah S, Bhatt U, et al. Visual outcomes and subjective experience after bilateral implantation of a new diffractive trifocal intraocular lens. J Cataract Refract Surg. 2013; 39:343–349.
12. Vryghem JC, Heireman S. Visual performance after the implantation of a new trifocal intraocular lens. Clin Ophthalmol. 2013; 7:1957–1965.
13. Cochener B, Vryghem J, Rozot P, et al. Visual and refractive outcomes after implantation of a fully diffractive trifocal lens. Clin Ophthalmol. 2012; 6:1421–1427.
14. Lesieur G. Outcomes after implantation of a trifocal diffractive IOL. J Fr Ophtalmol. 2012; 35:338–342.
15. Voskresenskaya A, Pozdeyeva N, Pashtaev N, et al. Initial results of trifocal diffractive IOL implantation. Graefes Arch Clin Exp Ophthalmol. 2010; 248:1299–1306.
16. Schmickler S, Bautista CP, Goes F, et al. Clinical evaluation of a multifocal aspheric diffractive intraocular lens. Br J Ophthalmol. 2013; 97:1560–1564.
17. Friedrich R. Intraocular lens multifocality combined with the compensation for corneal spherical aberration: a new concept of presbyopia-correcting intraocular lens. Case Rep Ophthalmol. 2012; 3:375–383.
18. Alio JL, Grabner G, Plaza-Puche AB, et al. Postoperative bilateral reading performance with 4 intraocular lens models: six-month results. J Cataract Refract Surg. 2011; 37:842–852.
19. Alio JL, Plaza-Puche AB, Pinero DP, et al. Optical analysis, reading performance, and quality-of-life evaluation after implantation of a diffractive multifocal intraocular lens. J Cataract Refract Surg. 2011; 37:27–37.
20. Alfonso JF, Fernandez-Vega L, Puchades C, Montes-Mico R. Intermediate visual function with different multifocal intraocular lens models. J Cataract Refract Surg. 2010; 36:733–739.
21. Alfonso JF, Puchades C, Fernandez-Vega L, et al. Visual acuity comparison of 2 models of bifocal aspheric intraocular lenses. J Cataract Refract Surg. 2009; 35:672–676.
22. Alfonso JF, Fernandez-Vega L, Baamonde MB, Montes-Mico R. Prospective visual evaluation of apodized diffractive intraocular lenses. J Cataract Refract Surg. 2007; 33:1235–1243.
23. Alfonso JF, Fernandez-Vega L, Senaris A, Montes-Mico R. Prospective study of the Acri.LISA bifocal intraocular lens. J Cataract Refract Surg. 2007; 33:1930–1935.
24. Alio JL, Pinero DP, Plaza-Puche AB, Chan MJ. Visual outcomes and optical performance of a monofocal intraocular lens and a new-generation multifocal intraocular lens. J Cataract Refract Surg. 2011; 37:241–250.
25. Alba-Bueno F, Vega F, Millan MS. Halos and multifocal intraocular lenses: origin and interpretation. Arch Soc Esp Oftalmol. 2014; 89:397–404.
26. Lubinski W, Gronkowska-Serafin J, Podboraczynska-Jodko K. Clinical outcomes after cataract surgery with implantation of the Tecnis ZMB00 multifocal intraocular lens. Med Sci Monit. 2014; 20:1220–1226.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download