Abstract
Purpose
To compare the two transscleral fixation (TSF) techniques of intrascleral pocket and conventional scleral flap with conjunctival division techniques in terms of short-term clinical effects.
Methods
This retrospective cohort study included all consecutive patients with aphakia in Gyeongsang National University Hospital in Jinju, Korea, who underwent TSF between January 2012 and December 2014. The medical records of all patients were retrospectively reviewed, and the endothelial cell count (ECC), refraction, best-corrected visual acuity (BCVA), intraocular pressure, slit lamp, and fundus examination results before and 1 day and 6 months after surgery were recorded. The postoperative complications and visual outcomes were also recorded.
Results
The intrascleral pocket and conventional-flap groups did not differ significantly in terms of demographics, presurgical BCVA, or ECC. However, the intrascleral pocket group had a significantly lower BCVA at 1 day and 6 months after surgery compared to the conventional-flap group. The two groups did not differ in terms of ECC 6 months after surgery. The intrascleral pocket group had no postoperative complications, but five patients in the conventional-flap group complained of irritation. In both groups, the intraocular lens was well positioned without tilting or subluxation, and astigmatism was significantly reduced at 1 day and 6 months after surgery.
Conclusions
The intrascleral pocket technique of TSF does not involve conjunctival dissection and is a successful method of sulcus fixation. It stably corrects the intraocular lens and is easy to perform, which helps to reduce operation time. It also reliably yields rapid visual acuity recovery without complications.
Transscleral fixation (TSF) of posterior chamber intraocular lenses (PCIOLs) allows implantation in the absence of sufficient capsular support. There are various methods for secondary intraocular lens (IOL) TSF at the ciliary sulcus or pars plana [123456]. TSF technique usually needs conjunctival dissections to create a scleral bed for the route of fixation sutures and to conceal the knot [789]. However, knot exposure remains one of the most common complications of this procedure. To avoid this complication, scleral flaps that cover the knots are often used. Scleral tunnels or scleral pockets are also sometimes used to avoid knot exposure [268]. However, these procedures still cannot completely prevent knot exposure. Moreover, scleral flaps require considerable technical skills and thus are associated with prolonged operation time. In addition, when there is adhesion of the sclera and conjunctiva or if there is a corneal wound at the flap site, it is difficult to generate the scleral flap.
To overcome these problems, the intrascleral pocket technique was introduced for TSF of IOL in previously vitrectomized eyes [10]. The present retrospective cohort study compared the intrascleral pocket and conventional scleral flap techniques with conjunctival division techniques in terms of short-term clinical results.
The institutional review board of Gyeongsang National University Hospital approved the study protocol (no. 2015-06-031), and the protocol complied with the tenets of the Declaration of Helsinki. All consecutive patients in a tertiary referral hospital, Gyeongsang National University Hospital in Jinju, Korea, who underwent TSF for aphakia due to various causes, including IOL dislocation, retinal detachment, trauma, zonulysis, endophthalmitis, phacomorphic, and acute angle closure glaucoma, between January 2012 and December 2014 were identified by a review of the medical records. Before surgery and 1 day and 6 months after surgery all patients underwent examinations to measure refraction, best-corrected visual acuity (BCVA), intraocular pressure, and specular microscopy, as well as slit lamp and fundus examinations. The power of IOL was calculated using the Sanders-Retzlaff-Kraff II formula. The postoperative complications were recorded.
The intrascleral pocket technique for TSF was conducted by one surgeon (KSJ), and the surgical procedures were as follows: at the limbus, two points 180° from each other were marked (Fig. 1A). To make a 2-mm-sized pocket, lamellar dissection without conjunctival dissection was performed with a crescent blade, then the blade was advanced about 1 to 1.5 mm (Fig. 1B and 1C). A straight needle attached to 10-0 polypropylene was passed through the transconjunctival transcleral passage, which was located 1.5 mm posterior from the limbus. A prolene suture was then docked using a 26-gauge needle (Fig. 1D). Anterior to the limbus, a clear corneal incision (CCI) was made using a keratome, and the prolene sutures were exteriorized through the CCI pocket. An ophthalmic viscosurgical device was inserted into the anterior chamber. A three-piece foldable acrylic IOL (SENSAR Soft Acrylic IOL; Abbott Medical Optics, Santa Ana, CA, USA) was injected through the CCI, and the prolene sutures for each haptic were tied (Fig. 1E). The IOL was placed in the anterior chamber, and its orientation was adjusted by pulling the prolene sutures. The IOL was centralized, and the ends of the prolene were sutured in the intrascleral pocket (Fig. 1F). To avoid exposure, knots were buried under the sclera flaps (Fig. 1G and 1H). The CCI and other paracentesis wounds were then hydrated, and the conjunctival edges were joined without suture.
The scleral flap with conjunctival division technique was as follows: after conjunctival dissection, a triangular-shaped scleral flap was made, a 2.8-mm CCI was generated at the anterior limbus using a keratome, and a three-piece foldable acrylic IOL was injected. The haptic ends were exteriorized through the CCI, after which each haptic was tied. After IOL centration, the scleral flap ends and conjunctiva were sutured.
Continuous data were presented as mean ± standard deviation, and categorical variables were presented as number (%). The two surgical groups were compared in terms of BVCA, endothelial cell count (ECC), spherical equivalent, and astigmatism using the paired t-test. All statistical analyses were performed using IBM SPSS ver. 19.0 (IBM Co., Armonk, NY, USA). A p-value less than 0.05 was considered to indicate statistical significance.
In total, 40 consecutive patients with aphakia underwent TSF in our hospital between January 2012 and December 2014. The mean age of the cohort was 59.8 ± 4.1 years, and there were 28 males and 12 females. The mean age of the intrascleral pocket and conventional-flap groups was 59.7 ± 9.2 and 59.8 ± 9.7 years, respectively. In both groups, the main cause of aphakia was IOL dislocation. Other causes were phacoemulsification, lens dislocation, zonulysis, and vitrectomy with lensectomy, which occurred in the two groups with similar frequencies (Table 1). The two groups did not differ significantly in terms of preoperative BCVA and ECC or ECC at 6 months after surgery (Table 2). However, the intrascleral pocket group had significantly better BCVA at 1 day and 6 months after surgery compared to the conventional-flap group (p = 0.03 and 0.04, respectively). The intrascleral pocket group did not experience any postoperative complications. In contrast, five of the 20 patients in the conventional-flap group complained of irritation after surgery (Table 2). One day and 6 months after surgery, the intrascleral pocket group exhibited significant decrease in spherical diopter (p = 0.018 and 0.005 compared to preoperative values, respectively) and astigmatism (p = 0.027 and 0.028, respectively). This was also observed for the conventional-flap group for spherical diopter (p = 0.000 and 0.007, respectively) and astigmatism (p = 0.009 and 0.007, respectively) (Fig. 2A and 2B).
TSF of an IOL is widely used for aphakic patients with poor support of the posterior chamber or ciliary body. Many recent studies have reported modifications of the TSF technique that was first introduced by Malbran et al. in 1986 [111213]. However, all of these methods can cause suture-related complications, including knot exposure or IOL dislocation due to suture decomposition or breakage. Of these complications, knot exposure is one of the most common and can have deleterious outcomes as it can act as a pathway for bacterial invasion into the eye, thereby causing endophthalmitis [14].
When Szurman et al. [12] retrospectively analyzed the results of 45 eyes that underwent TSF of PCIOL using Z-sutures and 22 eyes that underwent TSF of an iris prosthesis, they found one case of ciliary body hemorrhage during the 22.4 months of follow-up, but no complications such as knot exposure, suture looseness, conjunctival atrophy, or chronic inflammation. Ma et al. [5] also analyzed the clinical outcomes of a knotless external fixation technique of PCIOL TSF in five patients who had to undergo this technique because of adhesion between the conjunctiva and cornea or because the location of the conjunctival flap was near a corneal wound caused by trauma. Therefore, this study introduced the sutureless intrascleral pocket technique and compared the effects and complications including astigmatism or postoperative visual prognosis.
Compared with conventional techniques, this technique resulted in less irritation and astigmatism since knots were buried in the intrascleral pocket, and vertical and regular wounds were formed without a gap of wound. In addition, this technique led to rapid visual recovery and return to daily life, since the visual acuity the day after the operation was comparable to the BCVA before the surgery. During the follow-up period, there were no complications except for mild ciliary body hemorrhage in one case and IOL tilting immediately after the operation due to excessive knot tightness in another case. The BCVA in 16 of 20 cases (80%) improved, while the remaining case did not exhibit a change in BCVA. Thus, the outcomes of the intrascleral pocket technique in the present study were generally as successful as those of the knotless external fixation technique of PCIOL in a previous study [6].
The intrascleral pocket technique of TSF is especially useful for patients who previously underwent vitrectomy. Patients after vitrectomy, especially those who underwent surgery with a 20-gauge needle, usually have a relatively thin conjunctiva or conjunctiva-Tenon-scleral complex due to previous conjunctival dissection. This makes conjunctival dissection more difficult and increases the possibility of conjunctival defects and scleral injury. Thus, the intrascleral pocket technique will be particularly useful for such patients. In addition, since this technique does not involve conjunctival dissection, the operation time and bleeding risk are reduced. Moreover, subsequent glaucoma surgery can improve the success rate of the intrascleral pocket technique because the conjunctiva and Tenon's space maintain their native integrity [10]. The intrascleral pocket technique also allows for rapid visual acuity recovery and return to daily life because the associated irritation is low. In addition, the vertical and regular wound without a gap helps to reduce astigmatism. In a previous study using the sutureless intrascleral pocket technique [10], there was no specific finding from photographs 1 day after the surgery. This prompted us to reassess patients at 6 months after the surgery in this study, and the wounds were found to be clean without dehiscence or knot exposure (Fig. 3A and 3B).
Unlike the reverse pocket technique, the intrascleral pocket technique leaves the corneal limbus intact, which reduces the chance of injury to the corneal nerve. Moreover, it is possible to perform the intrascleral pocket technique with topical anesthesia because it is associated with less pain than other techniques. In addition, the intrascleral pocket technique is quite similar to glaucoma or flap-making procedures, which means that surgeons can rapidly become proficient in this technique. There is also no possibility of angle injury or anterior chamber puncture [10].
In conclusion, the present study showed that the intrascleral pocket technique of TSF had better clinical results than the conventional scleral flap with conjunctival division technique, as determined by ophthalmological examinations before and 1 day and 6 months after the operation. The improvement in BCVA was more marked in the intrascleral pocket group, and no postoperative complications were observed. These observations, together with the fact that this technique is relatively easy, suggest that this technique is a good method of TSF.
This study has some limitations. First, the sample size was small. Second, the patients were only followed up for 6 months. Further studies with longer-term clinical follow- up are required. However, the simplicity and good outcomes of this technique suggest that it is a good method of TSF.
Figures and Tables
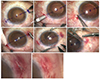 | Fig. 1Intrascleral pocket technique. (A,B) Two points were marked at 180° apart at the limbus. To create a 2-mm-sized pocket, lamellar dissection without conjunctival dissection was performed with a crescent blade. (C) The constructed pocket was visualized. (D) A 9-0 straight needle was passed through the transconjunctival transcleral passage. (E) A three-piece foldable acrylic intraocular lens was inserted via clear corneal incision, and then each haptic end was exteriorized through clear corneal incision and tied with prolene suture. (F) The suture was placed in the intrascleral pocket with forceps opening one part of the pocket. (G,H) Each knot was buried under scleral flaps to prevent exposure, and the conjunctiva was joined without suture. |
 | Fig. 2The intrascleral pocket group and conventional-flap group demonstrated significant decrease in spherical diopter (A) and astigmatism (B) at 1 day and 6 months after the operation. *Paired t-test. |
Acknowledgements
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT & Future Planning (NRF-2015R1C1A1A02037702).
References
1. Wagoner MD, Cox TA, Ariyasu RG, et al. Intraocular lens implantation in the absence of capsular support: a report by the American Academy of Ophthalmology. Ophthalmology. 2003; 110:840–859.
2. Lewis JS. Ab externo sulcus fixation. Ophthalmic Surg. 1991; 22:692–695.
3. Teichmann KD. Pars plana fixation of posterior chamber intraocular lenses. Ophthalmic Surg. 1994; 25:549–553.
4. Kim DH, Heo JW, Hwang SW, et al. Modified transscleral fixation using combined temporary haptic externalization and injector intraocular lens implantation. J Cataract Refract Surg. 2010; 36:707–711.
5. Ma DJ, Kim MK, Wee WR. Knotless external fixation technique for posterior chamber intraocular lens transscleral fixation: a 5-case analysis. J Korean Ophthalmol Soc. 2012; 53:1609–1614.
6. Lin CP, Tseng HY. Suture fixation technique for posterior chamber intraocular lenses. J Cataract Refract Surg. 2004; 30:1401–1404.
7. Solomon K, Gussler JR, Gussler C, Van Meter WS. Incidence and management of complications of transsclerally sutured posterior chamber lenses. J Cataract Refract Surg. 1993; 19:488–493.
8. Lewis JS. Sulcus fixation without flaps. Ophthalmology. 1993; 100:1346–1350.
9. Kir E, Kocaturk T, Dayanir V, et al. Prevention of suture exposure in transscleral intraocular lens fixation: an original technique. Can J Ophthalmol. 2008; 43:707–711.
10. Cho YW, Chung IY, Yoo JM, Kim SJ. Sutureless intrascleral pocket technique of transscleral fixation of intraocular lens in previous vitrectomized eyes. Korean J Ophthalmol. 2014; 28:181–185.
11. Malbran ES, Malbran E Jr, Negri I. Lens guide suture for transport and fixation in secondary IOL implantation after intracapsular extraction. Int Ophthalmol. 1986; 9:151–160.
12. Szurman P, Petermeier K, Aisenbrey S, et al. Z-suture: a new knotless technique for transscleral suture fixation of intraocular implants. Br J Ophthalmol. 2010; 94:167–169.
13. Stewart MW, Landers MB 3rd. Transscleral intraocular lens fixation with a "homemade" needle and hook. J Cataract Refract Surg. 2006; 32:200–202.
14. Heilskov T, Joondeph BC, Olsen KR, Blankenship GW. Late endophthalmitis after transscleral fixation of a posterior chamber intraocular lens. Arch Ophthalmol. 1989; 107:1427.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download