Abstract
Purpose
To compare the clinical characteristics of unilaterally progressing glaucoma (UPG) and simultaneously bilaterally progressing glaucoma (BPG) in medically treated cases.
Methods
Primary open angle glaucoma patients were classified as having UPG or BPG according to an assessment of optic disc and retinal nerve fiber layer photographs and visual field analysis. Risk factors including the presence of systemic diseases (hypertension, diabetes, cerebrovascular accident, migraine, and dyslipidema) were compared between the UPG and BPG groups. Baseline characteristics and pre- and post-treatment intraocular pressure (IOP) were compared between the progressing eye (PE) and the non-progressing eye (NPE) within the same patient in the UPG group and between the faster progressing eye and the slower progressing eye in the BPG group.
Results
Among 343 patients (average follow-up period of 4.2 years), 43 were categorized into the UPG group and 31 into the BPG group. The prevalence of all analyzed systemic diseases did not differ between the two groups. PEs in the UPG group had more severe pathology in terms of baseline visual field parameters than NPEs (mean deviation -6.9 ± 5.7 vs. -2.9 ± 3.9 dB, respectively; p < 0.001). However, baseline IOP, mean follow-up IOP, and other clinical characteristics were not significantly different between the PE and the NPE in the UPG group. The progression rate was significantly higher in the faster progressing eye in patients with BPG than in the PE for patients with UPG (-3.43 ± 3.27 vs. -0.70 ± 1.26 dB/yr, respectively; p = 0.014).
Glaucoma is characterized by the progressive loss of the neuroretinal rim in the optic disc and accompanying visual functional decay. As this pathologic change is irreversible, treatment usually focuses on slowing or halting progression of the condition. Therefore, identifying progression and measuring the progression rate are essential to glaucoma patient care. Glaucoma is mostly known as a bilateral disease. However, it can often manifest asymmetrically, with some cases showing a unilateral presentation. Bilaterally fast progressing glaucoma is the most important subtype to be aggressively treated, because bilateral visual field (VF) impairment substantially impacts a patient's quality of daily life [1,2,3].
Elevated intraocular pressure (IOP) is the principal risk factor for glaucoma [4,5,6]. However, the majority of glaucoma cases present with statistically normal IOP values in Eastern Asian countries, with some cases progressing despite well-controlled IOP [7,8,9,10]. Thus, risk factors for glaucoma progression other than IOP are under investigation [11,12]. Furthermore, differentiating factors for unilateral and bilateral glaucoma are of particular interest. According to a study by Kim and Kim [13], vascular diseases such as diabetes or cerebrovascular accidents are associated with the development of bilateral glaucoma, likely because these vascular pathologies are systemic in nature and vascular insufficiencies may influence both eyes. We therefore hypothesized that differences may exist between unilaterally progressing glaucoma (UPG) and bilaterally simultaneously progressing glaucoma (BPG). In this study, we aimed to investigate and compare the clinical characteristics of medically treated UPG and BPG. Additionally, we compared the faster progressing eye (FPE) and the relatively slower progressing fellow eye (SPE) within the same patient in the BPG group, as well as the ocular characteristics of the progressing eye (PE) and the non-progressing eye (NPE) in the UPG group.
This retrospective study included 343 glaucoma subjects who were examined at the glaucoma clinic of the Asan medical center. Patients who met our inclusion criteria of at least three years of follow-up and seven or more reliable VF measurements were consecutively enrolled by medical record review. Eyes that underwent intraocular surgery (including cataract and glaucoma filtering procedures) during the follow-up period were excluded. At initial diagnosis, each patient received a comprehensive ophthalmologic examination that included a review of medical history for the presence of systemic diseases like systemic hypertension, diabetes, cerebrovascular accident, dyslipidemia, and migraine, measurement of best-corrected visual acuity to confirm that visual acuity was adequate for automated perimetry performance, slit-lamp biomicroscopy, Goldmann applanation tonometry, gonioscopy, dilated fundoscopic examination using a 90- or 78-diopter lens, stereoscopic optic disc and retinal nerve fiber layer (RNFL) photography, VF examination by standard automated perimetry (Humphrey Swedish interactive threshold algorithm standard strategy 24-2; Carl Zeiss Meditec, Dublin, CA, USA), and measurement of central corneal thickness (CCT; DGH-550 instrument, DGH Technology Inc., Exton, PA, USA).
All included patients met the following criteria at the baseline exam: best-corrected visual acuity of 20 / 30 or better, with a spherical equivalent (SE) within ±5 diopters and a cylinder correction within +3 diopters; VF mean deviation (MD) higher than -20 dB; and the presence of a normal anterior chamber and open-angle on slit-lamp and gonioscopic examinations. Patients with concomitant diseases known to affect the VF were excluded. Diagnosis of glaucoma was based on both the presence of typical glaucomatous changes in the optic disc and glaucomatous VF defect. Thus, eyes with a glaucomatous optic disc and a normal VF were not defined as having glaucoma. Glaucomatous optic disc change included increased cupping (vertical cup-disc ratio more than 0.7), a difference in the vertical cup-disc ratio (more than 0.2 between the eyes), diffuse or focal neural rim thinning, disc hemorrhage, or RNFL defects. Eyes defined as having glaucomatous VF defects met two of the following three criteria (as confirmed by more than two reliable consecutive tests): 1) a cluster of three points with a probability of less than 5% on a pattern deviation map in at least one hemifield, including at least one point with a probability of less than 1% or a cluster of two points with a probability of less than 1%; 2) a glaucoma hemifield test result outside the normal limit; and 3) a pattern standard deviation result of less than 5%. Reliable VF assessment was defined as a VF test with a false-positive error of less than 15%, a false-negative error of less than 15%, and a fixation loss of less than 20%. The first VF test was excluded from analysis to reduce the learning effect. If at least one eye showed glaucomatous changes, that patient was included for analysis. IOP-lowering medication was prescribed if the eyes showed glaucomatous optic disc changes or had both a glaucomatous optic disc and VF changes. Glaucomatous eyes with secondary causes were excluded in the current study.
All procedures conformed to the Declaration of Helsinki, and the study was approved by the institutional review board of the Asan Medical Center.
Since glaucomatous damage involves both structural and functional changes that may not appear at the same time, glaucoma progression was determined by either structural or functional measures. Structural progression was assessed using a stereoscopic optic disc and red-free RNFL photographs. Serial stereoscopic photographs were displayed on an liquid crystal display monitor. Two glaucoma experts (KRS and JHN) independently assessed all of the photographs in order to estimate the glaucoma progression between the patients' first and last visits. Both graders were blind to each other's progression assessments and to all clinical and VF information. Photographs were presented in chronological order and with masking of patient identification, age, and test date. Each grader viewed all photographs of each eye before making an assessment and was asked to determine the possible presence of a glaucomatous optic disc or of RNFL progression, as revealed by an increase in the extent of neuroretinal rim thinning, enhancement of disc excavation, any widening or deepening of a RNFL defect, and/or the appearance of new disc hemorrhage [14,15]. Each grader classified each glaucomatous eye as either stable or progressing. If the opinions of the two observers differed, a third examiner (DJ) made the final decision.
Functional progression was determined using a VF series. Commercial software (Guided Progression Analysis, Carl Zeiss Meditec) was used to determine progressive functional loss of the VF. VF defect progression was defined as a significant deterioration from the baseline pattern of deviation at three or more of the same test points and was evaluated on three consecutive examinations [16].
If only one eye showed progression by either structural or functional assessment during the follow-up period, the patient was included in the UPG group. In contrast, if both eyes showed progression, the patient was included in the BPG group. Age, gender, and the prevalence of systemic diseases (systemic hypertension, diabetes, cerebrovascular accident, migraine, and dyslipidema) were compared between the UPG and BPG groups. In the UPG group, pre-treatment IOP, mean post-treatment IOP, CCT, SE, baseline VF MD, VF pattern standard deviation, and progression rates were compared between the PE and the NPE within the same patient. The progression rates (MD slope) were determined by linear regression analysis of MD values in serial VF analyses. In the BPG group, the same parameters were compared between the FPE and the SPE within the same patient. The Wilk-Shapiro test was used to determine the distribution of numerical data. Normally distributed data were compared between the UPG and BPG groups using unpaired t-tests. To compare categorical data, the chisquare test was employed. The paired t-test was used to compare eyes within the same patient. Non-normally distributed data were compared using either the Mann-Whitney or Wilcoxon signed rank test. Statistical analyses were performed using IBM SPSS ver. 21.0 (IBM Corp., Armonk, NY, USA). A p-value less than 0.05 was considered significant.
A total of 343 Korean patients were included in the final analysis, of which 182 were men and 161 were women. The mean follow-up period was 4.2 years. At baseline, 134 patients had unilateral glaucoma. Among these 134 patients, 102 showed glaucomatous optic disc changes but a normal VF in the fellow eye, while the remaining 32 patients had a normal appearing optic disc and a normal VF in the fellow eye. Among the 134 unilateral glaucoma patients, 25 patients showed unilateral progression during follow-up while 6 patients showed bilateral progression; thus, 31 patients had either unilateral or bilateral progression while 103 patients were stable. Among the 32 patients with unilateral glaucoma and a normal optic disc and VF in the fellow eye, none of the fellow eyes showed progression. At baseline, 209 patients had bilateral glaucoma, of which 43 showed progression with 25 showing bilateral progression. These data are shown in Fig. 1.
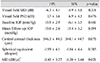
Hence, the BPG group consisted of 31 patients (6 from the unilateral glaucoma at baseline group and 25 from the bilateral glaucoma at baseline group), while the UPG group consisted of 43 patients (25 with unilateral glaucoma at baseline and 18 with bilateral glaucoma at baseline). The mean age was significantly higher in the UPG group than in the BPG group (58.7 ± 10.0 vs. 52.6 ± 3.9 years, p = 0.035). However, the prevalence of all analyzed systemic diseases was not different between the two groups (Table 1). PEs and NPEs were compared within the same patient in the UPG group. All PEs in the UPG group showed more severe clinical characteristics in terms of baseline VF parameters. However, baseline IOP, mean follow-up IOP, CCT, and SE were not significantly different between the PE and the NPE (Table 2).
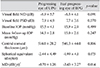
The progression rate determined by the MD slope was compared between the FPE and the SPE within the same patient in the BPG group. As expected, the progression rate was higher in the FPE, but other parameters did not differ significantly (Table 3). When the PE in the UPG group was compared to the FPE eye in the BPG group, the progression rate was significantly higher in the FPE in the BPG group, but no other parameters differed (Table 4).
According to the data from 343 patients analyzed in this study, 134 (39.1%) presented with unilateral glaucoma at baseline. Among these unilateral glaucoma patients, 76.1% showed glaucomatous optic disc changes in the fellow eye, while only 32 patients out of all glaucomatous patients (9.3%) had completely unilateral glaucoma with both a normal optic disc and a normal VF in the fellow eye. Among the 134 unilateral glaucoma patients, 23.1% showed progression during the follow-up period. The fellow eye of the 32 patients with unilateral glaucoma did not show progression during follow-up, although IOP-lowering treatment was not performed in those eyes. Among the 209 bilateral glaucoma patients, 20.6% showed progression. Thus, the overall prevalence of progression was similar between patients with unilateral glaucoma and bilateral glaucoma. Interestingly, 80.6% of patients with progressing disease in the unilateral glaucoma group demonstrated unilateral progression, while 58.1% of patients with progressing disease in the bilateral glaucoma group showed bilateral progression. Hence, unilateral glaucoma has a tendency to progress unilaterally and bilateral glaucoma bilaterally. The reported risk of fellow eye progression in unilateral glaucoma varies among previous studies [17,18,19]. Chen and Park [19] showed that 6.2% of fellow eyes progressed over a period of 8.7 years. Among 134 unilateral perimetric glaucoma patients, 6 (4.5%) showed progression in the fellow eye in the present study.
The results from the current study indicated no significant differences in the prevalence of any analyzed systemic disease between the UPG and BPG groups. Overall, the prevalence of systemic disease was very low in both groups, which may affect the statistical analysis and contribute to the lack of significance of the data. In contrast to the present data, a study by Kim and Kim [13] showed that the prevalence of systemic disease was different between patients with unilateral and bilateral glaucoma. The discrepancy is likely due to the fact that systemic disease can affect the development of bilateral glaucoma, but the progression of disease is modulated by various factors thus reducing the effect of systemic disease on glaucoma progression. In fact, risk factors for the development and progression of glaucoma may differ. For instance, myopia is known to be a risk factor for the development of glaucoma but not for progression of the disease, although this remains under debate [20,21,22,23,24,25].
When we compared the PE and the NPE in the UPG group, the PE showed a more advanced disease status at baseline. However, there was no difference in IOP, CCT, and SE between the FPE and SPE in the BPG group.
In the comparison between the PE and NPE in the UPG group, IOP was not found to differ between the two eyes. Similarly, IOP did not differ between the FPE and the SPE in the BPG group. As shown by mean baseline IOP measurements, most of the patients in the current study had low IOP and can be categorized as having normal-tension or low-tension glaucoma. Whether a correlation exists between IOP asymmetry and glaucoma severity in cases of normal-tension glaucoma has been under debate in previous studies [26,27,28]. Some studies have shown that higher IOP is related to more advanced stages of glaucoma [26,27]. However, the Low-Pressure Glaucoma Treatment Study reported that IOP asymmetry is unrelated to VF asymmetry [28]. The present study revealed no differences in IOP between the PE and the NPE in the UPG group or between the FPE and the SPE in the BPG group. While IOP reduction substantially decreased the progression rate in the Collaborative Normal-Tension Glaucoma Study, some treated eyes also showed progression in that randomized clinical trial [7]. Thus, taken together, our results and those of previous studies suggest that factors other than IOP, which may affect the progression of glaucoma with lower IOP readings, should be investigated in future studies.
Furthermore, no differences were noted in baseline VF defect severity and IOP values between the PE in the UPG group and the FPE in the BPG group; however, the progression rate was significantly higher in the FPE in the BPG group. The progression rate of the PE in the UPG group was -0.70 dB/year, which is approximately two times higher than the usual progression rates reported in previous randomized clinical trials (-0.36 to -0.41 dB/yr) [29,30]. The progression rate of the FPE in the BPG group was approximately five times higher (-3.43 vs. -0.70 dB/yr) than that of the PE in the UPG group. Thus, we speculate that in simultaneously bilaterally progressing patients, both eyes progress faster than the PE in UPG. In contrast, baseline VF defect severity was not different between the PE in the UPG group and the FPE in the BPG group.
The current study had several limitations. First, the prevalence of systemic disease was determined by self-reported histories from the patients. Second, the follow-up period (mean 4.2 years) was relatively short. Considering the slow-progressing nature of glaucoma, this period may not be sufficient to observe the natural progression of the disease. Some cases of unilateral glaucoma may eventually progress to bilateral glaucoma and some cases with a unilaterally progressing eye may show progression in the fellow eye over time. However, during the four years of observation in this study, unilateral glaucoma tended to progress only in the glaucomatous eye, while simultaneously bilaterally progressing patients showed much faster progression rates than those with a unilaterally progressing eye. No systemic factors analyzed in this study significantly differed in prevalence between the UPG and BPG groups. Therefore, glaucoma patients with simultaneous bilateral progression should be treated with caution in clinical practice because these cases can show relatively rapid progression.
Figures and Tables
Table 1
Comparison between the unilaterally progressing primary open angle glaucoma and bilaterally progressing primary open angle glaucoma groups

Table 2
Comparison between the PE and the NPE within the same patient in the unilaterally progressing glaucoma group
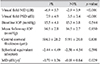
Table 3
Comparison between the FPE and the SPE within the same patient in the bilaterally progressing glaucoma group
References
1. Ramulu P. Glaucoma and disability: which tasks are affected, and at what stage of disease? Curr Opin Ophthalmol. 2009; 20:92–98.
2. Janz NK, Musch DC, Gillespie BW, et al. Evaluating clinical change and visual function concerns in drivers and nondrivers with glaucoma. Invest Ophthalmol Vis Sci. 2009; 50:1718–1725.
3. Lisboa R, Chun YS, Zangwill LM, et al. Association between rates of binocular visual field loss and vision-related quality of life in patients with glaucoma. JAMA Ophthalmol. 2013; 131:486–494.
4. Kass MA, Heuer DK, Higginbotham EJ, et al. The Ocular Hypertension Treatment Study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002; 120:701–713.
5. Sommer A, Tielsch JM, Katz J, et al. Relationship between intraocular pressure and primary open angle glaucoma among white and black Americans. The Baltimore Eye Survey. Arch Ophthalmol. 1991; 109:1090–1095.
6. Bonomi L, Marchini G, Marraffa M, et al. Prevalence of glaucoma and intraocular pressure distribution in a defined population. The Egna-Neumarkt Study. Ophthalmology. 1998; 105:209–215.
7. Collaborative Normal-Tension Glaucoma Study Group. The effectiveness of intraocular pressure reduction in the treatment of normal-tension glaucoma. Am J Ophthalmol. 1998; 126:498–505.
8. Leske MC, Heijl A, Hyman L, et al. Predictors of long-term progression in the early manifest glaucoma trial. Ophthalmology. 2007; 114:1965–1972.
9. Kim CS, Seong GJ, Lee NH, et al. Prevalence of primary open-angle glaucoma in central South Korea the Namil study. Ophthalmology. 2011; 118:1024–1030.
10. Iwase A, Suzuki Y, Araie M, et al. The prevalence of primary open-angle glaucoma in Japanese: the Tajimi Study. Ophthalmology. 2004; 111:1641–1648.
11. Sung KR, Lee S, Park SB, et al. Twenty-four hour ocular perfusion pressure fluctuation and risk of normal-tension glaucoma progression. Invest Ophthalmol Vis Sci. 2009; 50:5266–5274.
12. Berdahl JP, Fautsch MP, Stinnett SS, Allingham RR. Intracranial pressure in primary open angle glaucoma, normal tension glaucoma, and ocular hypertension: a case-control study. Invest Ophthalmol Vis Sci. 2008; 49:5412–5418.
13. Kim C, Kim TW. Comparison of risk factors for bilateral and unilateral eye involvement in normal-tension glaucoma. Invest Ophthalmol Vis Sci. 2009; 50:1215–1220.
14. Drance S, Anderson DR, Schulzer M. Collaborative Normal-Tension Glaucoma Study Group. Risk factors for progression of visual field abnormalities in normal-tension glaucoma. Am J Ophthalmol. 2001; 131:699–708.
15. Sung KR. Disc hemorrhage: is that a risk factor or sign of progression? J Glaucoma. 2012; 21:275–276.
16. Heijl A, Leske MC, Bengtsson B, et al. Measuring visual field progression in the Early Manifest Glaucoma Trial. Acta Ophthalmol Scand. 2003; 81:286–293.
17. Kass MA, Kolker AE, Becker B. Prognostic factors in glaucomatous visual field loss. Arch Ophthalmol. 1976; 94:1274–1276.
18. Susanna R, Drance SM, Douglas GR. The visual prognosis of the fellow eye in uniocular chronic open-angle glaucoma. Br J Ophthalmol. 1978; 62:327–329.
19. Chen PP, Park RJ. Visual field progression in patients with initially unilateral visual field loss from chronic open-angle glaucoma. Ophthalmology. 2000; 107:1688–1692.
20. Suzuki Y, Iwase A, Araie M, et al. Risk factors for open-angle glaucoma in a Japanese population: the Tajimi Study. Ophthalmology. 2006; 113:1613–1617.
21. Casson RJ, Gupta A, Newland HS, et al. Risk factors for primary open-angle glaucoma in a Burmese population: the Meiktila Eye Study. Clin Experiment Ophthalmol. 2007; 35:739–744.
22. Xu L, Wang Y, Wang S, et al. High myopia and glaucoma susceptibility the Beijing Eye Study. Ophthalmology. 2007; 114:216–220.
23. Wong TY, Klein BE, Klein R, et al. Refractive errors, intraocular pressure, and glaucoma in a white population. Ophthalmology. 2003; 110:211–217.
24. Leske MC, Nemesure B, He Q, et al. Patterns of open-angle glaucoma in the Barbados Family Study. Ophthalmology. 2001; 108:1015–1022.
25. Mitchell P, Hourihan F, Sandbach J, Wang JJ. The relationship between glaucoma and myopia: the Blue Mountains Eye Study. Ophthalmology. 1999; 106:2010–2015.
26. Cartwright MJ, Anderson DR. Correlation of asymmetric damage with asymmetric intraocular pressure in normal-tension glaucoma (low-tension glaucoma). Arch Ophthalmol. 1988; 106:898–900.
27. Crichton A, Drance SM, Douglas GR, Schulzer M. Unequal intraocular pressure and its relation to asymmetric visual field defects in low-tension glaucoma. Ophthalmology. 1989; 96:1312–1314.
28. Greenfield DS, Liebmann JM, Ritch R, et al. Visual field and intraocular pressure asymmetry in the low-pressure glaucoma treatment study. Ophthalmology. 2007; 114:460–465.
29. Heijl A, Bengtsson B, Hyman L, et al. Natural history of open-angle glaucoma. Ophthalmology. 2009; 116:2271–2276.
30. Anderson DR, Drance SM, Schulzer M. Collaborative Normal-Tension Glaucoma Study Group. Natural history of normal-tension glaucoma. Ophthalmology. 2001; 108:247–253.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download