Abstract
Purpose
Methods
Results
Figures and Tables
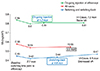 | Fig. 1Changes in mean best-corrected visual acuity (logarithm of the minimal angle of resolution, logMAR) for all cases including on-going and switching-back cases during the entire follow-up period. 2.7 months was the time point after 3 initial loading injections of aflibercept in all cases. 4.2 months was the time point of 4 or more on-going treatment of aflibercept in 14 cases. 4.6 months was the time point of switching-back treatment of bevacizumab in 10 cases. Improvement of best-correct visual acuity from baseline of all cases was statistically significant, but not significant in on-going or switching-back treatment cases during the entire follow-up period. Best-correct visual acuity was stable in on-going cases (p = 1.0) but deteriorated in switching-back cases (p = 0.06). VA = visual acuity. *p < 0.05. |
 | Fig. 2Changes in mean central macular thickness (CMT) of all cases, on-going cases, and switching-back cases during the entire follow-up period. 4.2 months was the time point of 4 or more on-going treatments of aflibercept in 14 cases. 4.6 months was the time point of switching-back treatment of bevacizumab in 10 cases. Improvement of CMT from baseline in all cases, including on-going and switching-back cases, was statistically significant during the entire follow-up period. However, after switching back to bevacizumab, CMT increased (p = 0.05) during the switching-back period. In contrast, CMT remained stable in on-going 4 or more treatment cases of aflibercept (p = 0.29) during the treatment period. *p < 0.05. |
Table 3
Qualitative analysis based on spectral domain optical coherence tomography findings of all cases

Values are presented as number or number (%); From Ho VY, et al. Am J Ophthalmol 2013;156:23-8.e2, with permission from Elsevier [5]; Results of all cases with refractory disease prior to anti-vascular endothelial growth factor treatments at 4.6 months after switching to aflibercept (4.6 months: time point before initiation of switching-back treatment); This trend was consistent among all 3 subgroups treated with previous bevacizumab treatment, ranibizumab treatment, or treatment with both agents (data not shown).
OCT = optical coherence tomography; IRF = intraretinal fluid; SRF = subretinal fluid; PED = pigment epithelial detachment; SRH = subretinal hemorrhage (additional assessment with fundus examination).




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download