This article has been
cited by other articles in ScienceCentral.
Abstract
Purpose
To evaluate the clinical outcome of viscoelastics (VE, sodium hyaluronate)-augmented trabeculectomy (VAT, 66 eyes) and conventional trabeculectomy (CT, 57 eyes) for glaucomatous eyes.
Methods
In the VAT group, half of the anterior chamber space was filled with VE via the paracentesis site at the end of CT and a balanced salt solution was injected into the anterior chamber. This procedure induced migration of VE from the anterior chamber into the bleb space; thus the bleb was elevated with underlying VE. Follow-up examinations were performed until 1 year after surgery. Success was defined as the attainment of an intraocular pressure (IOP) greater than 5 mmHg and less than 22 mmHg. If IOP was in the range of success without antiglaucoma medication, it was regarded as a complete success.
Results
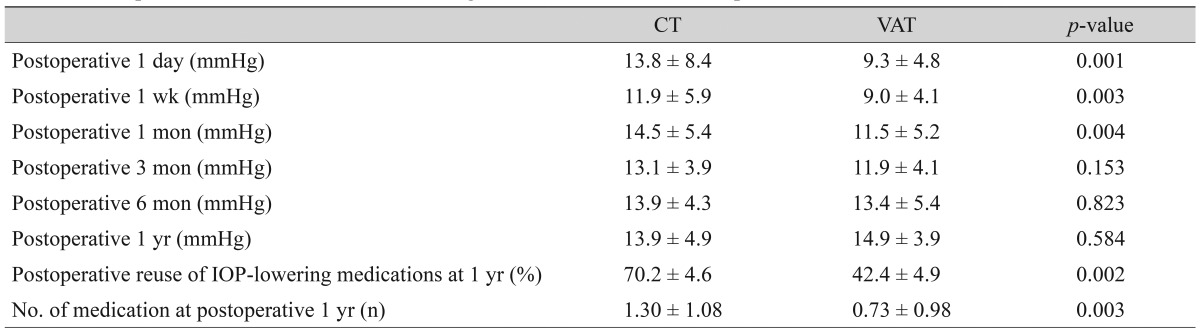
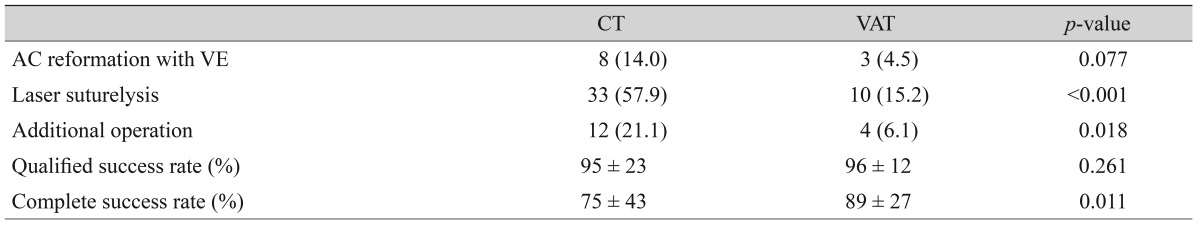
The mean postoperative IOP was significantly lower in the VAT group at postoperative 1 day, 1 week, and 1 month. The complete success rate was significantly higher in the VAT group (89%) than in the CT group (75%), though the qualified success rate was not different between the two groups. The number of IOP-lowering medications at postoperative 1 year was significantly higher in the CT group (1.30 ± 1.08 vs. 0.73 ± 0.98, p = 0.003). Among postoperative procedures, laser suture lysis was required less frequently in the VAT group (p < 0.001).
Conclusions
Placing VE within the bleb at the end of surgery may result in better IOP control and less need for IOP-lowering medication without any additional materials, cost, or time.
Go to :

Keywords: Anti-fibrotic agent, Glaucoma, Hyaluronic acid, Trabeculectomy, Viscoelastics
Trabeculectomy is a filtering procedure that connects the anterior chamber (AC) with the subconjunctival space to allow the passing of aqueous humor. Subconjunctival fibrosis associated with a filtering bleb is one of the most common causes of surgical failure [
1,
2,
3]. Thus, prevention of subconjunctival fibrosis is of crucial importance for maintaining bleb function. Another early postoperative complication is overfiltration. Overfiltration often causes a shallow or flat AC. This induces corneal endothelial decompensation or permanent peripheral anterior synechiae with subsequent intraocular pressure (IOP) elevation if not corrected properly [
4,
5,
6,
7]. Therefore, AC reformation with viscoelastics (VE) is sometimes used to treat this complication [
8,
9,
10,
11,
12].
Hyaluronic acid (HA) is an anionic, nonsulfated glycosaminoglycan that is widely distributed throughout the body. VE made of HA is used as an adjunct in various types of surgery including intraocular surgery. During intraocular surgery, VE has a role in maintaining the space in structures such as the AC or the capsular bag of the lens for the facilitation of surgical procedures or the protection of endothelial cells while performing cataract extraction or other intraocular surgeries. VE can also be used for other purposes such as preventing tissue adhesion [
13,
14,
15,
16,
17,
18]. For instance, HA has been used to prevent intestinal adhesion during abdominal surgery [
16]. HA has also been applied to trabeculectomy where it is used as a film located within the conjunctival flap [
17,
18]. Theoretically, VE within a bleb may prevent adhesion by maintaining the subconjunctival space.
The purpose of the present study is to test whether placing VE within blebs at the end of conventional trabeculectomy (CT) would augment bleb function. Furthermore, VE is frequently used for AC reformation when overfiltration after trabeculectomy results in a flat or shallow AC. It is further hypothesized that placing VE within both the AC and the bleb will be helpful for preventing both a postoperative flat AC and early bleb fibrosis. VE are generally used in CT. Thus, this procedure can be very easily combined with CT without the need for any additional materials, cost, or time.
The aim of this study was to compare the outcomes of VE-augmented trabeculectomy (VAT) with CT.
Materials and Methods
Subjects
A total of 123 patients that had undergone CT (57 eyes) or VAT (66 eyes) by a single surgeon (KRS) at the glaucoma clinic of the Asan Medical Center (Seoul, Korea) were included in this retrospective study. All included patients were followed for at least 1 year after surgery. CT was performed from March 2008 to December 2010 and VAT was performed from January 2011 to July 2011. Patients who were lost before 1 year after surgery or got ocular surgery other than glaucoma surgery during the study period were excluded. All patients that met the inclusion criteria were consecutively enrolled in the study. If both eyes met the inclusion criteria, only one eye was randomly chosen to be included in the study.
Surgical procedure
1) Conventional trabeculectomy
A fornix-based conjunctival flap was constructed in the superior area. The conjunctiva and Tenon's capsule were carefully dissected and the sub-Tenon space was widened using blunt scissors for preparation of the bleb. A limbus-based half-thickness scleral flap (2.5 mm circumference × 2 mm radius) was then prepared and a 0.2% mitomycin C soaked sponge was applied for 2 minutes under the sub-Tenon space. Copious irrigation was performed with balanced salt solution (BSS) to wash out the mitomycin C. AC paracentesis was performed through the clear cornea on the temporal side and VE (Healon, 1% sodium hyaluronate) was injected into the AC to maintain the proper space. A punch incision was performed to make a sclerotomy into the AC under the partial scleral flap. Trabeculectomy and peripheral iridectomy were performed through the sclerotomy site. The scleral flap was secured with a single 9-0 nylon suture. The conjunctival flap was closed with a 8-0 vicryl interrupted suture followed by running sutures. Bleb elevation and integrity of the conjunctival closure were checked. Topical corticosteroid (1% rimexolone), cycloplegics, and an antibiotic (0.5% moxifloxacin) were prescribed for approximately 1 month postoperatively, depending on the eye condition.
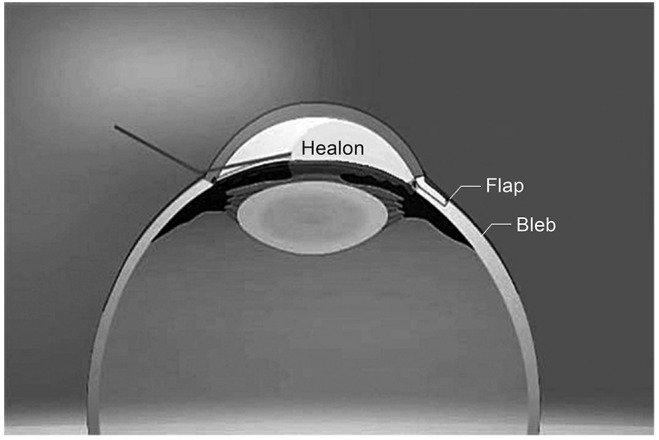
2) Viscoelastics-augmented trabeculectomy
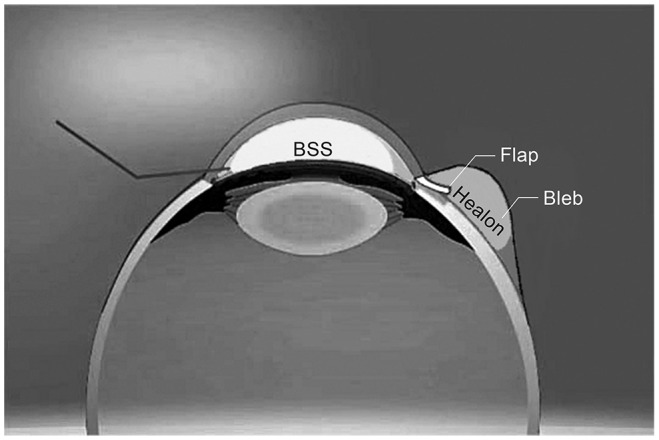
After CT, approximately half of the AC space was filled with VE applied via the paracentesis site (
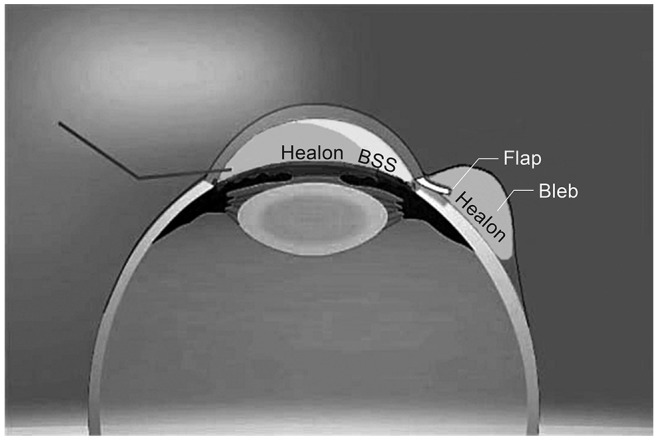
Fig. 1). Also, a small amount of BSS was injected into the AC via the same paracentesis site. While injecting BSS into the AC when the AC was filled with VE, movement of VE into the bleb space and subsequent elevation of the bleb was easily differentiated from that caused by BSS. Elevation of the bleb was much slower and firmer. The eyeball was gently pressed with an ophthalmic sponge near the bleb site. This procedure facilitated migration of VE from the AC into the bleb space; thus, the bleb was well-elevated by the underlying VE (
Fig. 2). Half of the AC space was again filled with VE (
Fig. 3).
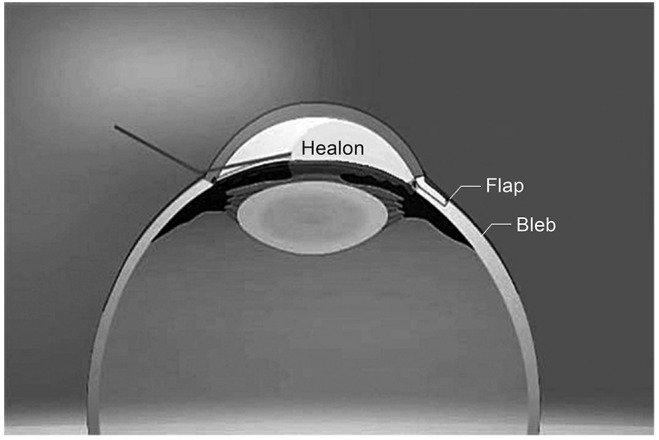 | Fig. 1At the end of conventional trabeculectomy approximately half of the anterior chamber space was filled with viscoelastics (Healon) via the paracentesis site. 
|
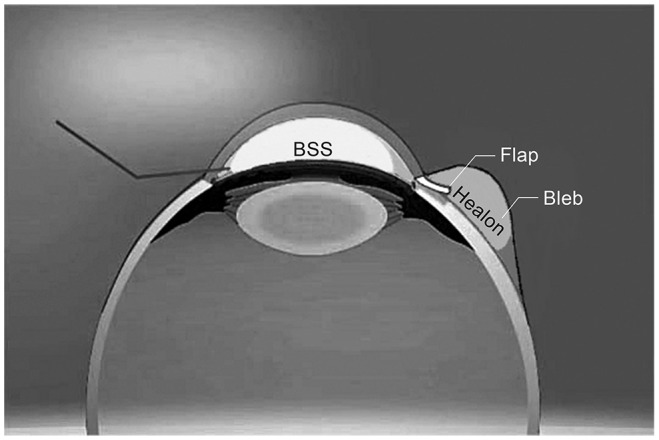 | Fig. 2A small amount of balanced salt solution (BSS) was injected into the anterior chamber via the same paracentesis site. This procedure induced migration of viscoelastics from the anterior chamber into the bleb space. Thus, the bleb was elevated by the underlying viscoelastics. 
|
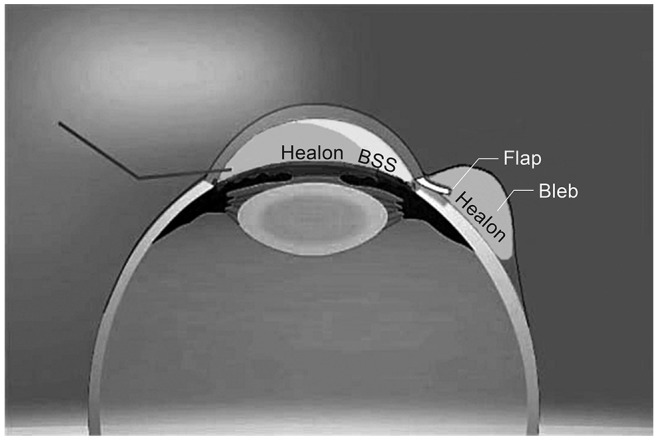 | Fig. 3Half of the anterior chamber space was again filled with viscoelastics. 
|
Analysis
Regular follow-up examinations were performed at 1 day, 1 week, 1 month, 3 months, 6 months, 9 months, and 1 year after surgery. If necessary, additional visits were scheduled. During all follow-up visits, the IOP was measured using Goldmann applanation tonometry, best-corrected visual acuity was determined, and the use of anti-glaucoma medications and the occurrence of complications were monitored. Overall success was defined as attainment of an IOP greater than 5 mmHg and less than 22 mmHg with or without the use of anti-glaucoma medication, the avoidance of additional glaucoma surgery, avoidance of revision of the original procedure, and the absence of serious complications. Complete success was considered to have been achieved when IOP could be controlled without the need for anti-glaucoma medication, whereas control of IOP with medication constituted qualified success. The success rate, number of postoperative IOP-lowering medications, and frequency of additional procedures such as AC reformation and laser suture lysis were compared between the CT and VAT groups. Kaplan-Meier survival analysis with log-rank testing was performed to compare cumulative complete success rates between two groups. All statistical analyses were performed using SPSS ver. 18.0 (SPSS Inc., Chicago, IL, USA). Informed consent was obtained from all patients. All procedures conformed to the Declaration of Helsinki and the study was approved by the institutional review board of the Asan Medical Center at the University of Ulsan (Seoul, Korea).
Go to :

Results
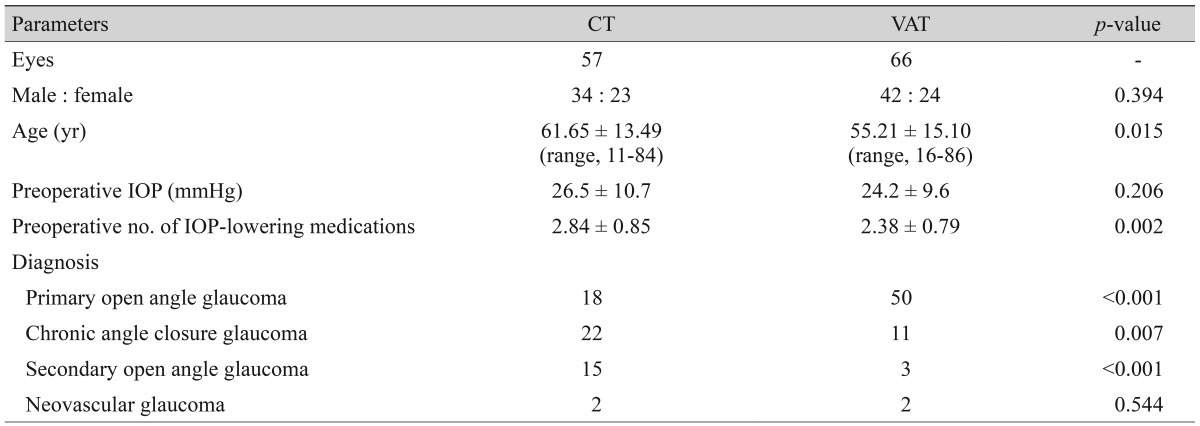
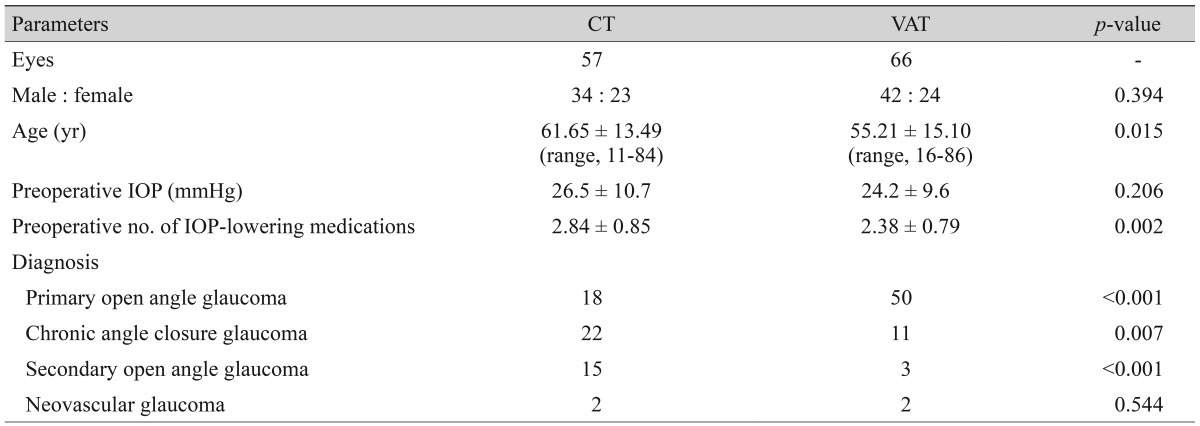
The mean age of the participants was 61.7 ± 13.5 years in the CT group and 55.3 ± 15.4 years in the VAT group. The proportion of patients with primary open angle glaucoma was significantly higher in the VAT group (CT, 37.6%; VAT, 75.8%;
p < 0.001). The preoperative demographics and diagnoses are described in
Table 1. The mean preoperative IOP was not different between the two groups (CT, 26.5 ± 10.7 mmHg; VAT, 24.2 ± 9.6 mmHg;
p = 0.206), but the number of IOP-lowering medications was greater in the CT group (CT, 2.84 ± 0.85; VAT, 2.38 ± 0.79;
p = 0.002).
Table 1
Characteristics of the CT and VAT groups

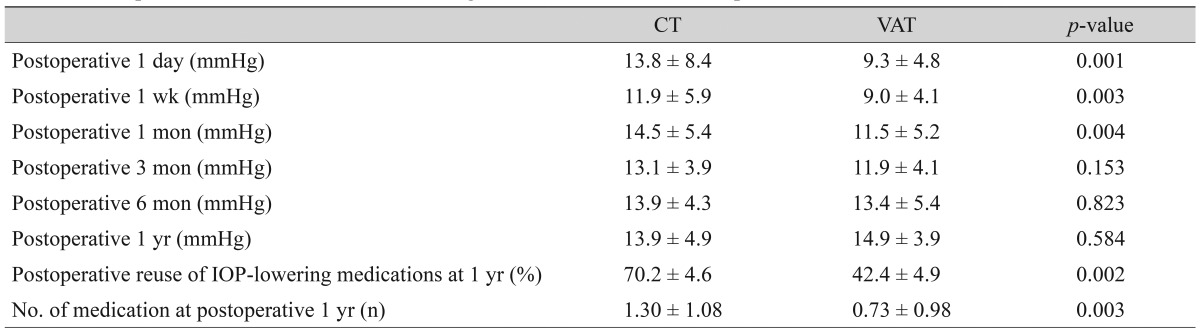
The mean postoperative IOP was significantly lower in the VAT group than in the CT group at postoperative 1 day, 1 week, and 1 month. At postoperative 3 months, 6 months, and 1 year, the mean IOP was not significantly different between the two groups. The mean postoperative IOP data and number of IOP-lowering medications are shown in
Table 2. The percentage of reuse of IOP-lowering medication and the number of IOP-lowering medications were significantly higher in the CT group than in the VAT group.
Table 2
Postoperative IOP and use of IOP-lowering medication at each follow-up visit

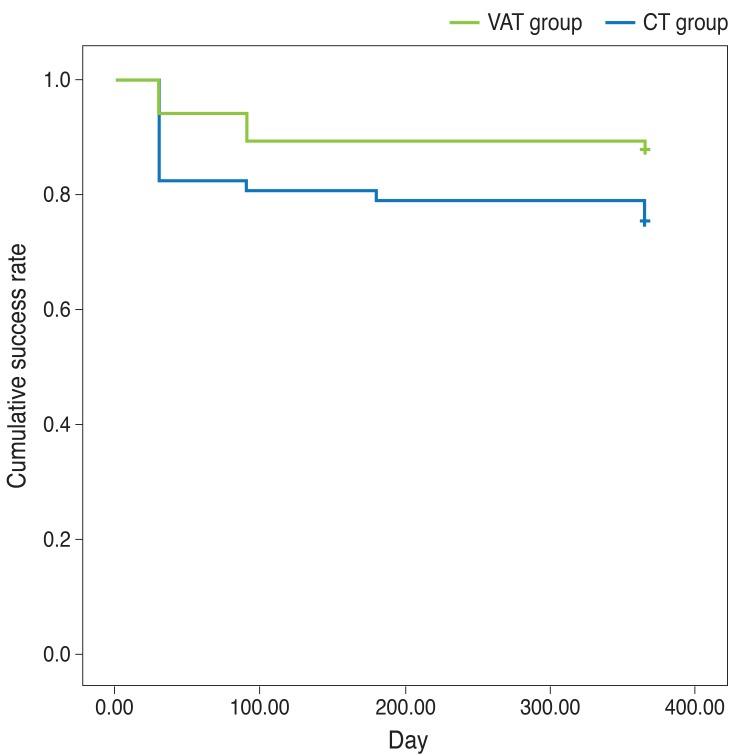
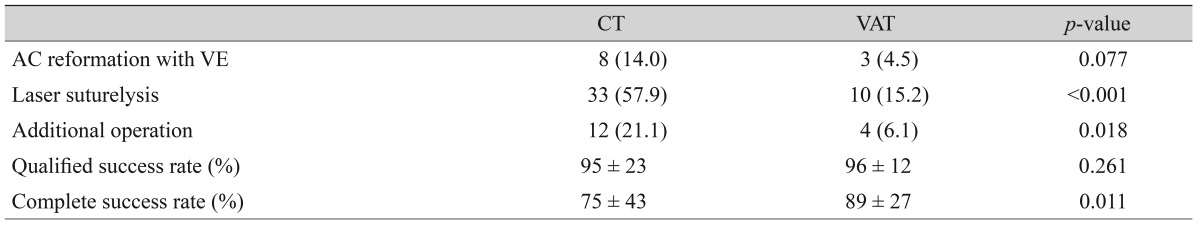
Among postoperative procedures, AC reformation with VE and laser suture lysis were less frequently performed in the VAT group although the former did not reach statistical significance (
p = 0.077,
p < 0.001). The complete success rate was significantly higher in the VAT group. The cumulative complete success rate was significantly higher in the VAT group than in the CT group (log rank test,
p = 0.042) (
Fig. 4). The postoperative clinical outcomes are shown in
Table 3.
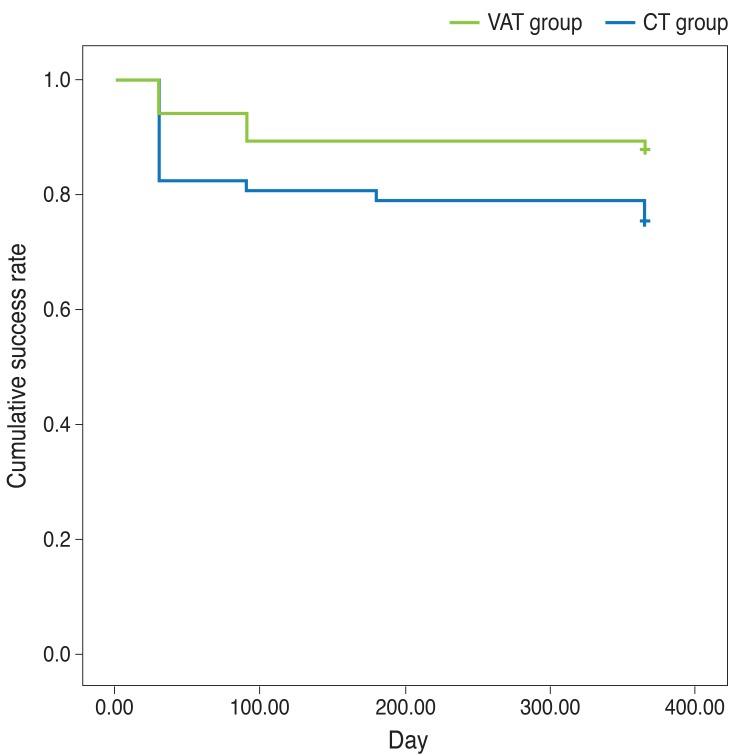 | Fig. 4The cumulative success rate of the viscoelastics-augmented trabeculectomy (VAT) and conventional trabeculectomy (CT) groups determined by Kaplan Meier Analysis. 
|
Table 3
Postoperative clinical outcomes

Go to :

Discussion
VE are routinely used in trabeculectomy as well as in other types of intraocular surgery. During CT, VE are used to prevent the sudden collapse of the AC and to protect the corneal endothelium. Since HA is the most widely used ingredient of VE and is a known anti-fibrotic agent, it is appropriate to try to expand the role of VE beyond their current use in CT. At the same time, VE within a bleb might function as a valve that can prevent overfiltration because VE would be absorbed more slowly than aqueous humor.
The results of the current study indicated that postoperative IOP was significantly lower in the VAT group in the early postoperative period. Despite lower IOPs in the VAT group, the frequency of AC reformation was lower in the VAT group, indicating that the insertion of VE in the bleb was effective in maintaining a lower level of IOP deep within the AC.
Although the absorption rate of VE under the subconjunctival space has not been reported, a rounder and more diffusely elevated bleb configuration was observed during the second to third postoperative weeks in eyes which underwent VAT, which may suggest an ongoing presence of VE within the bleb. It is speculated that an ongoing presence of VE within the bleb may prevent both AC collapse caused by overfiltration and adhesion of the subconjunctiva. The VAT group demonstrated a higher complete success rate and a less frequent use of anti-glaucoma medication. Thus, it is speculated that maintaining a lower IOP and avoiding a flat AC during the early postoperative period enhanced the surgical success rate in the VAT group.
One unexpected advantage of VAT was the reduced need for laser suture lysis. One potential explanation is that while the VE migrates from the AC to the bleb the scleral flap edge might be slightly lifted thereby allowing continuous movement of aqueous humor from the AC to the bleb. Thus, IOP was well controlled without the need for laser suture lysis in most of the cases. As VE remains within the bleb for an extended period, aqueous humor flow appears to be regulated to a certain extent.
This study was not a prospectively designed and randomized controlled study. We began to perform VAT cases in early 2011 and found the technique to be superior in terms of IOP control and postoperative complication management, and VAT has since become our standard treatment protocol. Given that we were aware of the superiority of VAT according to our preliminary results, it would have been unethical to randomize patients into two groups whereby one group was known to be receiving an inferior treatment. The lack of randomization is still, however, a limitation of the current study. These results should be interpreted cautiously since both the CT and VAT groups differed with respect to the proportion of preoperative diagnoses, the amount of glaucoma medication administered was different between the two groups, and the CT procedure was performed earlier than the VAT which may have increased the surgeon's experience in the VAT group. The other limitation of the current study would be the relatively shorter follow-up period.
Seprafilm, a bioresorbable transparent membrane made of HA, is used in trabeculectomy to prevent postoperative adhesion between the conjunctiva and sclera [
18]. The use of this product requires additional materials and time. Altering one's surgical technique as done here, however, requires no additional materials or cost and can be performed at the end of CT with a few minor procedural additions and in a short period of time. Therefore, we suggest that the technique of augmenting trabeculectomy with VE is effective for improving the surgical success rate.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download