Abstract
Purpose
To investigate the inhibitory effect of 0.02% mitomycin C on eyelash regrowth when injected to the eyelash hair follicle immediately after radiofrequency ablation.
Methods
We prospectively included 21 trichiasis patients from June 2011 to October 2012. Twenty eyes of 14 patients were treated with 0.02% mitomycin C to the hair follicle immediately after radiofrequency ablation in group 1, while radiofrequency ablation only was conducted in ten eyes of seven patients in group 2. Recurrences and complications were evaluated until six months after treatment.
Trichiasis is a condition of abnormally positioned eyelashes that grow toward the eyeball and contact the ocular surface [1]. This can cause corneal epithelial defects, corneal ulcer, and corneal scarring and may lead to severe vision loss [2]. Trichiasis can occur due to blepharoconjunctivitis, cicatrical pemphigoid, Stevens-Johnson syndrome, erythema multiforme, pseudomonas pemphigus, trauma, surgery, trachoma, among other reasons [2]. The global prevalence of trichiasis is high. Standard treatment involves removal or destruction of the affected eyelashes with epilation, radiofrequency ablation, cryotherapy, argon laser, surgical procedures, and other methods. However, widely acknowledged and effective treatment has not yet been established [3].
Mitomycin C is a metabolic antagonist extracted from Streptomyces caespitosus. This medication is a cytotoxic chemotherapy drug that shifts to an alkylating agent that is effective in all cell cycles of proliferative and non-proliferative cells. Mitomycin C was first introduced in the pterygium removal procedure in 1970 and has been widely applied in glaucoma surgery, treatment of conjunctiva and corneal epithelial tumors, refractive surgery, and other ophthalmological procedures in recent years [4].
In previous studies, the authors have reported the efficacy and safety of mitomycin C, which inhibits the regrowth of eyelashes, through epilation after treating mice with 0.04% mitomycin C [5]. The study aimed to verify the effect of locally injected 0.02% mitomycin C in conjunction with radiofrequency ablation in trichiasis patients.
The present study is a prospective and comparative study performed after gaining the approval of the Research Ethics Committee of Gyeongsang National University and the Korea Food and Drug Administration. The procedures used conformed to the tenets of the Declaration of Helsinki. All examinations and surgeries were conducted in the Department of Ophthalmology, Gyeongsang National University. The study involved 30 eyes of 21 patients diagnosed with trichiasis, and all surgical procedures were carried out by a single surgeon from June 2011 to October 2012. The study excluded patients younger than 13 years, and those who were pregnant or had cancer, severe cardiopulmonary disease, intellectual disability, or inflammatory ocular disease such as keratitis, scleritis, conjunctivitis, or blepharoconjunctivitis. An image of the anterior eye segment was collected in the trichiasis-affected region. Twenty-one volunteers were fully informed about the different treatment procedures and provided consent to be classified into group 1 (n = 14) with radiofrequency ablation and injection of 0.02% mitomycin C or group 2 (n = 7) with radiofrequency ablation.
Anesthesia was carried out by injecting 20 mg/mL lidocaine HCl and 0.018 mg/mL epinephrine in the surgical site. After flipping the lid margin to the far side of the eyeball, a sterilized epilation needle connected to a 3.8-MHz Ellman Surgitron was inserted into the eyelash root to a depth of 2 to 3 mm in the cut and coagulation mode (power = 3) in order to easily remove eyelashes, and the follicles were cauterized. In the mitomycin C group, 0.1 mL 0.02% mitomycin C was injected using a 27-gauge cannula arranged with a 1-mL syringe into the eyelash-removed follicles and left for two minutes after radiofrequency ablation. Subsequently, the follicles were washed with 10 mL normal saline. The procedure was completed by applying antibiotic ointment to the surgical site (Fig. 1).
After six postoperative months, medical records, the findings of slit-lamp biomicroscopy, imaging of the anterior eye segment, and the relapse of trichiasis were evaluated by comparison with the preoperative conditions. In addition, we evaluated complications associated with radiofrequency ablation and mitomycin C (Fig. 2).
From one group 1 patient with preoperative lower lid laxity, we were able to obtain tissues after radiofrequency ablation. The sample tissue was fixed with 2% glutaraldehyde, embedded with paraffin, and cut into sections. The tissue block was stained with hematoxylin-eosin and examined under an optical microscope.
SPSS ver. 18.0 (SPSS Inc., Chicago, IL, USA) was used for the statistical analysis. Mann-Whitney U-test and Fisher's exact test were performed to verify statistical significance.
A total of 200 eyelashes were investigated in 21 patients with trichiasis. The mean age of the subjects was 58.1 ± 18.3 years. Females and males accounted for 67% and 33% of patients, respectively. The mean age was 64.7 ± 10.1 in group 1 and 45.71 ± 24.3 in group 2. The ratio of females was 64.3% in group 1 and 71.4% in group 2. The number of eyelashes in the affected eye was 5.8 ± 3.2 in group 1 and 8.4 ± 6.6 in group 2. No significant differences were found in age, sex, and the average number of eyelashes between the two groups (Table 1). A total of 116 eyelashes underwent treatment in 20 eyes in group 1. Trichiasis recurred in 19 eyelashes (16.4%). A total of 84 eyelashes underwent treatment in ten eyes in group 2. Trichiasis recurred in 51 eyelashes (60.7%). In the comparison of the two groups, more favorable results were shown in group 1 where 0.02% mitomycin C was applied (p = 0.005) (Table 2).
In one case in group 1, histological examination was performed using follicle tissue obtained during eyelid surgery conducted six months after treatment. Optical microscopic findings revealed structural damage in all four examined follicles, and thickened follicle epithelium and sebaceous glands were observed after the regeneration process. Dermal papilla tissues were destroyed and not observed in three follicles. However, dermal papillae remained in the remaining follicle, and growth of the hair shaft was observed (Fig. 3).
No patients showed complications related to mitomycin C such as keratoconjunctival erosion or scleromalacia in the cornea, sclera, or conjunctiva. No specific complication was observed in the eyelid area where mitomycin C was injected. Eyelid notch, which is known to be a complication of radiofrequency ablation, was not found in group 1 with the use of mitomycin C but was detected in two patients in group 2. Therefore, there is a possibility that the wound site in the mitomycin C applied group might have been more clearly recovered (Fig. 4).
The standard treatments for trichiasis are epilation, radiofrequency ablation, cryotherapy, argon laser, and surgical procedures. However, a widely acknowledged and effective treatment has not yet been established [3]. Epilation is more commonly used because of its convenience and low risk. This method temporarily relieves the pain of corneal abrasion. Removed eyelashes usually regrow within 4 to 6 weeks after removal. In this process, shortened eyelashes may induce continuous corneal injury. West et al. [6] reported a high rate of corneal opacity in patients who underwent epilation in long-term treatment.
Radiofrequency ablation is another method that can be performed as swiftly as outpatient treatment. The success rate was reported to be 60% to 67% in a single session of radiofrequency ablation [3,7]. According to a study by Han and Doh [8], the success rate of follicle trephination combined with electrocautery was 83%. Sakarya et al. [9] reported success rates of 66.6% in a single session of electrocautery using an ultrafine needle and 100% with two to three sessions. Potential complications were edema, erythema, hematoma, eyelid notch, and others [7].
Various success rates for cryotherapy have been reported worldwide, ranging from a low of 34% [10] to a high of 71% to 90% [11-14]. However, the incidence of complications generated by cryotherapy has been reported at 26% [8,10-14].
Several studies have examined the treatment of trichiasis using argon or diode laser. Laser therapies have exhibited a success rate of 39% to 88% without relapse [1,15-17]. Application of more than three laser treatments increased the success rate to 91.3% to 100% [17,18]. Laser therapy can be usefully implemented in ocular pemphigoid patients who have mild trichiasis or need to avoid inflammation [1,16]. However, the disadvantages of this treatment are the high costs of the medical instruments and the association of complications such as eyelid notch, skin depigmentation, and dimpling of the skin [1,15,17,19].
A large number of treatment methods have been proposed, such as anterior and posterior lamellar repositioning, tarsal fracture, tarsal marginal rotation-associated full-thickness eyelid resection, and others. The majority of those procedures primarily correct entropion, and the recurrence rate has been reported to range between 3% to 62% [20-27]. All surgical procedures are influenced by various factors, including patient choice and the abilities of surgeons. The chief limitations are the time and cost burdens and the invasive nature of the procedure.
Mitomycin C inhibits the proliferation of fibroblasts, and it has been commonly used in ophthalmology to prohibit scarring of the surgical area by inducing apoptosis. Moreover, inflammatory complications could occur such as anterior and posterior scleritis, acute toxicity and local stimulation, delayed orbital fibrosis, and others. In a recent study, mitomycin C increased IL-8 (a chemokine of macrophages and chemical attractant) and MCP-1 (an activator of lymphocyte and neutrophils and chemical attractant) in the fibroblasts of the cornea and generated an inflammatory reaction [28,29]. Radiofrequency ablation incurs heat injuries, including bleeding, edema, and others, and severe inflammatory reaction occurs due to lymphocytes, macrophages, and foreign body giant cells. Those inflammatory reactions ultimately destruct matrix and hair papilla, and follicles are replaced with eosinophil collagen, characteristic of scar tissue [30]. In this process, mitomycin C is anticipated to accelerate the destruction of follicles by intensifying inflammatory reactions. In addition, the injection of mitomycin C is thought to be effective in prohibiting follicle regrowth by inducing programmed cell death. Previously, our study with rats verified that application of 0.04% mitomycin C generates the destruction and edema of wrinkles in the mitochondria of follicles following simple epilation [5].
Eyelid notch occurred in two patients in group 2 without the use of mitomycin C. In contrast, no injury in the eyelid structure was detected in group 1 with the use of mitomycin C. Histological findings revealed structural changes in follicles in group 1 where follicle tissues were obtainable. However, scarring and destruction in the surrounding tissue were not found to be severe (Fig. 3). Mitomycin C is thought to inhibit fibrosis and might be effective in preventing structural injuries, including postoperative eyelid notch, ectropion of the eyelid, and others.
Mitomycin C drops were locally applied to the eyes as an adjuvant therapy group after glaucoma filtering surgery or pterygium removal procedure. Consequently, associated complications were reported to be dry eye syndrome, superficial punctate keratitis, allergic reaction, punctum obstruction, keratomalacia and scleromalacia, surgical wound infection and dehiscence, and others [31-33]. Those complications could be avoided by using a low concentration of mitomycin C with thorough monitoring and treatment [34]. In the present study, no complications were detected after injecting 0.02% mitomycin C once for two minutes.
A nearly 100% success rate was acquired by repeatedly performing radiofrequency treatment in some studies [7,9]. However, repeated radiofrequency treatment is difficult to carry out due to high cost, pain, and other problems that influence the compliance of patients in actual clinical settings. In a recent study on eyelash trephination combined with electrocautery, the success rate was 83% [8], aligning with the success rate (83.6%) of the present study using the simpler additional injection of mitomycin C. In addition, this treatment is anticipated to be effective in reducing postoperative complications that occur due to eyelid injury after radiofrequency treatment.
There were some limitations to the present study. First, the authors were unable to verify if mitomycin C temporarily prohibited the division of follicular cells or completely destructed follicles. Although the outcome is an absence of misdirected eyelashes, the satisfaction of patients could be improved by extending the lack of symptoms for several months. Second, a small number of volunteers were included in the study. The six-month follow-up was also thought to be short. However, the average eyelash growth cycle is about 90 days [35]. Therefore, the period of postoperative six months was thought to be sufficient for evaluating the direct injury of follicles generated by mitomycin C in conjunction with radiofrequency ablation.
Local injection of 0.02% mitomycin C could be applied as an effective adjuvant therapy, increasing the success rate of radiofrequency ablation in patients with trichiasis. Mitomycin C may help to prevent the deformity of eyelids by facilitating the recovery of wounds caused by radiofrequency ablation.
Figures and Tables
Fig. 1
(A) After flipping the lid margin to the far side of the eyeball, a sterilized epilation needle connected to a 3.8-MHz Ellman Surgitron was inserted into the root of the eyelashes to a depth of 2 to 3 mm in the cut and coagulation mode (power = 3) in order to easily remove eyelashes, and follicles were cauterized. (B) After that, 0.1 mL 0.02% mitomycin C was injected by attaching a 27-gauge cannula to a 1-mL syringe in eyelash-removed follicles and left for two minutes after radiofrequency ablation.

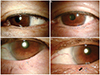
Fig. 2
(A) An image of the preoperative eyelashes (black arrows). (B) An image of eyelashes six months after the operation.

Fig. 3
Optical microscopic findings revealed structural damage in all four follicles. Thickened follicle epithelium and sebaceous glands were observed after the regeneration process. (A-C) The dermal papillae were destroyed and not found in three hair follicles. (D) However, dermal papillae remained in the remaining follicle, and growth of the hair shaft was observed (H&E, ×100).

Fig. 4
Patient in group 1. (A) Image of the preoperative eyelid. (B) There was no deformity or scarring in the eyelid at six postoperative months. Patient in group 2. (C) Image of the preoperative eyelid. (D) Notching in the eyelid at six postoperative months (black arrow).
References
1. Gossman MD, Yung R, Berlin AJ, Brightwell JR. Prospective evaluation of the argon laser in the treatment of trichiasis. Ophthalmic Surg. 1992; 23:183–187.
2. Basar E, Ozdemir H, Ozkan S, et al. Treatment of trichiasis with argon laser. Eur J Ophthalmol. 2000; 10:273–275.
3. Kezirian GM. Treatment of localized trichiasis with radiosurgery. Ophthal Plast Reconstr Surg. 1993; 9:260–266.
4. Kunitomo N, Mori S. Studies on pterygium: report IV. A treatment of the pterygium by mitomycin C installation. Acta Soc Ophthalmol Jpn. 1963; 67:601–607.
5. Kim CR, Yoo WS, Kim KH, Seo SW. Effects of mitomycin C on eyelash-regrowth in epilated rats. J Korean Ophthalmol Soc. 2011; 52:1501–1506.
6. West ES, Munoz B, Imeru A, et al. The association between epilation and corneal opacity among eyes with trachomatous trichiasis. Br J Ophthalmol. 2006; 90:171–174.
7. Kormann RB, Moreira H. Treatment of trichiasis with high-frequency radio wave electrosurgery. Arq Bras Oftalmol. 2007; 70:276–280.
8. Han JH, Doh SH. Treatment for trichiasis through a combination of eyelash trephination and electrocautery. Acta Ophthalmol. 2012; 90:e211–e213.
9. Sakarya Y, Sakarya R, Yildirim A. Electrolysis treatment of trichiasis by using ultra-fine needle. Eur J Ophthalmol. 2010; 20:664–668.
10. Elder MJ, Bernauer W. Cryotherapy for trichiasis in ocular cicatricial pemphigoid. Br J Ophthalmol. 1994; 78:769–771.
11. Johnson RL, Collin JR. Treatment of trichiasis with a lid cryoprobe. Br J Ophthalmol. 1985; 69:267–270.
12. Sullivan JH, Beard C, Bullock JD. Cryosurgery for treatment of trichiasis. Trans Am Ophthalmol Soc. 1976; 74:189–202.
13. Sullivan JH. The use of cryotherapy for trichiasis. Trans Sect Ophthalmol Am Acad Ophthalmol Otolaryngol. 1977; 83(4 Pt 1):708–712.
14. Wood JR, Anderson RL. Complications of cryosurgery. Arch Ophthalmol. 1981; 99:460–463.
15. Sharif KW, Arafat AF, Wykes WC. The treatment of recurrent trichiasis with argon laser photocoagulation. Eye (Lond). 1991; 5(Pt 5):591–595.
16. Bartley GB, Lowry JC. Argon laser treatment of trichiasis. Am J Ophthalmol. 1992; 113:71–74.
17. Oguz H, Aras C, Ozdamar A. Thermoablation treatment for trichiasis in trachoma using the semiconductor diode pumped laser. Eur J Ophthalmol. 1999; 9:85–88.
18. Ladas ID, Karamaounas N, Vergados J, et al. Use of argon laser photocoagulation in the treatment of recurrent trichiasis: long-term results. Ophthalmologica. 1993; 207:90–93.
19. Yung CW, Massicotte SJ, Kuwabara T. Argon laser treatment of trichiasis: a clinical and histopathologic evaluation. Ophthal Plast Reconstr Surg. 1994; 10:130–136.
20. Bi YL, Zhou Q, Xu W, Rong A. Anterior lamellar repositioning with complete lid split: a modified method for treating upper eyelids trichiasis in Asian patients. J Plast Reconstr Aesthet Surg. 2009; 62:1395–1402.
21. Hintschich CR. "Anterior lamellar repositioning" for correction of entropion of the upper eyelid. Ophthalmologe. 1997; 94:436–440.
22. Gower EW. Trichiasis: making progress toward elimination. Int Ophthalmol Clin. 2007; 47:77–86.
23. Burton M, Solomon A. What's new in trichiasis surgery? Community Eye Health. 2004; 17:52–53.
24. Khandekar R, Al-Hadrami K, Sarvanan N, et al. Recurrence of trachomatous trichiasis 17 years after bilamellar tarsal rotation procedure. Am J Ophthalmol. 2006; 141:1087–1091.
25. Thanh TT, Khandekar R, Luong VQ, Courtright P. One year recurrence of trachomatous trichiasis in routinely operated Cuenod Nataf procedure cases in Vietnam. Br J Ophthalmol. 2004; 88:1114–1118.
26. Khandekar R, Mohammed AJ, Courtright P. Recurrence of trichiasis: a long-term follow-up study in the Sultanate of Oman. Ophthalmic Epidemiol. 2001; 8:155–161.
27. Bowman RJ, Faal H, Jatta B, et al. Longitudinal study of trachomatous trichiasis in The Gambia: barriers to acceptance of surgery. Invest Ophthalmol Vis Sci. 2002; 43:936–940.
28. Chou SF, Chang SW, Chuang JL. Mitomycin C upregulates IL-8 and MCP-1 chemokine expression via mitogen-activated protein kinases in corneal fibroblasts. Invest Ophthalmol Vis Sci. 2007; 48:2009–2016.
29. Chang SW, Chou SF, Yu SY. Dexamethasone reduces mitomycin C-related inflammatory cytokine expression without inducing further cell death in corneal fibroblasts. Wound Repair Regen. 2010; 18:59–69.
30. Kligman AM, Peters L. Histologic changes of human hair follicles after electrolysis: a comparison of two methods. Cutis. 1984; 34:169–176.
31. Khong JJ, Muecke J. Complications of mitomycin C therapy in 100 eyes with ocular surface neoplasia. Br J Ophthalmol. 2006; 90:819–822.
32. Singh G, Wilson MR, Foster CS. Long-term follow-up study of mitomycin eye drops as adjunctive treatment of pterygia and its comparison with conjunctival autograft transplantation. Cornea. 1990; 9:331–334.
33. Bindlish R, Condon GP, Schlosser JD, et al. Efficacy and safety of mitomycin-C in primary trabeculectomy: five-year follow-up. Ophthalmology. 2002; 109:1336–1341.
34. Frucht-Pery J, Ilsar M. The use of low-dose mitomycin C for prevention of recurrent pterygium. Ophthalmology. 1994; 101:759–762.
35. Thibaut S, De Becker E, Caisey L, et al. Human eyelash characterization. Br J Dermatol. 2010; 162:304–310.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download