Abstract
Purpose
To describe the long-term results of deep sclerectomy with collagen implant (DSCI) with or without adjuvant mitomycin C in Korean patients with primary or secondary open-angle glaucoma (OAG).
Methods
This retrospective review was comprised of 65 Korean patients who received DSCI with or without adjuvant mitomycin C due to primary or secondary OAG. Patients were followed for 72 months after surgery. Complete success was defined as intraocular pressure (IOP) <21 mmHg without medication and qualified success was defined as IOP <21 mmHg with or without medication.
Results
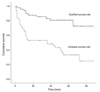
Mean postoperative follow-up period was 53.0 ± 16.2 months. Mean IOP was 30.5 ± 11.7 mmHg preoperatively, 8.4 ± 4.3 mmHg at postoperative day one and 13.4 ± 3.8 mmHg 60 months after surgery. The mean number of glaucoma medications was decreased from 3.6 ± 1.1 to 1.6 ± 1.3 at 60 months after the operation. Complete and qualified success rates were 36.7% and 79.6% at postoperative 60 months, respectively (Kaplan-Meier survival curve). No shallow or flat anterior chamber, endophthalmitis, or surgery-induced significant cataract was observed.
Deep sclerectomy (DS), one of the non-penetrating glaucoma surgeries, has been reported to be a safe and effective surgical procedure which provides long-term intraocular pressure (IOP) control in the management of open-angle glaucoma. Several studies comparing surgical outcomes of DS with those of trabeculectomy have also shown that DS provides less but comparable IOP reduction with fewer complications [1,2]. However, the surgical outcomes of DS may have racial differences. Although East Asian eyes are reported to ethnically differ in many aspects from other races, there are few reports about the long-term surgical results of DS in Asian populations. This report evaluates the long-term results of DS with small collagen implants in Korean open-angle glaucoma (OAG) patients.
After the approval of the institutional review board, 65 subjects with planned deep sclerectomy with collagen implant (DSCI) with or without the adjunctive use of mitomycin C due to primary and secondary OAG were retrospectively collected. All subjects were Korean (single ethnic group).
All surgical procedures were performed by a single surgeon. A one-third scleral thickness, limbal-based, 5.0 mm × 5.0 mm scleral flap was dissected. In the cases using mitomycin C, pieces of surgical sponge soaked with 0.2 mg/mL mitomycin C were applied to the exposed sclera for three minutes and washed out with 10 mL saline irrigation. In certain cases of thin conjunctiva (n = 4) or history of hypotony in the opposite eye (n = 2), mitomycin C was not applied. A hexahedron piece of deep sclera was then removed, leaving a thin scleral layer. Schlemm's canal was de-roofed at the level of the scleral spur. The dissection was continued until the trabeculo-Descemet's membrane (TDM) was exposed. The inner wall of Schlemm's canal and the juxtacanalicular meshwork was peeled off. A synthetic absorbable collagen implant (Ultraplug; Surgical Specialties, Reading, PA, USA) of a cylindrical shape measuring 0.4 mm in diameter and 2.0 mm in length was placed in the center of the deep sclerectomy and sutured with 10-0 nylon. The superficial scleral flap was repositioned over the implant and sutured with 10-0 nylon.
Surgery was considered a complete success when IOP was less than 21 mmHg without anti-glaucoma medication or laser goniopuncture, and a qualified success when medication or laser goniopuncture was necessary. It was considered a failure when an eye required further drainage surgery or lost light perception. Goniopuncture with a neodymium:YAG laser was performed when IOP failed to remain below 21 mmHg due to TDM fibrosis.
Kaplan-Meier survival curves were constructed using PASW ver. 18.0 (SPSS Inc., Chicago, IL, USA) for long-term success rate analysis.
Patient demographics are shown in Table 1. Of the 65 eyes initially selected for the initial review, 16 eyes were excluded from further analysis due to follow-up periods less than 12 months.
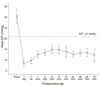
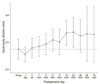
The IOP and best-corrected visual acuity changes are shown in Figs. 1 and 2. The mean IOP was 30.5 ± 11.7 mmHg (49 patients) preoperatively and 8.4 ± 4.3 mmHg one day postoperatively. However, as length out from surgery increased, the mean IOP was slightly increased to 13.2 ± 3.7 mmHg (25 patients) at 48 months and to 13.4 ± 3.8 mmHg (16 patients) at 60 months postoperatively. Complete success was 59.2% at 12 months but decreased to 36.7% at 60 months. Qualified success registered at 89.9% at 12 months and 79.6% at 60 months (Fig. 3). When we change the definition of success to an IOP level of 18 mmHg, complete and qualified success rates were slightly decreased to 34.7% and 75.5% 60 months postoperatively, respectively. The mean number of anti-glaucoma medications decreased from 3.6 ± 1.1 (49 patients) to 0.8 ± 1.4 (25 patients) at 48 months, then increased to 1.6 ± 1.3 (16 patients) at 60 months postoperatively (Fig. 4).
No shallow or flat anterior chamber, endophthalmitis, or surgery-induced significant cataract was observed. However, five eyes (10.2%) developed a progression of pre-existing cataract. Four eyes (8.2%) showed chronic hypotony lasting for more than two months. Goniopuncture was performed in 23 eyes (46.9%). Mean time between DSCI and goniopuncture was 4.7 ± 6.1 months. The rate of iris synechiae formation after laser goniopuncture was 5.4%. When the TDM was perforated, the procedure was converted to and completed as trabeculectomy. The conversion rate to trabeculectomy plateaued below 20% (Fig. 5).
Non-penetrating glaucoma surgery is technically more difficult to perform than conventional trabeculectomy, as it requires a longer learning curve [3-5]. Our experience shows a similar declining conversion rate as providers become more accustomed to the procedure.
The efficacy of IOP reduction after DSCI when compared to conventional trabeculectomy has been an issue [6,7] (Table 2). Shaarawy et al. [5] reported a higher success rate of DSCI compared to DS only [8]. In terms of not only success rate but also the number of anti-glaucoma medication after surgery, their report showed relatively desirable results. Lachkar et al. also described similar long term outcome (six years) of DS retrospectively. Chiselita found a small but statistically significant lower IOP in the trabeculectomy group, but had fewer complications in the DSCI group. It is obvious that we cannot directly compare the outcome of respective studies. However, many reports show that DSCI is better than DS only by means of success rate [9,10].
DSCI has non-penetrating characteristic though, in that it cannot be completely free from the nature of filtering surgery. Xu et al. [11] demonstrated the physiology of DS with porcine eyes. The major factors affecting postoperative outflow increase include the subconjunctival pathway, the functional deep scleral lake and the opening of Schlemm's canal.
In the past few years, it was discovered by authorities that the major late complication of DSCI was the loss of its efficacy [12]. This study found that 46% of eyes eventually needed goniopuncture at a mean post-operative period of 4.7 ± 6.1 months. It has been speculated that an early (less than nine months after the initial procedure) necessity for goniopuncture was because of the lack of surgical dissection during the initial procedure and when the necessity arose late in the course of follow-up, it was probably due to fibrosis of the TDM [5].
This differs from the findings of the present study. Most eyes requiring goniopuncture showed good filtration and low IOPs immediately after the initial DSCI procedure. We believe that this study group, as a single ethnic group, may show differences in patterns of postoperative fibrosis. This ethnic characteristic is also evident in the rate of iris synechiae formation after laser goniopuncture. The present study shows a significantly higher rate of synechiae formation at 5.4% that needed reduction by laser synechiolysis and peripheral iridectomy compared to a previous report [13]. The authors presume an ethnic predisposition to inflammation leading to excessive fibrosis after laser procedures involving uveal tissue in Koreans. Mermoud et al. [14] described the immediate success rate of goniopuncture as 83% with no iris synechiae. In fact, it is not always clear whether the iris synechiae was developed by the laser goniopuncture or by the surgery (DS) itself. For example, Moreno-Montanes et al. [15] reported that nine eyes (8.49%, total 106 eyes) showed iris synechiae after DS only.
Shallower anterior chambers and more reaction to light may also affect postoperative results. According to the study by Oh et al. [16], no statistically significant difference was found between the angle width of African-Americans, Caucasians and Far East Asians, however, the iris attaches to the scleral wall more anteriorly in Asian populations. Wang et al. [17] noted that Chinese populations had a smaller angle recess area and trabecular-iris space area, but greater dark-to-light changes in angle opening distance and the trabecular-iris space area. The answer warrants future study, which may possibly involve anterior chamber depth measurements.
Other possible reasons for the lower success rate include higher preoperative IOP level and a much greater number of preoperative glaucoma medications (Table 2). It has already been known that the eye of the patient who has higher IOP at diagnosis shows a lower success rate of trabeculectomy [18,19]. Additionally, those using two or more topical medications were more at risk of failure [18]. These might be applicable to predict outcome of DSCI. Moreover, the different proportion of uveitic glaucoma, which has a relatively poor outcome, could influence the lower success rate [18].
In conclusion, these results show that DSCI in Korean glaucoma patients can have a relatively lower complete success rate and tolerable qualified success rate compared to the outcome of other previous studies. The structural difference in anterior segment (in relation to ethnicity), higher preoperative IOP level, and increased number of preoperative anti-glaucoma eyedrops are the possible factors leading to a lower success rate.
Figures and Tables
Table 2
Comparisons of variable parameters at 60 months postoperative deep sclerectomy with collagen implant with different meta-analysis articles

FU = follow up; Preop = preoperative; Postop = postoperative; IOP = intraocular pressure.
*Complete success rate is defined as the proportion of subjects that showed IOP ≤21 mmHg without any IOP lowering medication, and qualified success rate is defined as IOP ≤21 mmHg with any IOP lowering medication at 60 months after surgery.
†Complications include aggravation of preexisting cataract, hyphema, hypotony associated complication.
Acknowledgements
This study was supported by a grant of the Korea Health Technology R&D Project, Ministry of Health and Welfare, Republic of Korea (A101727).
References
1. Watson PG, Jakeman C, Ozturk M, et al. The complications of trabeculectomy (a 20-year follow-up). Eye (Lond). 1990. 4(Pt 3):425–438.
2. El Sayyad F, Helal M, El-Kholify H, et al. Nonpenetrating deep sclerectomy versus trabeculectomy in bilateral primary open-angle glaucoma. Ophthalmology. 2000. 107:1671–1674.
3. Bauchiero L, Demarie A, Belli L, Brogliatti B. Deep sclerectomy and viscocanalostomy: critical revision of the results obtained during the learning curve. Acta Ophthalmol Scand Suppl. 2002. 236:64–66.
4. Mermoud A, Schnyder CC, Sickenberg M, et al. Comparison of deep sclerectomy with collagen implant and trabeculectomy in open-angle glaucoma. J Cataract Refract Surg. 1999. 25:323–331.
5. Shaarawy T, Mansouri K, Schnyder C, et al. Long-term results of deep sclerectomy with collagen implant. J Cataract Refract Surg. 2004. 30:1225–1231.
6. Shaarawy T, Karlen M, Schnyder C, et al. Five-year results of deep sclerectomy with collagen implant. J Cataract Refract Surg. 2001. 27:1770–1778.
7. Lachkar Y, Neverauskiene J, Jeanteur-Lunel MN, et al. Nonpenetrating deep sclerectomy: a 6-year retrospective study. Eur J Ophthalmol. 2004. 14:26–36.
8. Hamel M, Shaarawy T, Mermoud A. Deep sclerectomy with collagen implant in patients with glaucoma and high myopia. J Cataract Refract Surg. 2001. 27:1410–1417.
9. Shaarawy T, Nguyen C, Schnyder C, Mermoud A. Comparative study between deep sclerectomy with and without collagen implant: long term follow up. Br J Ophthalmol. 2004. 88:95–98.
10. Shaarawy T, Mermoud A. Deep sclerectomy in one eye vs deep sclerectomy with collagen implant in the contralateral eye of the same patient: long-term follow-up. Eye (Lond). 2005. 19:298–302.
11. Xu W, Yao K, Wu W, et al. Change in outflow pathway of porcine eyes in vitro by nonpenetrating filtering surgery. Can J Ophthalmol. 2010. 45:632–636.
12. Sarodia U, Shaarawy T, Barton K. Nonpenetrating glaucoma surgery: a critical evaluation. Curr Opin Ophthalmol. 2007. 18:152–158.
13. Kim CY, Hong YJ, Seong GJ, et al. Iris synechia after laser goniopuncture in a patient having deep sclerectomy with a collagen implant. J Cataract Refract Surg. 2002. 28:900–902.
14. Mermoud A, Karlen ME, Schnyder CC, et al. Nd:Yag goniopuncture after deep sclerectomy with collagen implant. Ophthalmic Surg Lasers. 1999. 30:120–125.
15. Moreno-Montanes J, Rebolleda G, Munoz-Negrete FJ. Prognostic value of gonioscopy after deep sclerectomy. Eur J Ophthalmol. 2007. 17:702–708.
16. Oh YG, Minelli S, Spaeth GL, Steinman WC. The anterior chamber angle is different in different racial groups: a gonioscopic study. Eye (Lond). 1994. 8(Pt 1):104–108.
17. Wang D, Chiu C, He M, et al. Differences in baseline dark and the dark-to-light changes in anterior chamber angle parameters in whites and ethnic Chinese. Invest Ophthalmol Vis Sci. 2011. 52:9404–9410.
18. Landers J, Martin K, Sarkies N, et al. A twenty-year follow-up study of trabeculectomy: risk factors and outcomes. Ophthalmology. 2012. 119:694–702.
19. Fontana H, Nouri-Mahdavi K, Caprioli J. Trabeculectomy with mitomycin C in pseudophakic patients with open-angle glaucoma: outcomes and risk factors for failure. Am J Ophthalmol. 2006. 141:652–659.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download