Infectious scleritis accounts for about 5% to 10% of all cases of anterior scleritis. It should be suspected in patients with anterior scleritis and a recent history of trauma, ocular surgery, recurrent attacks of herpetic eye disease, or a systemic review consistent with infection. Bacteria, fungi, viruses and parasites have been implicated as causes of infectious scleritis [1].
Nocardia asteroides is an aerobic, gram-positive, branching filamentous bacterium that is found in soil, dust, and decaying vegetable matter, although it has also been reported to be part of the normal conjunctival flora in some rural populations [2]. Nocardia may cause cutaneous, subcutaneous, lymphocutaneous, pulmonary, cerebral, and disseminated infections in humans [3]. Nocardial ocular infections most commonly cause keratitis, but scleritis and endophthalmitis have rarely been reported. In the presence of immunosuppressive therapy, nocardial ocular infections can be especially devastating [4].
Nocardial infections occasionally present as an infectious scleritis. Some of the predisposing factors identified include cataract surgery, scleral buckle surgery, trauma with vegetable matter, and soft contact lens-related keratitis with extension to the sclera [5]. This paper describes a case of culture-proven Nocardial necrotizing scleritis in a contact lens-wearing patient without an associated keratitis.
Case Report
A 52 year-old male presented with four weeks of pain, photophobia and redness in the right eye. The patient had been evaluated by three different ophthalmologists prior to his presentation and was referred for further management of a steroid unresponsive scleritis. The patient had been treated with topical ciprofloxacin 0.3%, Predforte 1%, and 80 mg of oral prednisone without improvement over a two-week period.
The patient's past medical history was significant for gout and hypertension. The patient was diagnosed with gout 25 years previous, and he averaged 1-2 gouty attacks in his feet each year. He denied smoking or alcohol/drug use and any history of ocular surgery or trauma. The patient worked as a plumber and had worn soft disposable contact lenses for 20 years. He stated that he was compliant with proper contact lens care.
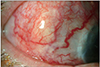
On examination, the patient's visual acuity was 20 / 100 in the right eye and 20 / 20 in the left eye. He had moderate right eyelid edema. Extraocular muscles and confrontation visual fields were normal in both eyes. His pupils reacted normally, and his intraocular pressure was 12 mmHg in the right eye and 14 mmHg in the left eye. On slit lamp examination with attention to the right eye, the conjunctiva was heavily injected. There was an 8 × 4 mm avascular patch of sclera at 9 o'clock with supprative inflammatory debris encasing the temporal conjunctiva. There were moderate Descemet's folds on the temporal cornea, but no evidence of either keratitis or an epithelial defect. There was neovascularization of the peripheral cornea at 10 o'clock. The anterior chamber was without cells or flare, and there were no keratic precipitates present. These negative findings are illustrated in Fig. 1. The posterior segment was within normal limits in both eyes.
Previously performed serology demonstrated a normal complete blood count, comprehensive metabolic panel, uric acid level, and urinalysis. Antinuclear antibodies, rheumatoid factor, antineutrophil cytoplasmic antibodies, and anti-double stranded DNA antibodies were also negative. The patient was diagnosed with necrotizing scleritis, poorly responsive to moderately high doses of oral steroids. Autoimmune, metabolic, and infectious causes were all considered. A swab culture of the supprative material coating the conjunctiva of the right eye was performed. A chest X-ray, lysozyme, rapid plasma reagin, venereal disease research laboratory, immunoglobulin A/immunoglobulin G for varicella zoster virus and herpes simplex virus, and thyroid-stimulating hormone tests were ordered. The patient was continued on the 80 mg of oral prednisone and referred to a rheumatologist for consideration of cyclophosphamide induction pending negative culture and laboratory results.
At five days follow-up from initial presentation, there was no significant change in the patient's symptoms or examination. The chest X-ray and the above mentioned labs were within normal limits. However, the culture came back positive for Nocardia asteroides, for which the patient was started on oral Bactrim DS twice daily and topical 2.5% amikacin every two hours. The prednisone dose was reduced to 40 mg, and a tapering schedule was implemented.
At one-week follow-up from the positive culture, there was significant improvement in the patient's symptoms and labs. His visual acuity improved to 20 / 40, and he was subjectively less photophobic and without significant pain. The culture results demonstrated that the Nocardia asteroides complex was sensitive to both amikacin and Bactrim, as shown in Fig. 2.
At one-month follow-up, the patient's visual acuity was 20 / 25 and he remained pain-free. The patient was tapered off the oral prednisone, and his topical amikacin was reduced to twice daily. At three months follow-up, the patient's right eye was refracted to 20 / 20 and he remained pain-free. The topical amikacin and oral Bactrim were discontinued. These results are illustrated in Fig. 3. The patient continued to be infection-free at his one-year follow-up examination.
Discussion
Fewer than ten cases of Nocardial necrotizing scleritis have been reported in the literature. The typical findings of Nocaridal necrotizing scleritis consist of a painful area of scleral inflammation with an associated avascular section with or without concomitant keratouveitis. The differential diagnoses include systemic inflammatory diseases such as rheumatoid arthritis and Wegener's granulomatosis; metabolic disorders such as thyrotoxicosis; skin diseases such as erythema nodosum and acne rosacea; and infectious diseases like syphilis, tuberculosis, herpes simplex, herpes zoster, pseudomonas, and Acanthamoeba species. Identifiable risk factors for the development of Nocardial scleritis include intraocular surgery [6], retinal detachment repair using a scleral buckle [7], trauma with vegetable matter [8], soft contact lens-related keratitis with extension to the sclera [9], and a subtenon triamcinolone acetonide injection [10]. One case of spontaneous Nocardia scleritis in a diabetic patient with no history of trauma or intraocular surgery has also been reported [11].
The case presented in this paper did not have any of the previously reported predisposing risk factors. Although the patient was a soft contact lens wearer, there was no evidence of an active or concomitant keratitis by which the infection may have extended from the sclera. The corneal findings were minimal and felt to be secondary to the adjacent scleritis. Since the patient in this report worked as a plumber, it is possible that he was exposed to Nocardia while on the job. However, even if the patient's conjunctiva became colonized by Nocardia, there would still need to be a mechanism by which the organism was able to penetrate the host's conjunctival defense. I propose that the patient's soft contact lens wear contributed to traumatic micro-abrasions on the conjunctival surface, thereby creating passageways for infectious organisms to bypass the host's conjunctival defense without first affecting the cornea. Although a contact lens-associated conjunctival micro-abrasion injury resulting in infection is an unlikely event, this seems to be the best causative explanation given this patient's history and findings. An alternative explanation would involve a significant work-related injury to the eye with or without prior conjunctival colonization by Nocardia, although this seems less likely given that the patient was a reliable historian and could not recount such a traumatic incident.
The choice of antibiotics in this case was based on the superior efficacy of oral Bactrim for nocardial ocular infections, as reported in the literature. Similar to the favorable responses using Bactrim reported by Ramos-Esteban et al. [5], Seth and Gaudio [10], and Choudhry et al. [11], this case demonstrated clinical improvement within one week and resolution within six months after initiation of Bactrim. Amikacin and minocycline have been recommended in cases of nocardial infection resistant to oral Bactrim DS [12].
In cases of necrotizing scleritis with an uncertain autoimmune etiology and poor response to both topical and oral corticosteroids as well as to standard antibiotics, it is important to obtain a culture. Timely recognition of necrotizing scleritis can prevent the development of scleral perforation and progression to endophthalmitis. Moreover, excellent communication among the ophthalmologist, the microbiology laboratory, and the rheumatologist is critical for the early diagnosis and treatment of Nocardial necrotizing scleritis in order to achieve the best possible outcome.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download