Abstract
Purpose
To elucidate risk potentiality of frontline radiotherapy associated cataracts in primary ocular adnexal mucosa-associated lymphoid tissue lymphoma (OAML).
Methods
Data from eight consecutive patients of 41 total OAML patients who had undergone cataract surgery after frontline radiotherapy were analyzed.
Results
The median patient age was 46 years (range, 36 to 69 years). The median total radiation dose was 3,780 cGy (range, 3,060 to 4,500 cGy), and the mean duration from radiation irradiation to cataract surgery was 36.60 ± 8.93 months. Preoperative lens opacification was primarily at the posterior lens subcapsule, and best-corrected visual acuity (BCVA) was 0.43 ± 0.21. Patients underwent the phacoemulsification surgical procedure with posterior chamber intraocular lens insertion. The average BCVA improved to 0.90 ± 0.14 after cataract surgery. Two patients underwent posterior continuous curvilinear capsulorhexis, and one had posterior capsule rupture. For posterior capsule opacification (PCO), three patients received Nd:YAG laser posterior capsulotomy after the initial surgery, and one patient is currently under consideration for laser posterior capsulotomy.
Conclusions
Radiotherapy increased posterior subcapsule opacification at a relatively young age in primary OAML. Phacoemulsification was a manageable procedure without severe complications, and final visual outcomes were good. However, because after-cataracts progressed earlier than did senile cataracts, close follow-up should be considered for PCO management.
Orbital lymphomas account for less than 1% of all non-Hodgkin's lymphomas in the body. The mucosa-associated lymphoid tissue (MALT) type of orbital lymphoma involving the ocular adnexa is the most common histological type [1-4]. Several studies have reported that MALT lymphomas constitute a higher proportion of primary ocular adnexal lymphomas (OAL) in Korea and Japan (80% to 98%) than in western countries (50% to 78%) [3,4] and that ocular adnexal MALT lymphoma (OAML) develops at a younger age at initial presentation in the Korean population [3].
Radiotherapy is known as a treatment modality with a high local control rate for primary OAML [1,2]. Despite its high local control rate, many studies have reported that radiation can induce complications such as cataracts, keratitis, dry eye syndrome, and retinopathy [1,5-8]. The lens of the eye is a radiosensitive structure [7]. It is well established that ionizing radiation exposure damages the dividing cells of the crystalline lens; differentiation and migration of the damaged cells to the posterior pole leads to posterior lens opacifications [7,9]. Cataracts can be induced by a single dose of <2 Gy, or 4 to 5.5 Gy in a fractionated dose, and toxicity is more common with doses >36 Gy [4-6,10-12]. While many studies have reported possible radiation doses for cataract formation [4-6,8], and some have reported that radiation can induce subcapsular opacification of the lens [9,13], we have limited detailed information about the characteristics of radiation-induced cataracts in OAML.
Although OAML is an indolent, non-fatal disease, and the overall survival rate of OAL is high (92.8%) [3], patients have the possibilities of surgery for radiation-induced cataract at a relatively young age [3,4]. Cataract operations can be stressful, especially in younger patients, and can decrease the quality of life due to early loss of accommodation and near vision. To our knowledge, there are no detailed reports on the characteristics of frontline radiotherapy associated cataracts. It would be helpful to analyze frontline radiotherapy associated cataracts in detail for OAML patients to maintain better quality of life.
The present retrospective study assessed the clinical characteristics of radiotherapy associated cataracts in eight consecutive patients with a diagnosis of OAML treated at Seoul St. Mary's Hospital. In particular, we investigated fractionation and total radiation dose, grade of lens opacification, intervals from first radiation exposure to cataract surgery, visual acuity changes before and after radiotherapy, cataract surgery techniques, final visual outcomes, and surgical complications.
A retrospective review was performed on the medical records of all patients who had undergone cataract surgery at the Department of Ophthalmology in Seoul St. Mary's Hospital after radiation therapy due to primary OAML from April 2005 through July 2010. Diagnosis and radiotherapy of OAML were performed at the Catholic University Lymphoma Group of Seoul St. Mary's Hospital. This study was approved by the institutional review board of the Catholic University of Korea and follows the principles of the Declaration of Helsinki.
Data collected included gender, affected eye, age at the time of OAML diagnosis, location of OAML, clinical stage of lymphoma, using both the Ann Arbor and TNM-based systems [14,15], best-corrected visual acuity (BCVA) at initial visit using the Snellen chart, and initial cataract status using the Lens Opacity Classification System III (LOCS III) cataract grading system.
In addition to radiation, treatment modalities were evaluated. Radiotherapy data included fractionation, daily radiation dose, total radiation dose, and BCVA just after radiotherapy. The interval between first radiation exposure and cataract operation, age at the cataract surgery, BCVA before the operation, and cataract status using LOCS III, were also evaluated.
Characteristics of cataracts included not only lens opacification, but also preoperative spherical equivalent (SE), preoperative corneal endothelial cell count, axial length, surgical techniques of lens removal, type of intraocular lens (IOL), postoperative uncorrected visual acuity (UCVA) and SE, and last-visit UCVA. The presence of after-cataracts and their durations were also checked to determine whether Nd:YAG laser posterior capsulotomy was needed.
Mean visual acuities (BCVA and UCVA) were determined using the Snellen chart. Statistical analyses were carried out using Excel 2007 (Microsoft Corporation, Redmond, WA, USA). A p-value <0.05 was considered significant.
Radiation treatment was administered five times weekly. Complete ocular examination was performed before cataract surgery. Corneal endothelial cell counts were performed using specular microscopy (Konan; Noncon Robo-CA-ICO-NAN Inc., Hyogo, Japan), and axial length was measured with IOL Master (Carl Zeiss, Jena, Germany). Cataract surgery was performed using a phaco machine (Alcon Infinity Vision System; Alcon, Hunenberg, Switzerland) with intraocular lens implantation into the capsular bag. Foldable acrylic IOL was inserted through a 2.0- or 3.0-mm clear corneal incision. During the operations of two patients, posterior continuous curvilinear capsulorhexis (PCCC) was manually performed. After surgery, patients used levofloxacin eye drops 4 times a day for 4 weeks and topical fluorometholone 4 times a day for at least 1 month. For management of after-cataracts, posterior capsulotomy was performed with an Nd:YAG laser (Optimis II, Quantel Medical, Cedex, France) at the outpatient department.
We followed-up with the patients every 3 months for the first 2 years after radiotherapy, every 4 months for the following 2 years, and every 6 months for the fifth year. In addition to adhering to their follow-up schedule, all patients were instructed to visit the Department of Ophthalmology whenever they had any ophthalmologic problem, including a decrease in visual acuity. After cataract surgery, we followed-up with them at postoperative day 1, 1 week, 1 month, and 2 months. Patients were then followed-up regularly every 3 months.
We identified 41 patients who had been treated with radiation for OAML and enrolled among them eight eyes from eight patients who had undergone cataract surgery due to radiation in OAML. There were seven women and one man; two were right eyes and six were left eyes. The median age was 46 years (range, 36 to 69 years). Pathologies of the patients were all reported as MALT lymphoma. The most common locations of OAML were the fornix conjunctiva (75%), especially the inferior side (Table 1). The clinical stages using the TNM-based system [14,15] were classified as T1N0M0 in seven patients and as T2N0M0 in one patient. All lymphomas were categorized as Stage IE using the Ann Arbor staging system. BCVAs at the initial visit were all determined to be 1.0 with the exception of one patient who had vision of 0.8. The mean lens opacification before any treatment using LOCS III was NO0.5, NC0.5, C0.5, P0.5.
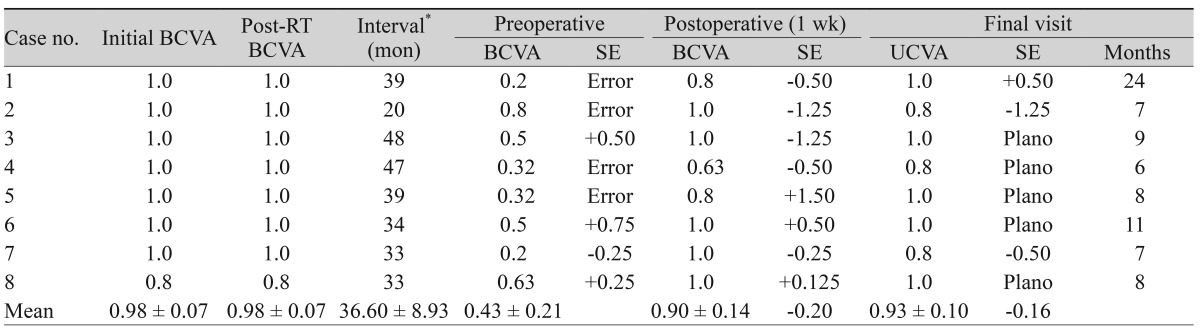
All patients were treated with radiation only and not with systemic therapy, such as chemotherapy. The median fractionation dose of radiotherapy was 20 cGy (range, 17 to 25 cGy), and the daily dose was 180 cGy in six patients and 200 cGy in two patients. The median dose of total radiation was 37.8 Gy (range, 30.6 to 45 Gy). The mean BCVA just after radiotherapy was 0.98 ± 0.07, which was the same visual acuity as that of the initial visit. The mean interval from the first radiation exposure to the cataract operation was 36.60 ± 8.93 months (Table 2). The median age of patients who underwent cataract surgeries was 46 years (range, 41 to 71 years).
The average BCVA just before cataract surgeries was 0.43 ± 0.21, and the average lens opacification using LOCS III was NO1.8, NC2.0, C1.9, P3.9. In all patients, posterior subcapsular cataract (P) increased in LOCS III grade by two or more units (Table 3). Half of the patients showed preoperative refractive errors due to cataracts. The median endothelial cell count was 2,621 cells/mm2 (range, 1,408 to 3,012 cells/mm2), and one patient had a very low corneal endothelial cell count of 1,408 cells/mm2 (case 7). The mean axial length was 23.69 ± 0.55 mm. All lenses were removed using the phacoemulsification technique, and foldable acrylic IOLs were inserted into the capsular bags. The characteristics of cataract and the types of IOLs inserted are summarized in Table 3.
For posterior subcapsular opacification (PSCO) management, PCCC was performed in two patients (case 3 and 7) during the surgery. Unfortunately, we experienced a minor posterior capsule (PC) tear during the operation for case 2, and an anterior vitrectomy was needed. After the operation, the patient complained of a floater for 1 month. Her final vision at postoperative 3 months was 0.8, and the floater symptom resolved. After-cataracts progressed in three patients within 4 months after the surgeries. In three of the cases (case 1, 2 months; case 5 and 8, 4 months), Nd:YAG laser posterior capsulotomy was performed. One case (case 6) is currently under consideration for laser posterior capsulotomy for glare vision, which occurred due to PCO at postoperative 8 months, although she has good visual acuity. The average UCVA 1 week after cataract surgery was 0.90 ± 0.14. We followed the patients for a median period of 5 months (range, 2 to 24 months) after cataract surgery. All patients (100%) experienced a return to their preoperative visual acuities (≥0.8), and the mean final UCVA was 0.93 ± 0.10. Changes in pre- and postoperative visual acuity with SE are shown in Table 2.
We report a series of eight primary OAML patients with radiotherapy associated cataracts that required surgery. Although the number of patients is small, this is the first report to elucidate risk potentiality of frontline radiotherapy associated cataract in primary OAML. Yoon et al. [3] reported that Korean MALT lymphoma patients are relatively young (mean age of 46 years). In this study, the median age at which surgery was performed was 46 years (range, 41 to 71 years); considering that cataract surgeries are usually performed in aged persons, the mid-forties is a relatively young age. Cataract surgery patients have problems with near vision without the help of near glasses due to decreased accommodative function, even though the surgery recovers visual acuity for distant vision. Thus, cataract surgery can be a stressful situation for relatively young patients, in whom surgery should be performed after radiation therapy.
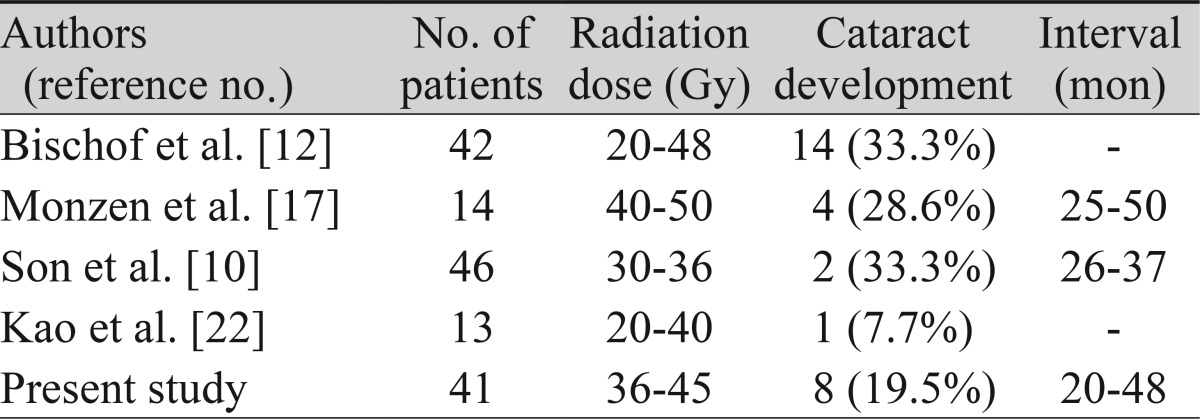
Cataracts can be induced by a rather low threshold radiation dose (below 0.5 Gy) [16], and many studies have warned that to prevent ophthalmic complications, the total radiation dose should not exceed 36 Gy [4-6,10-12]. Current National Cancer Center Network guidelines recommend radiotherapy of 20-30 Gy for initial treatment of early-stage nongastric extranodal marginal zone lymphoma of all sites, and re-irradiation for locally recurrent disease. Our median total radiation dose was 37.8 Gy (range, 30.6 to 45 Gy), which is a borderline dose for the recommended treatment. Although patients showed good vision with clear lenses at the initial ophthalmic examination, they lost vision and developed opacification after a mean interval of 36.6 ± 8.93 months from the first exposure to radiation. Ferrufino-Ponce and Henderson [7] reported that postradiation cataracts take an average of 42 months to develop (range, 1 month to 7 years). Son et al. [10] and Monzen and Hasebe [17] reported that especially in OAML patients, cataract development after radiation exposure ranged from 25 to 50 months and 26 to 37 months, respectively; these durations are similar to those of our study. Ferrufino-Ponce and Henderson [7] reported that clinically significant cataract formation after radiation therapy occurs in 40% to 50% of patients. Table 4 summarizes the literature regarding cataract development after radiation treatment in OAL patients; our study demonstrated an incidence of cataract formation of <20%.
The development of posterior subcapsular cataracts after radiation is widely accepted [7]. In our study, opacification of the posterior subcapsular area increased at least two grades using the LOCS III system in all patients. Cataractogenic radiation damage occurs at the "germinative zones" at the anterior surface, where dividing cells form a clear crystalline-protein fiber that migrates toward the posterior pole of the lens, the posterior subcapsular region [13]. However, Ferrufino-Ponce and Henderson [7] reported that there was evidence that cortical cataracts and nuclear sclerotic cataracts can also form in response to radiation.
During preparations for cataract surgeries, we found that 1 patient had a very low corneal endothelial cell count (1,408 cells/mm2) in the affected eye, but a much higher (over 2,000 cells/mm2) corneal endothelial cell count in the unaffected eye. Because we did not utilize specular microscopy at the initial visit prior to radiotherapy, we cannot prove the relationship between corneal endothelial damage and radiation irradiation. However, we carefully suggest that there might be a possibility of radiation-induced corneal endothelial damage via an unknown mechanism.
Due to PSCO, the posterior capsule was torn in one eye (12.5%); fortunately, we could insert an IOL into the capsular bag after anterior vitrectomy, and no further surgical management was needed. Wachtlin et al. [18] reported the same percentage (12.5%) of posterior capsular defects during radiation-induced cataract surgery in choroidal melanoma. Most patients should be under consideration for PSCO management during the operation.
Although there was the case of a PC tear during the operation and early development of after-cataracts, the final visual outcome of all patients was good and without complication. Usually, after-cataracts occur several years following surgery [19,20]. However, in this study, after-cataracts progressed in a very short period; within 4 months after the initial cataract operation, three patients (37.5%) had undergone Nd:YAG laser posterior capsulotomy. If after-cataracts progress, glare phenomena and reduced contrast can be problems in everyday life [21]; thus, patients who undergo cataract surgery due to radiation in OAML should be closely followed for early detection and management of after-cataracts.
In summary, radiotherapy in localized primary OAML mostly increased posterior subcapsular cataract at a relatively young age. It takes an average 3 years to develop cataract. Although it is possible that radiation damages not only the lens of the eye but also the cornel endothelium, which might lead to permanent corneal decompensation, the final postoperative visual outcomes of radiotherapy associated cataract surgeries were good. One of the important factors in determining cataract formation is the total radiation dose to the lens, and we should remember to always choose the lowest, most effective dose of radiation. To learn more about the complications caused by radiotherapy, prospective studies will be necessary.
References
1. Nam H, Ahn YC, Kim YD, et al. Prognostic significance of anatomic subsites: results of radiation therapy for 66 patients with localized orbital marginal zone B cell lymphoma. Radiother Oncol. 2009; 90:236–241. PMID: 18950885.

2. Yadav BS, Sharma SC. Orbital lymphoma: role of radiation. Indian J Ophthalmol. 2009; 57:91–97. PMID: 19237780.

3. Yoon JS, Ma KT, Kim SJ, et al. Prognosis for patients in a Korean population with ocular adnexal lymphoproliferative lesions. Ophthal Plast Reconstr Surg. 2007; 23:94–99.

4. Ferreri AJ, Dolcetti R, Du MQ, et al. Ocular adnexal MALT lymphoma: an intriguing model for antigen-driven lymphomagenesis and microbial-targeted therapy. Ann Oncol. 2008; 19:835–846. PMID: 17986622.

5. Stefanovic A, Lossos IS. Extranodal marginal zone lymphoma of the ocular adnexa. Blood. 2009; 114:501–510. PMID: 19372259.

6. De Cicco L, Cella L, Liuzzi R, et al. Radiation therapy in primary orbital lymphoma: a single institution retrospective analysis. Radiat Oncol. 2009; 4:60. PMID: 19968864.

7. Ferrufino-Ponce ZK, Henderson BA. Radiotherapy and cataract formation. Semin Ophthalmol. 2006; 21:171–180. PMID: 16912015.

8. Decaudin D, Dendale R, Lumbroso-Le Rouic L. Treatment of mucosa-associated lymphoid tissue-type ocular adnexal lymphoma. Anticancer Drugs. 2008; 19:673–680. PMID: 18594208.

9. Ainsbury EA, Bouffler SD, Dorr W, et al. Radiation cataractogenesis: a review of recent studies. Radiat Res. 2009; 172:1–9. PMID: 19580502.

10. Son SH, Choi BO, Kim GW, et al. Primary radiation therapy in patients with localized orbital marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue (MALT Lymphoma). Int J Radiat Oncol Biol Phys. 2010; 77:86–91. PMID: 19632068.

11. Osman IM, Abouzeid H, Balmer A, et al. Modern cataract surgery for radiation-induced cataracts in retinoblastoma. Br J Ophthalmol. 2011; 95:227–230. PMID: 20576779.

12. Bischof M, Karagiozidis M, Krempien R, et al. Radiotherapy for orbital lymphoma: outcome and late effects. Strahlenther Onkol. 2007; 183:17–22. PMID: 17225941.
13. Shore RE, Neriishi K, Nakashima E. Epidemiological studies of cataract risk at low to moderate radiation doses: (not) seeing is believing. Radiat Res. 2010; 174:889–894. PMID: 21128813.

14. Coupland SE, White VA, Rootman J, et al. A TNM-based clinical staging system of ocular adnexal lymphomas. Arch Pathol Lab Med. 2009; 133:1262–1267. PMID: 19653722.

15. Lee SE, Paik JS, Cho WK, et al. Feasibility of the TNM-based staging system of ocular adnexal extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue (MALT lymphoma). Am J Hematol. 2011; 86:262–266. PMID: 21328439.

16. Behrens R, Dietze G. Monitoring the eye lens: which dose quantity is adequate? Phys Med Biol. 2010; 55:4047–4062. PMID: 20601777.

17. Monzen Y, Hasebe H. Radiotherapy for localized orbital mucosa-associated lymphoid tissue lymphoma. Ophthalmologica. 2007; 221:233–237. PMID: 17579288.

18. Wachtlin J, Bechrakis NE, Schueler AO, et al. Phacoemulsification following treatment of choroidal melanoma. Graefes Arch Clin Exp Ophthalmol. 2000; 238:942–948. PMID: 11196355.

19. Schaumberg DA, Dana MR, Christen WG, Glynn RJ. A systematic overview of the incidence of posterior capsule opacification. Ophthalmology. 1998; 105:1213–1221. PMID: 9663224.

20. Kucuksumer Y, Bayraktar S, Sahin S, Yilmaz OF. Posterior capsule opacification 3 years after implantation of an AcrySof and a MemoryLens in fellow eyes. J Cataract Refract Surg. 2000; 26:1176–1182. PMID: 11008045.
21. Montenegro GA, Marvan P, Dexl A, et al. Posterior capsule opacification assessment and factors that influence visual quality after posterior capsulotomy. Am J Ophthalmol. 2010; 150:248–253. PMID: 20541740.

22. Kao SC, Kau HC, Tsai CC, et al. Lacrimal gland extranodal marginal zone B-cell lymphoma of MALT-type. Am J Ophthalmol. 2007; 143:311–316. PMID: 17184716.

Table 3
Characteristics of cataract and the types of IOLs used
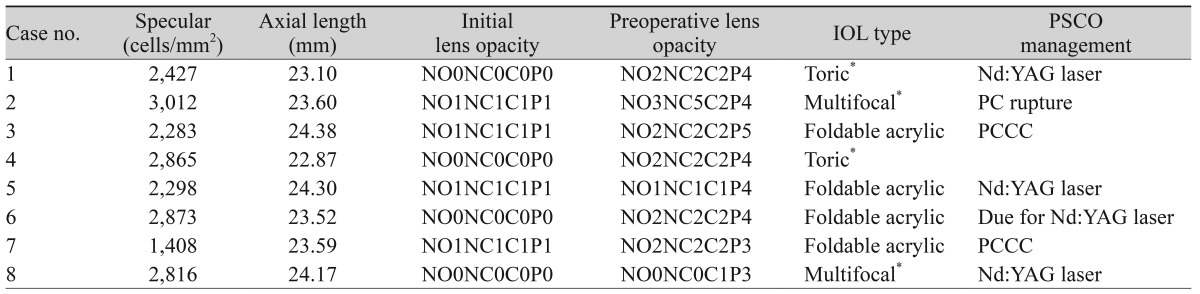
In all patients, P increased in LOCS III grade by two or more units. In case 2, a posterior capsule rupture occurred during phacoemulsification due to severe posterior subcapsular cataract, and in case 3 and 7 , PCCC was performed during the operation.
IOL = intraocular lens; NO = nuclear opalescence; NC = nuclear color; C = cortical cataract; P = posterior subcapsular cataract; PSCO = posterior subcapsular opacification; PC = posterior capsule; PCCC = posterior continuous curvilinear capsulorhexis
*Omits foldable acrylic




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download