Abstract
Purpose
To investigate correlations between preoperative and postoperative foveal microstructures in patients with macula-off rhegmatogenous retinal detachment (RRD).
Methods
We reviewed the records of 31 eyes from 31 patients with macula-off RRD who had undergone successful re-attachment surgery. We analyzed data obtained from complete ophthalmologic examinations and optical coherence tomography (OCT) before and 9 to 12 months after surgery. All postoperative OCT measurements were taken with spectral-domain OCT, but a subset of preoperative OCT measurements were taken with time-domain OCT.
Results
The mean duration of macular detachment was 15.5 ± 15.2 days, and mean preoperative best-corrected visual acuity (BCVA, logarithm of the minimum angle of resolution) was 1.03 ± 0.68. Preoperative visual acuity was correlated with retinal detachment height (p < 0.001) and the existence of intraretinal separation (IRS) along with outer layer undulation (OLU) (p = 0.022), but not with macula-off duration. The final BCVA was significantly correlated with integrity of the junction between the photoreceptor inner and outer segments (IS/OS) combined with the continuity of external limiting membrane (ELM) (p = 0.025). The presence of IRS and OLU on a detached macula were highly correlated with the final postoperative integrity of the IS/OS junction and the ELM (p = 0.017).
Conclusions
Eyes preoperatively exhibiting IRS and OLU showed a higher incidence of disruption to the photoreceptor IS/OS junction and the ELM at final follow-up. Such a close correlation between preoperative and postoperative structural changes may explain why ultimate visual recovery in such eyes is poor.
A substantial proportion of patients with macula-off rhegmatogenous retinal detachment (RRD) experience poor visual recovery even after successful re-attachment surgery. Many studies have shown associations between structural changes and final visual outcomes in macula-off retinal detachment (RD) patients who have undergone successful retinal re-attachment surgery.
Preoperative visual acuity and duration of macular detachment are known to influence post-surgery visual outcomes [1-3]. More recent studies using optical coherence tomography (OCT) showed that preoperative OCT findings, such as a greater height of the detached fovea, and the presence of an intraretinal cyst, intraretinal separation (IRS), and/or outer layer undulation (OLU), were associated with postoperative visual acuity [1,4,5].
Postoperative factors relevant to visual outcome include the presence of cystic macular edema, development of an epiretinal membrane (ERM), presence of retinal folds, subretinal retinal pigment epithelium migration, and the persistence of subretinal fluid [1,6]. With development of spectral-domain OCT (SD-OCT), the postoperative microstructure of a re-attached macula can now be studied in greater detail. Wakabayashi et al. found that the junction between the photoreceptor inner and outer segments (IS/OS) and that of the external limiting membrane (ELM) were both closely (and positively) correlated with postoperative visual acuity [7].
Although several studies have documented the relationship between preoperative and postoperative OCT findings on the one hand and pre and postoperative visual outcomes on the other, few reports have compared preoperative OCT findings with postoperative OCT data. In the present study, we used SD-OCT to evaluate preoperative and postoperative factors affecting the anatomic and functional outcomes of retinal re-attachment surgery after maculaoff RRD repair, focusing on the correlation between preoperative microstructure of the fovea and postoperative photoreceptor integrity.
This study was performed with approval from the instutional review board at Asan Medical Center and adhered to the tenets of the Declaration of Helsinki.
Data were retrospectively abstracted from the medical records of patients who underwent successful retinal re-attachment surgery after diagnosis of macula-off RRD at the Asan Medical Center, Seoul, Korea, from October 2006 to March 2009. Among 147 patients who underwent surgery to treat RRD, we selected those for whom both preoperative and postoperative OCT data (the latter collected 9 to 12 months after surgery) were available. Because some earlier patients were treated when only time-domain OCT (TD-OCT; Stratus OCT3, Carl Zeiss Meditec, Dublin, CA, USA) was available, such patients (18 patients) were examined using TD-OCT preoperatively and SD-OCT (Cirrus OCT, Carl Zeiss Meditec) postoperatively. The remaining patients were evaluated using SD-OCT both preoperatively and postoperatively. Eyes for which OCT images were poor (with a signal strength lower than 6) were excluded. In addition, 24 eyes with bullous RD were also excluded either because the fovea was hidden or the acutely detached fovea could not be included in the field of the OCT scan. Patients were considered ineligible if they had any ocular findings that might influence visual acuity such as traumatic RD, intraocular inflammation, vitreous hemorrhage, proliferative vitreoretinopathy, corneal opacity, a visually significant cataract, or pathologic myopia. Seventeen eyes with complications, including development of a postoperative ERM (3 eyes), persistence of subfoveal fluid (2 eyes), or recurrent RD (12 eyes), were also excluded. Finally, we analyzed 31 eyes of 31 macula-off RRD patients in the present study.
All patients underwent complete ophthalmologic examinations both preoperatively and at their final visits. The duration of macular detachment was based on the onset of central visual decrease. Best-corrected visual acuity (BCVA) was evaluated using the Snellen visual acuity (VA) chart, and the data were converted to the logarithm of the minimum angle of resolution (logMAR) scale. When a patient could not read text 1 m away, VA was measured by counting fingers or by hand movement and was converted to a Snellen value of 0.014 or 0.003, respectively [8].
The preoperative OCT parameters included in analysis were the RD height, which was manually measured as the vertical distance from the detached fovea to the retinal base, and the RD distance, which was measured as the shortest distance from the detached fovea to the undetached retina (Fig. 1A). Intraretinal morphologic parameters, IRS and OLU, were assessed from the central macular area (3 mm in diameter) either from TD-OCT images or from SD-OCT images (Fig. 1B and 1C).
Postoperative OCT parameters, emphasizing photoreceptor restoration, IS/OS integrity, and ELM status, were analyzed from 31 postoperative SD-OCT images taken using enhanced resolution. Patients were classified into two groups (those with an intact IS/OS and an intact ELM, and patients with a damaged IS/OS and a damaged ELM). 'Damage' was defined as disruption or loss of integrity as shown in SD-OCT imaging (Fig. 1D). All OCT findings were interpreted by two investigators, SGJ and YHY, who were blinded to clinical data.
All statistical tests were performed using SPSS ver. 15.0 (SPSS Inc., Chicago, IL, USA). Correlations between parameters were determined using Pearson's test. Comparisons of variables between groups were performed employing the independent t-test or ANOVA. Cross-table analysis was achieved using the chi-square test or Fisher's exact test, depending on the numbers of variables in the cross-table cells.
The baseline characteristics of the 31 patients are summarized in Table 1. The mean patient age was 44.1 ± 18.1 years; 25 (81%) patients were treated with pars plana vitrectomy and 6 (19%) with only scleral buckling. Twelve (39%) patients who were older than 50 years underwent cataract extraction at the time of vitrectomy. Therefore, cataract formation after reattachment surgery may not confound the analysis of our series of patients. Among the 31 eyes, 12 (39%) had superior detachment and 15 (48%) inferior detachment.
The clinical and OCT characteristics of the 31 patients are listed in Table 2. Of all patients, 18 were examined by TD-OCT preoperatively and by SD-OCT after surgery. The other patients were examined using SD-OCT both preoperatively and postoperatively. The mean duration of macular detachment was 15.5 ± 15.2 days (range, 1 to 60 days), with 30 days or less in 26 (83%) patients. Only patients for whom detached maculae were visible inside the OCT frame were included, so the average height of a detached macula was 531.19 ± 388.31 µm (range, 67 to 1,344 µm).
On preoperative OCT, IRS with OLU was seen in 12 (39%) eyes, and IRS without OLU was detected in 4 (13%). IRS with OLU was more commonly noted in eyes with superior segment detachment (p = 0.039), but this was not correlated with patient age or phakic or pseudophakic preoperative lens status. Upon postoperative photoreceptor integrity classification, 15 (48%) eyes showed an intact IS/OS and ELM, 1 (3%) had a damaged IS/OS but an intact ELM, 1 (3%) had an intact IS/OS but a damaged ELM, and 14 (45%) had damage to both the IS/OS and the ELM.
RD height was significantly associated with preoperative VA (p < 0.001), but RD distance was not (p = 0.120). Macula-off duration, defined as the time from central vision loss to operation, was not correlated with preoperative BCVA (p = 0.905). Of the tested OCT parameters, IRS with OLU was not correlated with duration of macular detachment but significantly correlated with RD height (p = 0.28 andp = 0.002, respectively) (Fig. 2A and 2B). IRS associated with OLU was correlated with preoperative visual acuity (p = 0.022) (Fig. 2C).
When we assessed the relationship between postoperative photoreceptor integrity and postoperative VA, a significant correlation was evident (p = 0.025) (Fig. 2D).
The mean preoperative and final postoperative VA values were 1.03 ± 0.68 and 0.42 ± 0.46 logMAR units, respectively. No correlation between preoperative and postoperative BCVA values was evident (p = 0.35). RD height was associated with postoperative BCVA (p = 0.019), but the RD distance was not (p = 0.25). Postoperative BCVA was not associated with macula-off duration (p = 0.17).
Macula-off duration was significantly (negatively) associated with postoperative restoration of the IS/OS and the ELM (p = 0.037). Microstructural change in the detached macula (IRS or OLU) was negatively correlated with postoperative microstructural recovery as assessed by photoreceptor integrity. When IRS and OLU were present together, recovery of photoreceptor integrity postoperatively was significantly reduced (p = 0.017) (Fig. 3).
Although the surgical anatomic success rate is relatively high in patients with macula-off RRD [9], visual outcomes are often less than satisfactory and difficult to predict [1,10-12]. When the macula becomes detached from the underlying retinal pigment epithelium, macular microstructure changes rapidly. In our previous work, we showed that, unlike the situation in patients with central serous chorioretinopathy (CSR) (in whom VA remains relatively good for several months), patients with macula-off RRD lose VA within days, even when the height of the detached macula is no greater than the elevation of the CSR [4].
Preoperative predictors are helpful to predict postoperative visual prognosis and as aids toward understanding the mechanism of postoperative VA restoration in patients with macula-off RRD. As mentioned above, several preoperative clinical variables and structural features are known to be associated with postoperative VA status. Some postoperative structural changes have also been shown to correlate with postoperative VA [13].
In the present study, we re-evaluated such correlations and showed that preoperative microstructural changes (IRS and OLU) in the detached macula appeared to be negatively correlated with postoperative recovery of the photoreceptor layer (as assessed by IS/OS integrity and ELM status) in a re-attached macula. To the best of our knowledge, such comparisons have not previously been conducted due to the technical limitations of conventional low-resolution OCT. Although preoperative OCT variables such as IRS and OLU are adequately measured using TD-OCT [13], OCT parameters such as ELM and IS/OS junction status can be accurately evaluated only via the use of SD-OCT [14].
As shown here, eyes with IRS, especially when accompanied by OLU of the detached macula, were more likely to show disruption of the IS/OS junction and damage to the ELM after macular re-attachment. A recent study has shown that damage to the IS/OS junction, with or without disruption of the ELM in postoperative SD-OCT image, may explain inadequate postoperative visual recovery [7]. Nakanishi et al. [15] showed, using their prototype SD-OCT, that a preoperative foveal loss of IS/OS at the detached macula was significantly correlated with postoperative visual acuity. This preoperative feature of IS/OS dropout shared a common characteristic with our preoperative variables (IRS and OLU) of being significantly associated with the height of the detached macula but not with the duration of the macular detachment.
The presence of IRS or OLU in the detached macula has been reported to indicate poor prognosis [1,3,5,16]. However, the pathogenic mechanisms causing such changes and the predisposing factors remain unknown. In our patient series, we found that increased height of the detached macula and superior hemisphere detachment may predispose toward development of IRS or OLU in the detached outer retinal layer. It is likely that any condition resulting in rapid and broad separation of the neural retina from the underlying retinal pigment epithelial layer can induce outer retinal layer separation accompanied by OLU.
Photoreceptor cells in a detached retina undergo apoptosis [17]. In humans, cell death was evident within 24 hours of separation, peaked at day 2, and decreased to a low level at day 7 [17]. In animals, apoptosis peaked 2 to 3 days after separation and returned to low levels 7 to 28 days after detachment [17]. In the present study, macula-off duration was significantly negatively associated with postoperative restoration of the IS/OS and the ELM. However, no such association was evident when the influence of preoperative structural changes such as IRS or OLU on restoration was evaluated. A greater risk of photoreceptor apoptosis upon longer duration of macular detachment may hinder postoperative restoration of photoreceptor integrity.
Although conventional OCT can easily demonstrate the persistence of subfoveal fluid or the presence of an ERM, resulting in poor postoperative VA, recent technical innovations introducing SD-OCT have enabled foveal microstructure to be studied in greater detail. When a re-attached macula attains normal morphology, the integrity of the photoreceptor cell layer at the fovea remains of interest. Several authors have reported significant correlations between photoreceptor integrity, as assessed by the presence of an ELM with or without an IS/OS line, and postoperative BCVA [5,7,15,16,18].
We found that disrupted photoreceptor integrity in a re-attached macula was well-correlated with the presence of IRS and OLU in the detached macula. This may explain why eyes with preoperative IRS or OLU showed poor visual recovery even after successful macular re-attachment.
It is known that postoperative VA recovers during the first 6 months after treatment and may continue to improve until 12 months following surgical re-attachment. Hence, we conducted all final assessments 9 to 12 months after surgery. A recent study by Shimoda et al. [19] found that a gradual morphological recovery of the IS/OS line continued until 6 months postoperatively, and this was well-correlated with improvements in visual recovery during the early postoperative period. Although we did not compare earlier postoperative macular morphology with later morphology (thus, we did not perform serial SD-OCT evaluation), we are currently collecting further data on serial improvement in postoperative OCT parameters.
Unlike what was seen in several previous studies [1,6,20-23], neither preoperative VA nor duration of macular detachment was correlated with postoperative BCVA in our patient series. The reasons for this observation remain unknown, but one explanation is that our study patients did not include those who had significantly poor preoperative VA and were expected to show poor postoperative VA. In other words, our study population seemed to be rather skewed toward those with relatively good visual potential. Most of our patients experienced macular detachment of relatively short duration. Thus, 48% (15 / 31) of our patients were treated within 8 days and 68% (21 / 31) within 21 days [1]. In addition, many exclusion criteria, such as an RD height greater than the OCT image frame, may explain the lack of correlation between preoperative BCVA and final postoperative BCVA. It was notable that RD height was associated not only with preoperative, but also postoperative BCVA. This observation is consistent with those of previous reports. The greater the distance between the foveal cones and the pigment epithelial layer, the less likely it is that the cones will receive adequate oxygenation and nutrition from the choriocapillaries and epithelial layer via diffusion across the subretinal space [1,24]. Ross and Stockl [3] also emphasized that, even in patients in whom the duration of detachment is longer, postoperative BCVA may nonetheless be better in patients with a low compared to elevated RD height.
Our study had some limitations, including a retrospective design, a small sample size, and the possible co-existence of uncontrolled variables. In some patients treated early in the study, preoperative OCT did not employ SD-OCT. However, unlike when relevant postoperative parameters (IS/OS junction, ELM) are evaluated, preoperative parameters (IRS or OLU) are easily determined using Stratus OCT (Fig. 1B). We thus consider our assessments to be accurate. A larger sample size and use of identical OCT equipment in all patients will render our future data more reliable. The postoperative OCT collection timing was not the same in all patients, ranging from 9 to 12 months after surgery. However, we consider this limitation to be acceptable, because the postoperative functional recovery was reported to reach to the near-plateau level after 9 months following macular reattachment [25].
In conclusion, preoperative macular analysis using OCT may assist in the prediction of both postoperative foveal microstructure and final visual outcomes in patients with macula-off RRD. IRS with OLU in a detached macula is a poor prognostic factor for visual recovery, regardless of the duration of macular detachment.
Figures and Tables
Fig. 1
(A) time-domain optical coherence tomographic (TD-OCT) image of macula-off rhegmatogenous retinal detachment reveals retinal detachment (RD); the height of such detachment and the extent of RD. (B) A TD-OCT image of macular-off rhegmatogenous retinal detachment shows intraretinal separation (IRS) and outer layer undulation (OLU). (C) An image acquired using spectral-domain optical coherence tomography (SD-OCT). IRS and OLU are relatively large structural changes. Thus, TD-OCT can identify such changes as reliably as can SD-OCT. (D) An SD-OCT image shows disruption of the junction between the photoreceptor inner and outer segments (IS/OS) and an external limiting membrane (ELM); the image was acquired on postoperative follow-up. All parameters were assessed from the central 3-mm diameter area.

Fig. 2
(A) No significant difference in macula-off duration was evident between eyes with both intraretinal separation (IRS) and outer layer undulation (OLU) (p = 0.28). (B) Eyes with both IRS and OLU had a greater height of retinal detachment (RD) than did eyes lacking both IRS and OLU (p = 0.002). (C) Eyes with both IRS and OLU had lower best-corrected visual acuity (BCVA) values than eyes without either feature (p = 0.022). (D) Eyes with an intact junction between the photoreceptor inner and outer segments (IS/OS) and an intact external limiting membrane (ELM) showed better postoperative BCVA values than did eyes in which the IS/OS junction and the ELM were both damaged (p = 0.025). The solid lines indicate the medians and the long dashes the averages. logMAR = logarithm of the minimum angle of resolution.

Fig. 3
Eyes with both intraretinal separation (IRS) and outer layer undulation (OLU) exhibited lower integrity of both junction between the photoreceptor inner and outer segments and the external limiting membrane (p = 0.017). PHRc = photoreceptor complex including external limiting membrane and junction between the photoreceptor inner and outer segments.
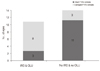
Table 2
Clinical and optical coherence tomographic characteristics of patients
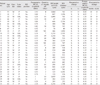
RD = retinal detachment; BCVA = best-corrected visual acuity; logMAR = logarithm of the minimum angle of resolution; S = intraretinal (outer nuclear layer) separation; U = undulation; IS/OS = junction between the photoreceptor inner and outer segments; ELM = external limiting membrane; M = male; F = female; P = phakic; Su = superior; NE = not evaluable; O = exists; D = disrupted; X = does not exist; I = intact; IOL = intraocular lens (pseudophakia); In = inferior.
Acknowledgements
This study was supported by a grant of the Korea Healthcare Technology R&D Project, Ministry of Health, Welfare & Family Affairs, Republic of Korea (no. A080557).
References
1. Lecleire-Collet A, Muraine M, Menard JF, Brasseur G. Predictive visual outcome after macula-off retinal detachment surgery using optical coherence tomography. Retina. 2005. 25:44–53.
2. Hassan TS, Sarrafizadeh R, Ruby AJ, et al. The effect of duration of macular detachment on results after the scleral buckle repair of primary, macula-off retinal detachments. Ophthalmology. 2002. 109:146–152.
3. Ross WH, Stockl FA. Visual recovery after retinal detachment. Curr Opin Ophthalmol. 2000. 11:191–194.
4. Lee SY, Joe SG, Kim JG, et al. Optical coherence tomography evaluation of detached macula from rhegmatogenous retinal detachment and central serous chorioretinopathy. Am J Ophthalmol. 2008. 145:1071–1076.
5. Lecleire-Collet A, Muraine M, Menard JF, Brasseur G. Evaluation of macular changes before and after successful retinal detachment surgery using stratus-optical coherence tomography. Am J Ophthalmol. 2006. 142:176–179.
6. Abouzeid H, Wolfensberger TJ. Macular recovery after retinal detachment. Acta Ophthalmol Scand. 2006. 84:597–605.
7. Wakabayashi T, Oshima Y, Fujimoto H, et al. Foveal microstructure and visual acuity after retinal detachment repair: imaging analysis by Fourier-domain optical coherence tomography. Ophthalmology. 2009. 116:519–528.
8. Schulze-Bonsel K, Feltgen N, Burau H, et al. Visual acuities "hand motion" and "counting fingers" can be quantified with the freiburg visual acuity test. Invest Ophthalmol Vis Sci. 2006. 47:1236–1240.
9. Minihan M, Tanner V, Williamson TH. Primary rhegmatogenous retinal detachment: 20 years of change. Br J Ophthalmol. 2001. 85:546–548.
10. McPherson AR, O'Malley RE, Butner RW, Beltangady SS. Visual acuity after surgery for retinal detachment with macular involvement. Ann Ophthalmol. 1982. 14:639–645.
11. Yazici B, Gelisken O, Avci R, Yucel A. Prediction of visual outcome after retinal detachment surgery using the Lotmar visometer. Br J Ophthalmol. 2002. 86:278–281.
12. Friberg TR, Eller AW. Prediction of visual recovery after scleral buckling of macula-off retinal detachments. Am J Ophthalmol. 1992. 114:715–722.
13. Hagimura N, Suto K, Iida T, Kishi S. Optical coherence tomography of the neurosensory retina in rhegmatogenous retinal detachment. Am J Ophthalmol. 2000. 129:186–190.
14. Kiernan DF, Mieler WF, Hariprasad SM. Spectral-domain optical coherence tomography: a comparison of modern high-resolution retinal imaging systems. Am J Ophthalmol. 2010. 149:18–31.
15. Nakanishi H, Hangai M, Unoki N, et al. Spectral-domain optical coherence tomography imaging of the detached macula in rhegmatogenous retinal detachment. Retina. 2009. 29:232–242.
16. Smith AJ, Telander DG, Zawadzki RJ, et al. High-resolution Fourier-domain optical coherence tomography and microperimetric findings after macula-off retinal detachment repair. Ophthalmology. 2008. 115:1923–1929.
17. Arroyo JG, Yang L, Bula D, Chen DF. Photoreceptor apoptosis in human retinal detachment. Am J Ophthalmol. 2005. 139:605–610.
18. Schocket LS, Witkin AJ, Fujimoto JG, et al. Ultrahigh-resolution optical coherence tomography in patients with decreased visual acuity after retinal detachment repair. Ophthalmology. 2006. 113:666–672.
19. Shimoda Y, Sano M, Hashimoto H, et al. Restoration of photoreceptor outer segment after vitrectomy for retinal detachment. Am J Ophthalmol. 2010. 149:284–290.
20. Doyle E, Herbert EN, Bunce C, et al. How effective is macula-off retinal detachment surgery. Might good outcome be predicted? Eye (Lond). 2007. 21:534–540.
21. Laatikainen L, Harju H, Tolppanen EM. Post-operative outcome in rhegmatogenous retinal detachment. Acta Ophthalmol (Copenh). 1985. 63:647–655.
22. Salicone A, Smiddy WE, Venkatraman A, Feuer W. Visual recovery after scleral buckling procedure for retinal detachment. Ophthalmology. 2006. 113:1734–1742.
23. Tani P, Robertson DM, Langworthy A. Prognosis for central vision and anatomic reattachment in rhegmatogenous retinal detachment with macula detached. Am J Ophthalmol. 1981. 92:611–620.
24. Machemer R. Experimental retinal detachment in the owl monkey. II. Histology of retina and pigment epithelium. Am J Ophthalmol. 1968. 66:396–410.
25. Rossetti A, Doro D, Manfre A, Midena E. Long-term follow-up with optical coherence tomography and microperimetry in eyes with metamorphopsia after macula-off retinal detachment repair. Eye (Lond). 2010. 24:1808–1813.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download