Abstract
Herein, we report a case of nasal natural killer T-cell lymphoma (NKTL) with intraocular involvement. A 57-year-old woman was referred due to a three-day history of photophobia and diplopia in the left eye. One-month previously, she was diagnosed with nasal NKTL of the right nasal cavity. Ophthalmic examination revealed conjunctival injection and ptosis. The left pupil was fully dilated and non-reactive to light. Ocular motion was restricted on left-upper gaze. Five days later, anterior uveitis developed and persisted despite topical steroid treatment. An orbital magnetic resonance imaging was without specific findings, however, ophthalmoplegia, vitreous opacity, and an iris mass were observed. A diagnostic anterior chamber aspiration was performed. Aqueous humor aspiration revealed 35% morphologically atypical lymphocytes. After an intravitreal triamcinolone injection, radiotherapy and chemotherapy were administered; this resolved the uveitis and iris mass. When refractory uveitis or orbital pseudotumor occurs in patients with nasal NKTL, ocular and orbital involvement of the NKTL should be considered.
Malignant lymphomas that develop in the orbit and ocular adnexa account for 8% of all extranodal lymphomas [1,2]. Most ocular and orbital lymphomas are non-Hodgkin's B-cell lymphoma [1]. At these sites, with the exception of B-cell lymphoma, lymphoblastic diseases are rare and occur in only 1% to 3% of cases [2]. Ocular and ocular adnexa T-cell lymphomas are rare. There are few cases of nasal natural killer T-cell lymphoma (NKTL) reported in the medical literature [1-4]. Additionally, pathologically confirmed intraocular involvement of nasal NKTL, such as the case reported here, is very rare [3].
A 57-year-old woman presented with a three-day history of photophobia and diplopia in the left eye. She was diagnosed with histologically confirmed nasal NKTL of the right nasal cavity one month prior. The Snellen visual acuity of the affected eye with correction was 1.0 / 0.63, and the intraocular pressure in the right and left eyes was 17 and 18 mmHg, respectively. The patient had mild left eye conjunctival injection, ptosis, and swelling of the eyelid. The left pupil was fully dilated with no pupillary light reflex. Ocular movement on left-upper gaze was limited in the left eye. Five days later, the left corrected visual acuity deteriorated and ptosis worsened. Slit lamp examination revealed anterior uveitis refractory to topical steroid treatment. Opthalmoplegia, vitreous opacity, and an iris mass developed in the left eye (Fig. 1A and 1B). Orbital magnetic resonance imaging and cerebrospinal fluid investigations were unremarkable. Aqueous humor aspiration from the anterior chamber was performed with a 26-gauge needle. Thirty-five percent of the cells obtained from the aspiration were morphologically atypical lymphocytes.
The patient was diagnosed with intraocular dissemination of the lymphoma. Treatment with intravitreal triamcinolone injections, radiotherapy, and chemotherapy was administered. Skin manifestations of the lymphoma were noted 40 days post-chemotherapy (Fig. 2A). Skin biopsy confirmed neoplastic infiltration of small- to medium-sized pleomorphic lymphocytes with irregular nuclei, inconspicuous nucleoli, and scant cytoplasm (Fig. 2B). Immunohistochemical staining was positive for CD56 (Fig. 2C) and CD3 (Fig. 2D). The patient was diagnosed with nasal NKTL with ocular involvement. After receiving radiotherapy at 900 cGy, her visual acuity improved and her anterior uveitis, vitreous opacity, and iris mass resolved (Fig. 3A and 3B). However, the patient's condition continued to deteriorate despite radiotherapy and chemotherapy, and her ptosis and ophthalmoplegia gradually progressed. She died of sepsis three months after diagnosis.
Extranodal NKTL, including nasal NKTL, previously known as lethal midline granuloma, is a definitive diagnostic entity according to the World Health Organization lymphoma classification [1,4,5]. The nasal cavity is the most common site of involvement. However, histopathologically identical tumors may be identified at other extranodal sites, including the skin, muscle, gastrointestinal tract, liver, kidney, and retroperitoneal space [6,7]. Orbital and adnexal involvement has been infrequently reported in patients with this disorder [6]. There are few reported cases of nasal NKTL involving the orbit and/or ocular adnexa [2,6]. Coupland et al. [2] and Woog et al. [6] reported the formation of chronic uveitis and vitritis as intraocular manifestations of NKTL. Cimino et al. [3] did report a case of histologically confirmed nasal NKTL with intraocular involvement, however, in most cases intraocular involvement has not been confirmed histologically. The presence of intraocular involvement raises the possibility of leptomeningeal or central nervous system dissemination, and prompts consideration for external-beam radiotherapy to the eye and orbit in addition to systemic chemotherapy [1,6,8]. NKTL involving the ocular adnexa is generally a rapidly progressing disease, with a short survival from time of diagnosis, despite standard therapy [6,9,10]. This was true in the current case as well; the patient died three months after diagnosis. Since NKTL with ocular and orbital involvement is very rare and is characterized by rapid disease progression and a poor prognosis, NKTL should be considered in the differential diagnosis of uveitis or orbital pseudotumor refractory to therapy.
Figures and Tables
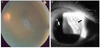 | Fig. 1(A) Fundoscopy revealed vitreous haziness and opacity. (B) Slit lamp exam revealed a nodular, depigmented, mass-like appearance of the iris (black arrow) and a pinkish lump in the iris (white arrow). |
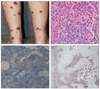 | Fig. 2(A) This photograph demonstrates multiple erythematous and violaceous, well-defined, coin-sized plaques and nodules in the lower limbs. (B) The neoplastic infiltrate was composed of small- to medium-sized pleomorphic lymphocytes with irregular nuclei, inconspicuous nucleoli, and scant cytoplasm. (C) Immunotype was CD56+. (D) Immunotype was CD3+. |
References
1. Choi KH, Lee SJ, Suh YL, Kim YD. Nasal-type natural killer/T-cell lymphoma of the orbit. J Korean Ophthalmol Soc. 2004. 45:2145–2150.
2. Coupland SE, Krause L, Delecluse HJ, et al. Lymphoproliferative lesions of the ocular adnexa. Analysis of 112 cases. Ophthalmology. 1998. 105:1430–1441.
3. Cimino L, Chan CC, Shen D, et al. Ocular involvement in nasal natural killer T-cell lymphoma. Int Ophthalmol. 2009. 29:275–279.
4. Hon C, Kwok AK, Shek TW, et al. Vision-threatening complications of nasal T/NK lymphoma. Am J Ophthalmol. 2002. 134:406–410.
5. Al-Hakeem DA, Fedele S, Carlos R, Porter S. Extranodal NK/T-cell lymphoma, nasal type. Oral Oncol. 2007. 43:4–14.
6. Woog JJ, Kim YD, Yeatts RP, et al. Natural killer/T-cell lymphoma with ocular and adnexal involvement. Ophthalmology. 2006. 113:140–147.
7. Nakamura S, Suchi T, Koshikawa T, et al. Clinicopathologic study of CD56 (NCAM)-positive angiocentric lymphoma occurring in sites other than the upper and lower respiratory tract. Am J Surg Pathol. 1995. 19:284–296.
8. Cheung MM, Chan JK, Lau WH, et al. Primary non-Hodgkin's lymphoma of the nose and nasopharynx: clinical features, tumor immunophenotype, and treatment outcome in 113 patients. J Clin Oncol. 1998. 16:70–77.
9. Chan JK, Sin VC, Wong KF, et al. Nonnasal lymphoma expressing the natural killer cell marker CD56: a clinicopathologic study of 49 cases of an uncommon aggressive neoplasm. Blood. 1997. 89:4501–4513.
10. Chan JK. Natural killer cell neoplasms. Anat Pathol. 1998. 3:77–145.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download