Abstract
Tubulointerstitial nephritis and uveitis (TINU) syndrome is a rare disease entity usually occurring in children. In the present study a case of TINU syndrome in an elderly patient is described and relevant literature is reviewed. A 61-year-old man presented with bilateral flank pain, urinary frequency, and foamy urine. A kidney ultrasonography revealed an increase in kidney parenchyma echogenicity. Following a kidney biopsy, the patient was diagnosed with acute tubulointerstitial nephritis. An ophthalmology examination initially performed for floater symptoms, revealed anterior uveitis in both eyes. Acute tubulointerstitial nephritis and anterior uveitis in both eyes responded to treatment with oral prednisolone, furosemide, carvedilol, and a topical steroid. TINU syndrome can occur in the elderly and should be part of the differential diagnosis when seeing a patient who has uveitis in association with renal disease; any therapy should be managed by both an internist and an ophthalmologist.
Tubulointerstitial nephritis and uveitis (TINU) syndrome was first described by Dobrin et al. in 1975 [1], and nearly 200 cases have been reported to date [2,3]. Approximately, 1% to 2% of patients who visit uveitis clinics present with TINU [4,5]. Although separately they are common diseases, co-occurrence is uncommon and is mainly seen in children [6,7]. Therefore, physicians, especially pediatricians, nephrologists, rheumatologists, and ophthalmologists, who are likely to see such patients should be familiar with TINU syndrome in order to recognize and properly diagnose the condition [6].
Available case reports describing TINU generally involve children and young adults [7-12]. However, the authors of the present study encountered an elderly patient with TINU; the following is a description of this case and a review of the relevant literature. To our knowledge, this is the first case report of TINU in Korea specifically occurring in the elderly.
A 61-year-old man came to the hospital complaining of bilateral flank pain. Left flank pain began approximately a month earlier, followed by right flank pain 4 days later. The patient also complained of dyspnea on exertion, urinary frequency, and foamy urine. He was diagnosed with hypertension 15 years prior and had taken traditional Korean herbal medicines, such as acanthopanax, phellinus, licorice root, and steamed red ginseng. One week before coming to our hospital, he visited a local ophthalmologic clinic for bilateral floater symptoms and was diagnosed with anterior uveitis and treated with systemic and topical steroids.
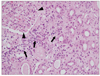
Laboratory tests conducted at the hospital showed a blood urea nitrogen of 26 mg/dL (the upper limit of normal), a serum creatinine of 2.3 mg/dL, and an estimated glomerular filtration rate (GFR) of 30.9 mL/min (normal, 80 to 120 mL/min). An ultrasonography of the kidney showed elevated echogenicity of the parenchyma. A kidney biopsy specimen revealed diffuse interstitial infiltration of lymphocytes and eosinophils and mild tubular atrophy with focal fibrosis of the interstitium (Fig. 1). No electron-dense deposits were seen on electron microscopy (Fig. 2). No antibody deposits or immune complexes were apparent on immunofluorescent studies. A diagnosis of acute tubulointerstitial nephritis was made. Systemic administration of prednisolone 1 mg/kg/day was started and slowly tapered; furosemide and carvedilol were added for blood pressure control.
An ophthalmologic examination was conducted for evaluation of uveitis. The patient's visual acuity was 20 / 20 in the right eye and 20 / 25 in the left eye. A slit lamp examination showed a mild degree (1+ to 2+) of inflammatory cells in the anterior chamber of both eyes; however, synechia of the iris was not observed. Results of a funduscopic examination were normal, and vitreous opacity was not observed. Based on these findings, a diagnosis of TINU syndrome was made, and the patient was treated with a topical steroid (Pred Forte; Allergan, Irvine, CA, USA) for anterior uveitis. Subsequently, the anterior uveitis was well-controlled.
TINU syndrome is reportedly three times more common in women than in men, with a median age at onset of 15 years (range, 9 to 74 years) [7]. Although diagnosis of TINU syndrome is uncommon after 61 years of age, we experienced a patient with such a case [13]. Generally, renal involvement in TINU is mild [7]; however, in our patient the GRF decreased to well below the normal range. Failure to detect the disease earlier may have been the possible cause of the renal impairment.
Several medications, such as antibiotics and non-steroidal anti-inflammatory drugs, have been reported as a cause of TINU syndrome [7,14]. Using traditional Korean medicines for 9 years may have contributed to the development of the disease in the present case.
TINU is an uncommon disease and is primarily a diagnosis by exclusion; symptoms are associated with both uveitis and interstitial nephritis. General symptoms with TINU include fever (53%), weight loss (47%), general weakness and malaise (44%), and anorexia (28%) [3,7]. Ocular effects seen with uveitis are limited to the anterior chamber in approximately 80% of cases; both eyes are affected in 77% of cases. Posterior uveitis can sometimes be seen [7,15]. In most cases (65%), nephritis precedes uveitis; however, in 21% of cases, uveitis is present before nephritis, and in 15% the two conditions occur simultaneously [7].
Symptoms associated with nephritis are typical of acute interstitial nephritis, such as flank pain, pyuria (mainly sterile), hematuria, and proteinuria (which is less severe than seen with nephrotic syndrome). Renal failure could also occur and may be acute and/or chronic [16].
The etiology of TINU is unknown. An association with human leukocyte antigens has been mentioned in some reports, as well as sensitization of common antigens located both in the eye and the kidney as possible pathologic processes of TINU [7]. Several case reports have been published attributing the disease to medication use [7,17]. In addition to hypersensitivity reactions, the causative drug may act as a hapten, inducing cytokine production or vasculitis. Another possible etiology is cross reactivity of active transporters that are inhibited by carbonic anhydrase inhibitors in both the renal tubule and ciliary epithelium [7].
Laboratory examination in the evaluation of TINU syndrome is not typical. Eosinophilia, elevated C-reactive protein, elevated erythrocyte sedimentation rate, normocytic normochromic anemia, and abnormal liver function tests are among the possible findings [11]. In addition, anti-neutrophil cytoplasmic antibody, anti-nuclear antibody, and rheumatoid factor may be positive, and complement levels may be decreased. In the present case, all laboratory findings were within the normal range except for kidney function. In the absence of proteinuria and pyuria, detection of beta-2 microglobulin in the urine could lead to an early detection of acute interstitial nephritis [15]. The degree of proximal or distal tubular dysfunction may not be directly proportional to the decrease in GFR [2].
Tubulointerstitial edema and infiltration can be observed in kidney biopsy under a light microscopy [7,18], while the glomerulus and blood vessels are relatively normal; this is consistent with the present case. Infiltration with lymphocytes, plasma cells, and histiocytes may be observed, and in 34% of cases, eosinophils. Immunofluorescent findings are negative for antibody or complement in 86% of cases; similarly, no antibodies or complements were detected in our patient [7].
The differential diagnosis of TINU includes sarcoidosis, Sjogren's syndrome, Behcet's disease, Wegener's granulomatosis, systemic lupus erythematosis, hyperthyroidism, primary hyperparathyroidism, and infectious diseases (e.g., tuberculosis, brucellosis, toxoplasmosis, and herpes) [7]. Various clinical findings and laboratory results could be helpful in making the diagnosis. TINU is often not recognized and affected patients often fail to seek medical care, making the prevalence of the disease appear less than in actuality [6].
There are no prospective, randomized clinical trials regarding the treatment of TINU available. Topical steroids are commonly recommended as the treatment of choice of anterior uveitis. During the initial attack, topical steroids are usually sufficient to control the inflammation. Based on published case reports, ocular symptoms resolved in 3 months in 44% of cases while symptoms persisted for more than 3 months in 14% of cases; uveitis recurred in 41% of cases [6]. If the inflammation is not controlled with steroids or if steroid use is contraindicated or not tolerated, immunosuppressive agents such as azathioprine or methotrexate may be considered [6,19].
A diagnosis of TINU should be considered in patients with idiopathic uveitis presenting with renal disease even in elderly patients. As TINU is diagnosed by exclusion, a kidney biopsy and a thorough ophthalmologic examination are needed. Once the diagnosis of TINU is made, immediate steroid therapy is necessary together with a collaborative approach to treatment by an internist and an ophthalmologist.
Figures and Tables
References
1. Dobrin RS, Vernier RL, Fish AL. Acute eosinophilic interstitial nephritis and renal failure with bone marrow-lymph node granulomas and anterior uveitis: a new syndrome. Am J Med. 1975. 59:325–333.
2. Mackensen F, Smith JR, Rosenbaum JT. Enhanced recognition, treatment, and prognosis of tubulointerstitial nephritis and uveitis syndrome. Ophthalmology. 2007. 114:995–999.
3. Thomassen VH, Ring T, Thaarup J, Baggesen K. Tubulointerstitial nephritis and uveitis (TINU) syndrome: a case report and review of the literature. Acta Ophthalmol. 2009. 87:676–679.
4. Rosenbaum JT. Bilateral anterior uveitis and interstitial nephritis. Am J Ophthalmol. 1988. 105:534–537.
5. Levinson RD. Tubulointerstitial nephritis and uveitis syndrome. Int Ophthalmol Clin. 2008. 48:51–59.
6. Liakopoulos V, Ioannidis I, Zengos N, et al. Tubulointerstitial nephritis and uveitis (TINU) syndrome in a 52-year-old female: a case report and review of the literature. Ren Fail. 2006. 28:355–359.
7. Mandeville JT, Levinson RD, Holland GN. The tubulointerstitial nephritis and uveitis syndrome. Surv Ophthalmol. 2001. 46:195–208.
8. Vanhaesebrouck P, Carton D, De Bel C, et al. Acute tubulo-interstitial nephritis and uveitis syndrome (TINU syndrome). Nephron. 1985. 40:418–422.
9. Hirano K, Tomino Y, Mikami H, et al. A case of acute tubulointerstitial nephritis and uveitis syndrome with a dramatic response to corticosteroid therapy. Am J Nephrol. 1989. 9:499–503.
10. Radig H, Bialasiewicz AA, Gerding H, Helmchen U. Tubulointerstitial nephritis and uveitis (TINU syndrome). Ophthalmologe. 1992. 89:441–443.
11. Vohra S, Eddy A, Levin AV, et al. Tubulointerstitial nephritis and uveitis in children and adolescents: four new cases and a review of the literature. Pediatr Nephrol. 1999. 13:426–432.
12. Guerriero S, Vischi A, Giancipoli G, et al. Tubulointerstitial nephritis and uveitis syndrome. J Pediatr Ophthalmol Strabismus. 2006. 43:241–243.
13. Welzl-Hinterkorner E, Tholen A. Bilateral cystoid macular edema in an older female patient with tubulointerstitial nephritis and uveitis (TINU syndrome). Klin Monbl Augenheilkd. 2000. 216:116–117.
14. Fried T. Acute interstitial nephritis. Why do the kidneys suddenly fail? Postgrad Med. 1993. 93:105–106. 111–112. 117–120.
15. Goda C, Kotake S, Ichiishi A, et al. Clinical features in tubulointerstitial nephritis and uveitis (TINU) syndrome. Am J Ophthalmol. 2005. 140:637–641.
16. Kadanoff R, Lipps B, Khanna A, Hou S. Tubulointerstitial nephritis with uveitis (TINU): a syndrome rheumatologists should recognize: a case report and review of the literature. J Clin Rheumatol. 2004. 10:25–27.
17. Suzuki H, Yoshioka K, Miyano M, et al. Tubulointerstitial nephritis and uveitis (TINU) syndrome caused by the Chinese herb "Goreisan". Clin Exp Nephrol. 2009. 13:73–76.
18. Yanagihara T, Kitamura H, Aki K, et al. Serial renal biopsies in three girls with tubulointerstitial nephritis and uveitis syndrome. Pediatr Nephrol. 2009. 24:1159–1164.
19. Gion N, Stavrou P, Foster CS. Immunomodulatory therapy for chronic tubulointerstitial nephritis-associated uveitis. Am J Ophthalmol. 2000. 129:764–768.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download