Abstract
A 12-year-old male presented with a chief complaint of a 1-month-history of decreased visual acuity in his right eye. The patient had no past history of steroid use or other systemic diseases. On fundus examination, which included fluorescent angiography (FAG) and optical coherence tomography (OCT), the patient was diagnosed with idiopathic central chorioretinopathy, whose clinical course was monitored without any specific treatments. At the time of admission, the best-corrected visual acuity was 0.5 in the right eye and 1.0 in the left eye. On fundoscopy, a serous detachment of 1 disc diameter in size was observed in the posterior pole. According to the FAG and the OCT, serous neurosensory detachment was present. After two months of monitoring the clinical course, the best corrected visual acuity in the right eye was 0.8, and there was improvement of neurosensory retinal detachment. However, OCT detected recurrence after five months, and the corrected visual acuity was decreased to 0.6. Bevacizumab was then injected into the vitreous cavity. Complete resolution of the subretinal fluid resulted eight months later, and the corrected visual acuity improved to 1.0.
Central chorioretinopathy (CSC) is a disease that can present with either serous retinal pigment epithelial detachment or neurosensory retinal detachment in the macular region due to the accumulation of serous fluid in the posterior pole. It commonly occurs in patients between 20 and 50 years of age [1,2]. Given this background, we experienced a rare case of idiopathic CSC in a 12-year-old male that had no past history of systemic or ophthalmologic disease. Here, we report our case along with a review of the current literature.
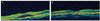
A 12-year-old male presented with the chief complaint of a 1-month-history of decreased visual acuity in his right eye. At the time of admission, the best corrected visual acuity was 0.5 in the right eye and 1.0 in the left eye. Based on fundoscopy, the serous detachment had a well-defined margin of 1 disc diameter and was observed in the posterior pole (Fig. 1A). Fluorescein angiography (FAG) identified the point-like hyperfluorescent findings of the early stage (Fig. 1B). The fluorescent substance was found to slightly spread from the leakage point with time (Fig. 1C). There was serous neurosensory detachment on optical coherence tomography (OCT; Stratus OCT, Carl Zeiss Meditec, Dublin, CA, USA) (Fig. 2A). Upon slit lamp examination, there was no evidence of inflammation in the anterior or posterior chamber. There was a lack of systemic causative factors for this patient. There were also no notable finding upon hematologic assessment performed in the Department of Endocrine Pediatrics. The patient was diagnosed with idiopathic CSC, whose clinical course was monitored without any specific treatments. Two months following a monitoring regimen, fundoscopy and OCT were performed. These tests showed that the serous retinal detachment was almost absorbed (Fig. 2B). The best corrected visual acuity in the right eye was 0.8. However, recurrence was detected by OCT five months after a monitoring regimen, and the corrected visual acuity was decreased to 0.6. There was no improvement of the symptoms over the course of a two month period. Bevacizumab (1.25 mg in 0.05 mL; Avastin, Genentech Inc., San Francisco, CA, USA) was then injected into the vitreous cavity, which gradually improved the visual acuity. A complete resolution of the subretinal fluid was shown eight months later, and the corrected visual acuity had improved to 1.0.
CSC is a disease that can show serous retinal pigment epithelial detachment or neurosensory retinal detachment in the macular region due to the accumulation of serous fluid in the posterior pole [1]. Risk factors for developing CSC include male sex, mental stress, type A personality, the use of steroids, and pregnancy [1-5]. Although rare, Cushing's syndrome or steroid-producing tumors can also occur [5,6]. The age of CSC onset has been reported to be between 20 and 50 years of age [1,2]. Fine and Owens [7] reported a case of central serous retinopathy occurring in a 7-year-old girl in 1980, which was not primary but secondary to focal chorioditis. There were no cases in which the typical symptoms of CSC had manifested without other causes. In the current case, the patient was of healthy status and had no past history of any specific disease. The patient made no complaints regarding any specific systemic diseases when he was referred to the Department of Pediatrics. The patient also had no past history of steroid use or use of psychiatric medicinal products. Furthermore, the patient had no underlying stress-related events and was not attributed a type A personality. According to FAG and OCT, the patient did not exhibit any secondary signs of other retinal and choroidal diseases.
Acute CSC has a relatively good prognosis in regard to visual acuity, and it has also been known to result in the spontaneous loss of retinal detachment and improvement of visual acuity without any specific treatment. It has recently been considered as a chronic disease that can produce decreased visual acuity [1]. Active treatments have been attempted, and the effectiveness of laser therapy and photodynamic therapy (PDT) have been demonstrated. Ongoing studies of bevacizumab use are being conducted with case reports [8,9]. Controversial opinions still exist regarding the etiology of central serous chorioretinopathy. In recent years, choroidal hyperpermeability has been assumed to be the cause of CSC based upon indocyanine green angiography and has been considered a basis of PDT treatment. Vascular endothelial growth factor (VEGF) is one of the major cytokines that induce vascular hyperpermeability. An intra-ocular injection of anti-VEGF bevacizumab may improve the symptoms of CSC by blocking the activity of VEGF. The effectiveness of this treatment method has been described [8,9]. To date, however, no studies have demonstrated the correlation between hyperpermeability of the choroidal vessel and VEGF.
Also, in the current study, due to the lack of improvement of symptoms following the recurrence, bevacizumab was injected into the vitreous cavity. Eight months following this procedure, a complete resolution of the subretinal fluid was shown. It remains unclear, however, whether the improvement of visual acuity and the resolution of the subretinal fluid originated from the treatment effect of the bevacizumab or as a result of spontaneous recovery.
Figures and Tables
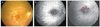 | Fig. 1(A) A fundus photograph of the right eye shows a 1-disc-diameter, well circumscribed collection of subretinal fluid at the posterior pole (arrow). (B) The filling phase of fluorescein angiography (FAG) shows pinpoint dye leakage (arrow). (C) The late phase of the FAG shows spread of the dye and filling of the detached area (arrow head). |
References
1. Wang M, Munch IC, Hasler PW, et al. Central serous chorioretinopathy. Acta Ophthalmol. 2008. 86:126–145.
2. Levine R, Brucker AJ, Robinson F. Long-term follow-up of idiopathic central serous chorioretinopathy by fluorescein angiography. Ophthalmology. 1989. 96:854–859.
3. Yannuzzi LA. Type-A behavior and central serous chorioretinopathy. Retina. 1987. 7:111–131.
4. Gelber GS, Schatz H. Loss of vision due to central serous chorioretinopathy following psychological stress. Am J Psychiatry. 1987. 144:46–50.
5. Garg SP, Dada T, Talwar D, Biswas NR. Endogenous cortisol profile in patients with central serous chorioretinopathy. Br J Ophthalmol. 1997. 81:962–964.
6. Bouzas EA, Scott MH, Mastorakos G, et al. Central serous chorioretinopathy in endogenous hypercortisolism. Arch Ophthalmol. 1993. 111:1229–1233.
7. Fine SL, Owens SL. Central serous retinopathy in a 7-year-old girl. Am J Ophthalmol. 1980. 90:871–873.
8. Torres-Soriano ME, Garcia-Aguirre G, Kon-Jara V, et al. A pilot study of intravitreal bevacizumab for the treatment of central serous chorioretinopathy (case reports). Graefes Arch Clin Exp Ophthalmol. 2008. 246:1235–1239.
9. Lim SJ, Roh MI, Kwon OW. Intravitreal bevacizumab injection for central serous chorioretinopathy. Retina. 2010. 30:100–106.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download