This article has been
cited by other articles in ScienceCentral.
Abstract
Purpose
To report the long term results of bifocal treatment in nonrefractive accommodative esotropia and to analyze the changes of accommodative convergence to accommodation (AC/A) ratio.
Methods
Sixteen patients treated with bifocal glasses for at least 5 years were evaluated retrospectively. Angle of deviation at near and distance, refractive error, and AC/A ratio by the lens gradient method were analyzed. The changes of AC/A ratios were also compared after dividing the patients according to continuation or cessation of bifocal therapy.
Results
Six patients (38%; bifocal stop group, BSG) were able to stop using bifocal glasses at an average age of 10.8 years (range, 6.5 to 15.4 years) during their follow-up. However, the other ten patients (62%; bifocal continue group, BCG) had to continue using bifocal glasses until the final visit, which was 13.8 years on average (range, 11.3 to 18.5 years). The AC/A ratio decreased from time of bifocal prescription to the last visit in both groups, from 4.4 to 2.7 in the BSG and from 5.9 to 4.5 in the BCG. AC/A ratios were significantly higher (p = 0.03) in the BCG than that of the BSG from the beginning of bifocal treatment and this difference was persistent until the final visit (p = 0.03).
Conclusions
The AC/A ratio decreased with age in both groups but was significantly higher throughout the entire follow-up period in the BCG. AC/A ratio at bifocal prescription could be an important factor in predicting response to bifocal treatment.
Go to :

Keywords: Accommodation, Convergence, Esotropia
Nonrefractive accommodative esotropia is a condition that is diagnosed when an emmetropically corrected patient with a high accommodative convergence to accommodation (AC/A) ratio shows orthotropia at distance fixation but displays more than 10 prism diopters of esotropia at near fixation which can be corrected with a +3.00 diopter add lens.
The AC/A ratio is the amount of induced convergence that occurs when accommodation is exerted. In normal eyes, the ratio is thought to remain stable without change until presbyopia, after which the AC/A ratio increases [
1-
3]. However, the change of the AC/A ratio with age in nonrefractive accommodative esotropia has not yet been studied.
Nonrefractive accommodative esotropia can be treated with bifocal lenses or miotics [
4-
9]. Miotics pharmacologically decrease accommodative convergence and correct esotropia at near fixation. Long term effects of miotics have been studied in detail and reports of iris cysts, cataracts, retinal detachment, iridocyclitis and punctal occlusion are abundant in the literature and thus are used only for diagnostic purposes or for short term correction. Bifocal lenses horizontally divide the visual field with a +2.50 - +3.00 diopters add lens in the lower portion and uses the upper and lower portions for distance and near fixation, respectively. Bifocal glasses induce orthotropia for both far and near vision and decrease chances of amblyopia with appropriate development of stereopsis.
As patients grow older, some can discontinue the use of bifocal lenses due to spontaneous normalization of the AC/A ratio [
10], but others need to keep their bifocal lenses or undergo strabismus surgery in an attempt to eliminate the need for bifocals [
11-
13]. Surgical options include augmented recession, slanted recession, and recession with posterior fixation suture of the medial rectus muscles [
12,
14,
15].
The AC/A ratio can be calculated in several ways, among which only the lens gradient method gives a true estimate of the ratio. In the lens gradient method, the change in stimulus to accommodation is produced by means of an ophthalmic lens, not a change in viewing distance. Franceschetti and Burian [
16] reported that the normal range of the AC/A ratio by the lens gradient method is lower than that by the heterophoria method. The heterophoria method does not account for proximal convergence, which is kept constant in the lens gradient method by performing both measurements at the same distance [
17]. Previous studies did not evaluate the AC/A ratio by the lens gradient method, but by heterophoria methods [
9,
18]. However, in this study we computed the AC/A ratio by the lens gradient method.
Materials and Methods
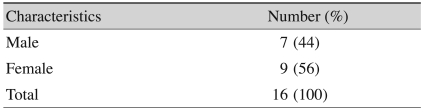
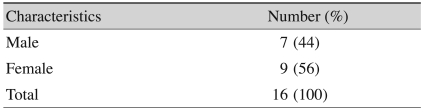
Medical records of nonrefractive accommodative esotropia patients who were treated with bifocal glasses for at least 5 years were retrospectively reviewed. Sixteen patients were included (
Table 1). Institutional review board approval was obtained for this study and the research adhered to the tenets of the Declaration of Helsinki. Patients who received strabismus surgery, which could affect the AC/A ratio, were excluded. Visual acuity, angle of deviation at near and distance fixation, cycloplegic refraction, and the AC/A ratio at each follow-up visit were collected. Ocular alignment was measured with the prism cover test, and cycloplegic refraction was assessed approximately 30 minutes after final instillation of two topical eye drops of Cyclogyl (cyclopentolate 1.0%) and Mydrin-P (tropicamide 0.5% and phenylephrine 0.5%), which were used three times at 10 minute intervals. Complete cycloplegia was confirmed by no pupillary response to light.
Table 1
Sex distribution of included 16 patients with nonrefractive accommodative esotropi

In this study, we computed the AC/A ratio by the lens gradient method using the angle of deviation with and without +3.00 lenses at near fixation. The AC/A ratio was calculated from the difference between the upper and lower segments of a bifocal lens which was divided by the added power of the lower segment.
Bifocal lenses were prescribed if the angle of esodeviation with near fixation was at least 10 prism diopters greater than the angle with distance fixation with full optical correction and the angle of esodeviation with near fixation could be eliminated or nearly eliminated with plus spherical lenses. Plus adds were initially prescribed from +2.50 to +3.00 diopters but were decreased to +2.50 diopters during the follow up period if a patient who was prescribed +3.00 diopters at initial visit showed orthotropia at near fixation.
During the course of follow-up, cycloplegic refractions were performed semiannually, and the diopters of glasses were adjusted if the refractive error had changed. Bifocals were discontinued if the patient was able to keep fusion at near through distance correction lenses and showed no or only minute differences in angle of deviation at both distance and near fixation. Binocular vision was also tested when stopping bifocals.
Statistical analysis was performed using descriptive analysis and the Mann-Whitney U-test. A p-value of <0.05 was considered statistically significant. SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA) was used.
Go to :

Results
Patient demographics
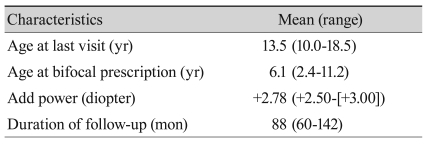
Tables 1 and
2 show the demographic data of 16 patients who were included (
Table 1). Average age at last visit was 13.5 years (range, 9.4 to 18.5 years) and the average age at bifocal prescription was 6.1 years (range, 2.4 to 11.2 years). Average follow-up duration was 88 months (range, 60 to 142 months). Average added power was +2.78 diopters (
Table 2).
Table 2
Characteristics of 16 patients with nonrefractive accommodative esotropia
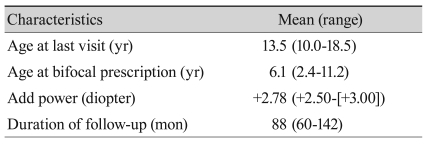

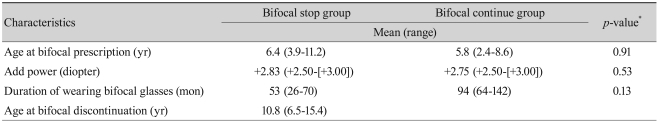
Comparisons of bifocal stop group and bifocal continue group
Of the 16 patients, six patients (38%), referred to as the bifocal stop group (BSG), were able to stop using bifocal lenses at an average age of 10.8 years during their follow-up, and ten patients (62%), referred to as the bifocal continue group (BCG), continued using bifocal lenses until their last visit (
Table 3).
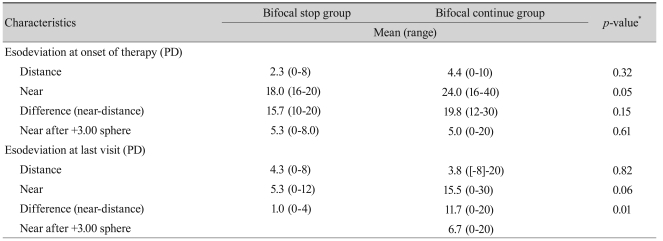
Table 3
Clinical characteristics of 16 patients with nonrefractive accommodative esotropia grouped according to therapeutic results
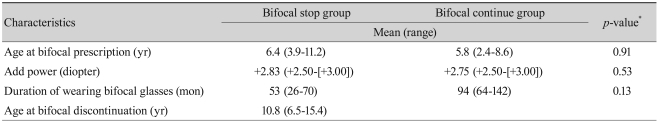

The mean angle of esodeviation at near fixation at prescription in the BCG was 24 prism diopters, which was significantly larger than the 18 prism diopters in the BSG. Differences of angle of deviation between distance and near fixation in the BCG were 19.8 prism diopters, which were larger than the 15.7 prism diopters in BSG (
Table 4).
Table 4
Esodeviation of two groups according to therapeutic results

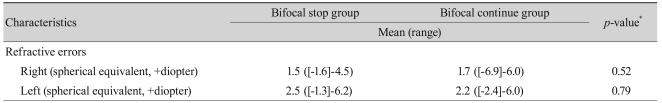
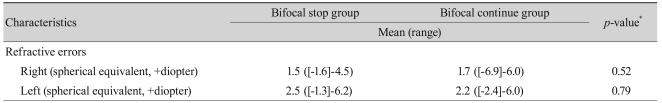
The average refractive errors in BSG were 1.5 diopters in the right eye and 2.5 diopters in the left eye, which were not significantly different with those in the BCG (
Table 5).
Table 5
Refractive errors in two groups according to therapeutic results

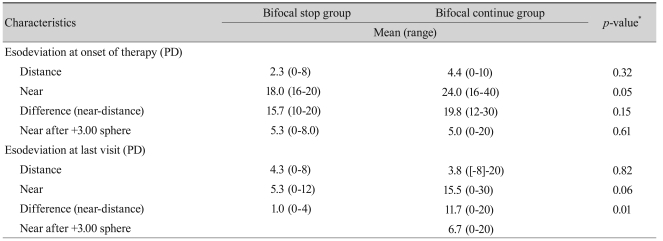
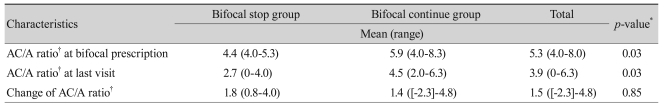
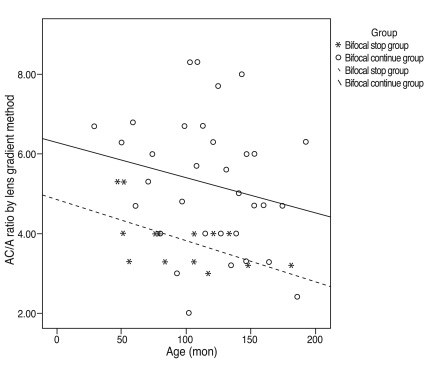
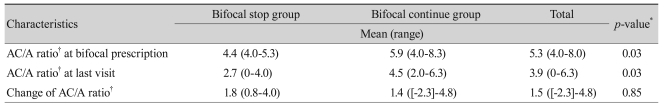
Change in accommodative convergence to accommodation ratio over time for the two groups
The AC/A ratio decreased with age from 4.4 to 2.7 in the BSG and from 5.9 to 4.5 in the BCG (
Table 6). The AC/A ratio at bifocal prescription in the BSG was 4.4, which was significantly lower than the 5.9 in the BCG (
p = 0.03). The AC/A ratio at last visit in the BSG was 2.7, which was significantly lower than the 4.5 in the BCG. The AC/A ratio decreased with age in both groups, but the initially higher AC/A ratio of the BCG remained higher than that of the BSG until the last visit. The AC/A ratio changes very slowly with age. As the graphs depicting the change in AC/A ratio over time for the two groups show, the decrease in the AC/A ratio with age was 0.01 per 1 month in both groups (
Fig. 1).
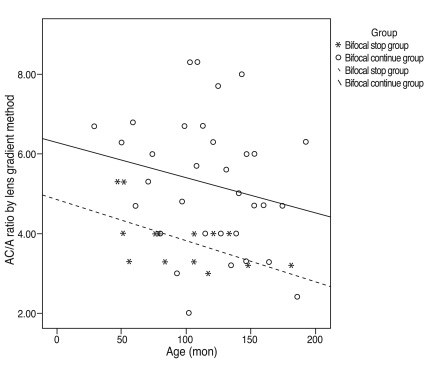 | Fig. 1Regression graph of the change in accommodative convergence to accommodation (AC/A) ratio according to age in the bifocal stop group compared with the bifocal continue group. Graphs depicting change in AC/A ratio over time for two groups show a decrease in AC/A ratio with age, -0.01 × (age) + 4.84 in the bifocal stop group and -0.01 × (age) + 6.28 in the bifocal continue group. 
|
Table 6
The change in AC/A ratio of 16 patients with nonrefractive accommodative esotropia

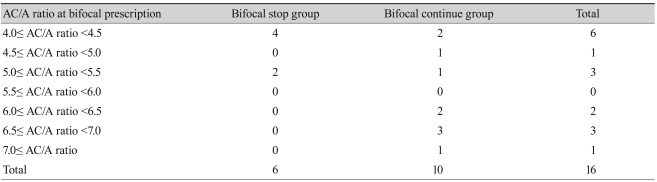
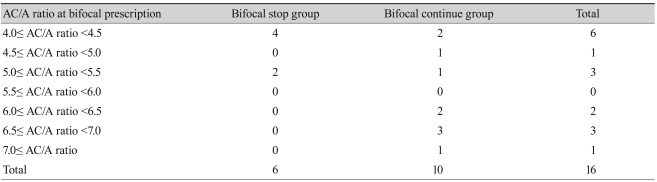
Initial accommodative convergence to accommodation ratio at bifocal prescription in both groups
All of the AC/A ratios of the BSG at bifocal prescription were less than 5.5, but the AC/A ratios of the BCG were distributed over a range from 4.0 to above 7.0 (
Table 7). No patient in the BSG had an AC/A ratio of more than 5.5 at time of bifocal prescription.
Table 7
The AC/A ratio of two groups at the time of bifocal glasses prescription

Go to :

Discussion
Treatment with bifocals to correct residual near esodeviation is a well-established and popular method for patients with nonrefractive accommodative esotropia [
10,
18]. In this study, about one-third of patients with nonrefractive accommodative esotropia were able to stop using bifocal lenses during follow-up without surgery. The AC/A ratio of these patients, measured by the lens gradient method, decreased with age and normalized. Binocular fusion was made by a spontaneous decrease of esodeviation at near fixation [
19]. A previous study reported that 37.0% (31 / 84) of patients were either cured or improved with bifocals [
19]. Another study reported that 61.5% (40 / 65) of patients were able to stop using bifocals at an average age of 9.7 years [
10].
The average age at bifocal discontinuation in this study was 10.8 years, which is older than that of the study just mentioned. The average bifocal discontinuation age of 10.8 years in this study may indicate that surgical treatment of nonrefractive accommodative esotropia can be delayed until this age. Other reports have revealed good postoperative outcomes following strabismus surgery at even younger ages, but a second surgery was required more frequently in younger patients [
10,
11]. In this study, there were six patients who received strabismus surgery because of uncontrolled esotropia, even with bifocal lenses, during follow-up. We excluded these patients to avoid the possible effect of surgery on the AC/A ratio [
20-
22].
The unique benefit of this study is that AC/A ratios were computed by the lens gradient method, which gives a true estimate of the AC/A ratio. The gradual decrease of the AC/A ratio with age in nonrefractive accommodative esotropia was revealed in this study, which corresponds well with observations from previous studies [
9,
10]. The rates of decrease were 0.01 per 1 month, which were similar in both groups in this study.
In this study, the factor that determined whether the final AC/A ratio became normal was the initial AC/A ratio at bifocal prescription. The initial AC/A ratios of the BSG were significantly lower than that of the BCG. This finding is in contrast to a previous report that found that the higher the initial AC/A ratio, the higher the chance of bifocal discontinuation [
19]. All of the patients in the bifocal stop group had an AC/A ratio of less than 5.5 at their bifocal prescription. This suggests that the AC/A ratio at bifocal prescription could be important in predicting response to bifocal treatment.
In this study, about 30% of patients with nonrefractive accommodative esotropia were able to stop using bifocal lenses spontaneously during follow-up. The average age at bifocal discontinuation in this study was 10.8 years. This may indicate that surgical treatment of nonrefractive accommodative esotropia to eliminate the need for bifocal glasses should be deferred until patients reach this age.
The AC/A ratio decreased with age in all cases of nonrefractive accommodative esotropia, but the initially higher AC/A ratios remained higher. Furthermore, a low AC/A ratio of less than 5.5 at the time of bifocal prescription could be good prognostic factor in bifocal treatment.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download