Abstract
An 81-year-old woman with a raised pigmented nodule over her left cornea for 7 months duration was examined. Dark conjunctival pigmentation was observed in the upper bulbar fornix conjunctiva. She had previously undergone primary surgical excision of a malignant conjunctival melanoma four years earlier. The tumor separated easily from the corneal surface, but remained slightly attached to the corneoscleral surface. A corneoscleral lamellar dissection of 3 mm in width and 2 mm in depth as well as a corneoscleral lamellar keratoplasty for the reconstruction of the corneoscleral defect were performed. The wide upper bulbar and fornix conjunctiva were excised, and an amniotic membrane transplantation was performed. Biopsy revealed an invasive melanoma with a depth of 1 mm. Left, right, and inferior tumor margins of the corneoscleral lesion and the pigmentary lesion in the conjunctiva were free of the tumor. After surgery, 0.04% mitomycin was administered topically 4 times daily for 4 weeks. There was no recurrence 2 years after surgery, and systemic evaluation revealed no metastasis.
Conjunctival melanomas are a rare unilateral disease comprising 2% of all ocular melanomas [1]. Malignant melanomas grow on the cornea without evidence of invasive conjunctival tumors [2]. The incidence of a corneal displaced conjunctival melanoma remains unknown. Previous studies have reported that more than 50% of patients have local tumor recurrence after ocular treatment [3,4].
In the past, conjunctival malignant melanomas were treated by primary orbital exenteration [5]. This radical treatment has been more recently found to be less effective than previously described. More recently local resection has generally been performed [6]. Cryotherapy has been developed for an adjuvant treatment after local excision [7]. Topical chemotherapy with mitomycin C (MMC), adjuvant radiotherapy, and topical and subconjunctival injection of Interferon alfa-2b have also been performed as adjuvant treatments after local excision [8-10]. In the past, when the size of the conjunctival defect is too large for primary closure after local excision, autografts of conjunctiva from the fellow eye or oral mucosa have been performed [7]. More recently, reconstruction with a preserved amniotic membrane to close large conjunctival defects after excision of wide tumors has been reported [11]. In an invasive corneal displaced melanoma, lamellar dissection of the cornea, and reconstruction with corneoscleral tissue is required after removal of the invasive tumor. However, there have been no reports on lamellar dissection of the cornea and reconstruction with corneoscleral tissue.
We report, to the best of our knowledge, the first case of surgical excision of a corneal displaced recurrent conjunctival melanoma and reconstruction with a corneoscleral lamellar keratoplasty and amniotic membrane transplantation (AMT).
An 81-year-old woman was examined for a raised pigmented nodule over her left cornea for 7 months duration, which disturbed vision and blinking. She had previously undergone primary surgical excision of a malignant conjunctival melanoma four years earlier (Fig. 1). Visual acuity was 8 / 20, and the right eye was normal. A pale, lightly pigmented, vascularized tumor was present superiorly in her left eye, parallel to the the adjacent limbus. Dark conjunctival pigmentation was observed in the upper bulbar conjunctiva and fornix area. The tumor separated easily from the corneal surface, but remained slightly attached to the corneoscleral surface. Corneoscleral lamellar dissection on the melanoma mass that measured 3 mm in width and 2 mm in depth and corneoscleral lamellar keratoplasty for reconstruction of the corneoscleral defect were performed. The wide upper bulbar and fornix conjunctiva were excised for evaluation of tumor invasion, and an AMT was performed for reconstruction of the large conjunctival defects (Fig. 2). Biopsy revealed an invasive conjunctival melanoma with 1 mm depth of invasion under the conjunctival epithelium (Fig. 3). The total thickness of the specimen was 3 mm. There was also slight invasion in the corneal stroma. However, the remaining tumor margins in the corneoscleral lesion were free of tumor cells. The pigmentary lesion in the upper bulbar and fornix conjunctiva revealed a pigmentary macrophage in the subconjunctiva, but no melanoma cells. After surgery, 0.04% mitomycin was administered topically four times daily for 4 weeks. No tumor recurrence had appeared in the superior cornea and conjunctiva 2 years after surgery. Systemic evaluation revealed no metastases.
This case demonstrates the successful use of a corneoscleral lamellar keratoplasty and an AMT for the reconstruction of ocular surface defects following surgical excision of a corneal displaced recurrent conjunctival melanoma. The advantages of an AMT for surgery of a conjunctival melanoma include: 1) cosmetic appearance following surgery, 2) the absence of donor site morbidity complicating the harvest of mucosal autografts, and 3) the ability to clinically monitor local recurrence of tumors underneath the transparent amniotic membrane graft [12]. In this case, dark conjunctival pigmentation was observed in the upper bulbar conjunctiva and fornix area. We excised the wide upper bulbar and fornix conjunctiva for evaluation of tumor invasion. AMT was necessary for the reconstruction of the wide conjunctival defects in the whole upper bulbar and fornix area.
In addition to local recurrence and metastasis, limbal melanomas may rarely show intraocular extension [13]. A case study of a conjunctival melanoma with intraocular extension was attributed a previous surgery in which Bowman's membrane was penetrated and removing its effect as a barrier [14].
In conventional local resection of an invasive corneoscleral melanoma with adjunctive therapy, there is a risk of intraocular extension of the invasive melanoma because of a defect in Bowman's membrane [14].
In this case, we felt the conjunctival melanoma was slightly attached to the corneoscleral surface during surgery. Therefore, we performed a lamellar dissection of the corneoscleral area to evaluate local tumor invasion. The corneoscleral surface was elevated due to the conjunctival melanoma. A corneoscleral lamellar dissection with a depth of 2 mm including the thickness of the melanoma was necessary. We performed a corneoscleral lamellar keratoplasty for the reconstruction of Bowman's membrane in the corneoscleral area. In conventional surgery, deep excision is difficult because corneoscleral thinning may result after surgery, increasing the risk of an intraocular extension of the invasive melanoma due to a defect in Bowman's membrane. In comparison with conventional surgery, corneoscleral lamellar keratoplasty may be useful in preventing intraocular extension of a recurrent melanoma if there is a danger of damaging Bowman's membrane during surgery. An AMT was also helpful for the reconstruction of the wide conjunctival defects in the upper bulbar and fornix area.
Topical mitomycin, 5-fluorouracil (5-FU), and Interferon alfa-2b have been used alone or as adjunctive treatments for conjunctival primary acquired melanosis (PAM) with atypia and conjunctival melanoma [15]. MMC is an alkylating agent that binds to DNA during all phases of the cell cycle, leading to irreversible cross-linking, and inhibition of nucleotide synthesis [15]. Chalasani et al. [16] reported that the overall recurrence rate in patients receiving MMC as an adjuvant therapy was 43%, while Shields et al. [17] reported that the recurrence rate was 0%. The major side-effect of MMC was transient keratoconjunctivitis that resolved following cessation. MMC is the most widely used agent for PAM with atypia and conjunctival melanoma. 5-FU is also an antimetabolite used to treat many epithelial cancers because of its action on rapidly proliferating cells [15]. Midena et al. [18] reported that the recurrence rate was 12.5% after treatment with topical 1% 5-FU in conjunctival squamous cell carcinoma, and recurrence cases were successfully retreated with a second 4-week course of topical 5-FU. The exact mechanism of Interferon alfa-2b is not completely understood, but it seems to play an indirect immunoregulatory role rather than having a direct antitumor mechanism [19]. Finger et al. [19] reported that for primary or recurrent malignant melanoma, the lesions regressed without side effects two months after topical Interferon alfa-2b treatment. We used topical 0.04% mitomycin for adjuvant therapy after surgery, and no tumor recurrence or complications were observed 2 years after surgery.
To the best of our knowledge, this is the first case of the surgical excision of corneal displaced recurrent conjunctival melanoma and reconstruction with corneoscleral lamellar keratoplasty and AMT. We hypothesize that if there is a risk of a conjunctival melanoma attaching to the corneoscleral surface, a corneoscleral lamellar keratoplasty may be useful to prevent intraocular extension. An AMT may be necessary for the reconstruction of conjunctival defects after wide resection of the conjunctival melanoma. Adjuvant topical 0.04% mitomycin may be efficient in preventing local tumor recurrence.
Figures and Tables
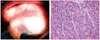 | Fig. 1(A) Pigmented lesion on the bulbar conjunctiva and cornea of the left eye. (B) Epithelioid melanoma cells infiltrations were observed by hematoxylin & eosin stain (×400). This patient had an epithelioid conjunctival melanoma with corneal displacement. The pictures were taken 4 years previously. |
 | Fig. 2Surgical excision of a corneal-displaced recurrent conjunctival melanoma, and reconstruction with corneoscleral lamellar keratoplasty and amniotic membrane transplantation. (A) Preoperative finding. (B) Corneoscleral lamellar dissection with a width of 3 mm and a depth of 2 mm was performed. (C) Donor corneoscleral lamellar tissue was prepared. (D) Corneoscleral lamellar keratoplasty was performed. (E) Pigmentary lesion of the wide upper bulbar and fornix conjunctival was excised. (F) Amniotic membrane transplantation was performed. |
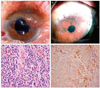 | Fig. 3(A) Preoperative corneal displaced recurrent conjunctival melanoma. (B) Postoperative ocular findings showing a well-removed pigmented mass and well-attached corneoscleral lamellar keratoplasty. (C) Epithelioid melanoma cells can be observed by hematoxylin & eosin stain (×400). (D) Positive staining for HMB 45 in melanoma cells (×200). |
Acknowledgements
This work was supported by National Research Foundation of Korea Grant founded by the Korean Government (2012038648).
References
1. Layton C, Glasson W. Clinical aspects of conjunctival melanoma. Clin Experiment Ophthalmol. 2002. 30:72–79.
2. Kim SY, Lee SB, Yang SW. A case of conjunctival malignant melanoma with extensive corneal displacement. J Korean Ophthalmol Soc. 2005. 46:1235–1239.
3. Shields CL. Conjunctival melanoma: risk factors for recurrence, exenteration, metastasis, and death in 150 consecutive patients. Trans Am Ophthalmol Soc. 2000. 98:471–492.
4. Anastassiou G, Heiligenhaus A, Bechrakis N, et al. Prognostic value of clinical and histopathological parameters in conjunctival melanomas: a retrospective study. Br J Ophthalmol. 2002. 86:163–167.
5. Paridaens AD, McCartney AC, Minassian DC, Hungerford JL. Orbital exenteration in 95 cases of primary conjunctival malignant melanoma. Br J Ophthalmol. 1994. 78:520–528.
6. Damato B, Coupland SE. Management of conjunctival melanoma. Expert Rev Anticancer Ther. 2009. 9:1227–1239.
7. Shields JA, Shields CL, De Potter P. Surgical management of circumscribed conjunctival melanomas. Ophthal Plast Reconstr Surg. 1998. 14:208–215.
8. Finger PT. Topical mitomycin chemotherapy for malignant conjunctival and corneal neoplasia. Br J Ophthalmol. 2006. 90:807–809.
9. Lederman M, Wybar K, Busby E. Malignant epibulbar melanoma: natural history and treatment by radiotherapy. Br J Ophthalmol. 1984. 68:605–617.
10. Schechter BA, Schrier A, Nagler RS, et al. Regression of presumed primary conjunctival and corneal intraepithelial neoplasia with topical interferon alpha-2b. Cornea. 2002. 21:6–11.
11. Dalla Pozza G, Ghirlando A, Busato F, Midena E. Reconstruction of conjunctiva with amniotic membrane after excision of large conjunctival melanoma: a long-term study. Eur J Ophthalmol. 2005. 15:446–450.
12. Paridaens D, Beekhuis H, van Den Bosch W, et al. Amniotic membrane transplantation in the management of conjunctival malignant melanoma and primary acquired melanosis with atypia. Br J Ophthalmol. 2001. 85:658–661.
13. Sandinha T, Russell H, Kemp E, Roberts F. Malignant melanoma of the conjunctiva with intraocular extension: a clinicopathological study of three cases. Graefes Arch Clin Exp Ophthalmol. 2007. 245:431–436.
14. Wenkel H, Rummelt V, Naumann GO. Malignant melanoma of the conjunctiva with intraocular extension. Arch Ophthalmol. 2000. 118:557–560.
15. Kim JW, Abramson DH. Topical treatment options for conjunctival neoplasms. Clin Ophthalmol. 2008. 2:503–515.
16. Chalasani R, Giblin M, Conway RM. Role of topical chemotherapy for primary acquired melanosis and malignant melanoma of the conjunctiva and cornea: review of the evidence and recommendations for treatment. Clin Experiment Ophthalmol. 2006. 34:708–714.
17. Shields CL, Shields JA, Armstrong T. Management of conjunctival and corneal melanoma with surgical excision, amniotic membrane allograft, and topical chemotherapy. Am J Ophthalmol. 2001. 132:576–578.
18. Midena E, Angeli CD, Valenti M, et al. Treatment of conjunctival squamous cell carcinoma with topical 5-fluorouracil. Br J Ophthalmol. 2000. 84:268–272.
19. Finger PT, Sedeek RW, Chin KJ. Topical interferon alfa in the treatment of conjunctival melanoma and primary acquired melanosis complex. Am J Ophthalmol. 2008. 145:124–129.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download