Abstract
Purpose
To report the three-year outcomes of macular laser photocoagulation following intravitreal injection of triamcinolone acetonide (IVTA) for diffuse diabetic macular edema (DME).
Methods
A prospective, randomized controlled study was completed. Eighty-six eyes of 74 patients with diffuse DME were randomized into two groups. Eyes assigned to the combination group (n = 48) were subjected to macular laser photocoagulation three weeks after IVTA. Eyes in the IVTA group (n = 38) underwent IVTA alone. Central macular thickness was measured by optical coherence tomography, and the number of additional treatments and mean time to recurrence were assessed.
Results
Thirty-seven eyes in the combination group and 26 eyes in the IVTA group completed the three-year follow-up. Recurrence of DME after initial treatment was not observed for nine of the 37 (24.3%) eyes in the combination group or for one of the 26 (3.9$) eyes in the IVTA group (p = 0.028). DME was absent for 19.9 months after treatment in the combination group compared to 10.3 months in the IVTA group (p = 0.027). The mean number of additional treatments was 0.92 in the combination group and 1.88 in the IVTA group (p = 0.001).
Conclusions
Results in the subset of subjects who completed the three-year follow-up demonstrated that laser photocoagulation following IVTA is more effective than IVTA monotherapy for diffuse DME. Combination therapy required fewer additional treatments and resulted in a lower recurrence rate than IVTA monotherapy.
Since the report from the Early Treatment Diabetic Retinopathy Study, macular laser photocoagulation has been widely accepted as the treatment of choice for clinically significant macular edema (CSME). However, intractable diabetic macular edema (DME) is a well-known limitation of this treatment [1-3]. A recent large clinical trial showed favorable results after laser photocoagulation for DME, but 12% of the eyes in the trial still had worsening of 10 or more letters at the three-year follow-up [4]. Although intravitreal injection of triamcinolone acetonide (IVTA) is a potent treatment method, it has some limitations. Many investigators have reported excellent short-term outcomes, but the effect of IVTA is usually only maintained for a period of several months; as a result, frequent repeat injections may be necessary [5-7]. In addition, DME refractory to IVTA is also an issue. Therefore, IVTA, which is expected to decrease central macular thickness (CMT) over a short period of time, has been employed for the reinforcement of laser photocoagulation, which is more effective for treating DME with CMT less than 400 µm [8,9].
In a randomized, multicenter clinical trial, the Diabetic Retinopathy Clinical Research (DRCR) Network showed that IVTA plus prompt laser therapy seems to be more effective in pseudophakic eyes than laser therapy alone [10]. In a recent randomized clinical trial of eyes with DME, IVTA plus laser therapy resulted in a marked improvement in vision (by 10 letters or more) compared with laser therapy only. Gillies et al. [11] found that IVTA can be a useful adjunct to laser treatment in the management of DME. We previously reported a six-month result from a prospective comparative clinical trial showing that macular grid photocoagulation subsequent to IVTA is more effective than IVTA monotherapy [8]. Eyes treated with the combination therapy showed better logarithm of the minimum angle of resolution (logMAR) best-corrected visual acuity (BCVA) at three- and six-month follow-up visits. The maintenance of reduced central macular thickness was noted after six months of follow-up. However, these results were not replicated in a subsequent study, although a similar trend was noted [12]. Therefore, it is expected that a longer follow-up period will confirm the validity of combination therapy. The purpose of this study was to assess the three-year outcomes of laser photocoagulation following IVTA in the treatment of DME.
Eighty-six eyes from 74 diabetic individuals were included in this study. The demographics and clinical characteristics have been described previously [8]. Patients diagnosed with diffuse DME at Samsung Medical Center between September 2003 and August 2004 were enrolled. Diffuse DME was defined as macular thickening corresponding to CSME on biomicroscopy with findings of diffuse fluorescein leakage without a responsible microaneurysm on angiography and increased CMT (>250 µm) on optical coherence tomography [8]. All decisions on diagnosis and additional treatments were made by the same physician.
The eligible eyes were randomized into either the combination group or the IVTA group. Eyes in the combination group underwent modified macular grid/focal laser photocoagulation three weeks after IVTA. Four milligrams of triamcinolone were injected intravitreally after sterilization with betadine using a sterile lid speculum. Modified grid laser photocoagulation, which consisted of grid patterned laser burns on the capillary non-perfusion area, retinal thickening of the parafoveal region, and direct photocoagulation on the leaking microaneurysms were performed as described previously [8]. Eyes in the IVTA group were treated with IVTA alone.
All patients underwent a complete ocular examination, including assessment of best corrected visual acuity on a Snellen chart, applanation tonometry, slit lamp examination, dilated fundus examination utilizing biomicroscopy, fundus fluorescein angiography, and optical coherence tomography (OCT; Stratus OCT ver. A 3.0, Carl Zeiss Meditec, Dublin, CA, USA). Central macular thickness was automatically measured by OCT.
Responses after treatment were evaluated with respect to best corrected visual acuity and central macular thickness on OCT. Best corrected visual acuity was converted to a logarithmic scale (logMAR) for statistical analysis. Slit lamp biomicroscopy, fundus examination, and measurement of intraocular pressure were conducted at each follow-up visit. This study was initially performed as a prospective study for six months; the results are described in a previous report [8]. After the initial six-month follow-up, visits were made every 3 to 4 months at the physician's discretion (SWK). OCT examination was performed when 1) funduscopy revealed any macular change or 2) visual acuity changed. Additional treatment was applied at least six months after the initial treatment. If the funduscopy and OCT showed apparent macular edema, additional treatment (such as macular photocoagulation, IVTA, a combination of the two, or pars plana vitrectomy with IVTA followed by macular photocoagulation) was completed. The choice of additional treatment was based primarily on the tomographic and angiographic appearance of the recurrent DME [13].
For diffuse DME with cystoid intraretinal fluid or subretinal fluid accumulation, IVTA and laser photocoagulation were considered if the eye had previously been included in the group receiving only IVTA. In the most intractable cases, sequential triple therapy of vitrectomy and IVTA followed by macular laser photocoagulation was performed [12].
The demographics and clinical characteristics of the patients (age, duration of diabetes, number of prior focal/grid laser photocoagulation treatments, central macular thickness, and logMAR visual acuity) were analyzed by a two-tailed t-test. Sex, extent of diabetic retinopathy, and presence of systemic hypertension were evaluated with Fisher's exact test. Initial response was determined at the six-month follow-up visit in eyes that completed the three-year follow-up. Initial response was defined as resolution of macular edema (CMT measured via OCT <250 µm). Kaplan-Meier survival analysis with log ranks for DME recurrence was employed to evaluate the duration of DME resolution. Recurrence of DME was defined as 1) CMT greater than 250 µm or 2) the need for additional treatment of macular edema in eyes that had initially responded to treatment.
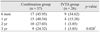
The mean follow-up period was 30.7 ± 11.2 months (range, 6 to 41 months) for the combination group and 32.5 ± 10.1 months (range, 6 to 40 months) for the IVTA group. Among 86 eyes from 74 patients, 67 eyes from 56 patients completed the three-year follow-up. Of those 67 eyes, two in the combination group and two in the IVTA group were excluded from analysis because pars plana vitrectomy was performed for reasons other than macular edema. Three eyes (two eyes in the combination group and one eye in the IVTA group) underwent pars plana vitrectomy for proliferative diabetic retinopathy complicated by vitreous hemorrhage. One eye in the IVTA group was subjected to pars plana vitrectomy for an epiretinal membrane. A total of 63 eyes from 52 patients were eventually included in this study. Clinical and demographic characteristics at baseline and at six months for patients who did and did not complete the three-year follow-up are summarized in Table 1. No significant differences between those who did and did not complete follow-up were observed at baseline or at six months. Thirty-seven eyes in the combination group and 26 eyes in the IVTA group were evaluated for three years. Baseline features, including visual acuity, CMT, stage of retinopathy, mean duration of diabetes, lens status, and number of prior macular photocoagulation procedures, did not differ between the two groups (Table 2).
Throughout the three-year follow-up period, macular edema was not observed in nine of 37 eyes (24.32%) in the combination group that did not receive additional treatment and in only one of 26 eyes (3.85%) in the IVTA group (p = 0.028) (Table 3). In eyes with initial response, recurrence of DME was absent in nine of 17 eyes (52.94%) in the combination group and in one of nine eyes (11.11%) in the IVTA group. In these eyes, macular edema was absent for an average of 19.88 months (up to 30 months) in the combination group and 10.33 months in the IVTA group (p = 0.027) (Fig. 1).
Although BCVA and CMT improved six months after treatment in both groups, the improvement was greater in the combination group than in the IVTA group (Table 2). BCVA and CMT were evaluated at one-, two-, and three-year follow-ups. For the nine eyes in the combination group that completed the three-year follow-up without additional treatment, logMAR visual acuity measurements at baseline, six months, and three years were 0.80 ± 0.34, 0.66 ± 0.37, and 0.53 ± 0.48, respectively. The respective CMT values were 481.9 ± 177.5, 157.5 ± 12.9, and 172.0 ± 37.4 µm. Because only three eyes in the IVTA group were exempt from additional treatment after the one-year follow-up, statistical analysis and comparison of BCVA and CMT were not feasible.
Nine (34.6%) eyes in the IVTA group and eight (21.6%) eyes in the combination group experienced IOP elevation in excess of 21 mmHg after initial treatment. However, this difference was not significant (p = 0.267). These eyes were treated with topical glaucoma medication, and IOP normalized after treatment in most cases. Glaucoma medications
were discontinued within six months in 17 eyes (94.1%). No evidence of glaucomatous damage to the optic nerve was observed. Trabeculectomy was performed in one eye due to intractable intraocular pressure elevation that normalized after surgery.
Cataract extraction was performed in 13 (38.2%) of 34 phakic eyes in the combination group compared to seven (26.9%) of 26 phakic eyes in the IVTA group. All cataract surgeries were performed successfully without intraoperative or postoperative complications. The mean time to cataract extraction was 15.54 months in the combination group and 19.14 months in the IVTA group. This difference was not statistically significant (p = 0.300). Other injection-related complications, including infectious endophthalmitis, vitreous hemorrhage, and retinal detachment, were not observed.
We previously reported on a six-month comparison between IVTA monotherapy and combined IVTA and laser photocoagulation. This comparison revealed that combined therapy resulted in greater improvement in BCVA and CMT [8]. Among the 86 eyes from 74 patients who were recruited in a previous study, 63 eyes from 56 patients were included in this report. Clinical and demographic characteristics of the patients who did and did not complete follow-up were compared for the evaluation of unexpected biases due to follow-up loss. No statistically significant difference was observed between these groups (Table 1). A comparison of clinical and demographic data at baseline between the combination group and IVTA group among patients who completed follow-up revealed no significant differences (Table 2). Therefore, we assumed that unexpected bias from loss to follow-up was not significant.
Compared with only one of 26 (3.85%) eyes in the IVTA group, nine of 37 (24.32%) eyes in the combination group sustained their normalized macular thickness up to the final follow-up visit. The proportion with persistent resolution of DME was significantly higher in the combination group than in the IVTA group (p = 0.028). The duration of DME resolution was also significantly longer in the combination group than in the group receiving IVTA only (p = 0.027). Seventeen eyes that initially responded to combination therapy had a significantly longer DME-free period than nine eyes in the IVTA group. It is also noteworthy that nine of the 17 eyes (52.9%) showing an initial response to combination therapy did not require additional treatment for diffuse DME for three years. These results suggest that a combination of IVTA and laser photocoagulation may have long-lasting effects with a lower recurrence rate.
The mean number of additional treatments in the combination group was 0.92, which was significantly smaller than the number in the IVTA group (1.88). In a large clinical trial conducted by the DRCR network, the mean number of treatments in eyes that underwent macular grid/focal photocoagulation was reported to be 3.1, and the mean frequency of treatments in eyes receiving a 4-mg intravitreal triamcinolone injection was 4 [14]. This discrepancy is believed to arise from the difference in the mode of additional treatments. Because our study targeted only diffuse DME, which is thought to be more intractable, we employed not only monotherapy (such as IVTA or laser photocoagulation), but also combination therapies (including pars plana vitrectomy, IVTA, and laser photocoagulation) that may have a longer duration of action [8,12]. Because most eyes (23 of 26 eyes) in the IVTA group required additional treatment after the one-year follow-up, a comparison of visual acuity and central macular thickness between the combination group and IVTA group was not feasible. BCVA and CMT improved gradually throughout the follow-up period in eyes in the combination group that did not undergo additional treatment. These changes in BCVA and CMT correspond with results from an earlier study that reported sustained improvement with gradual augmentation of visual acuity and CMT after macular grid/focal photocoagulation at the three-year follow-up [4].
We previously reported on the improvement in BCVA and CMT after macular focal/grid laser photocoagulation combined with IVTA at six months [8]. In another study, although CMT improvement at six months was better in the combination group, the difference in BCVA among the combination, laser, and IVTA groups was not statistically significant [9]. This dissimilarity between the two studies may originate from differences in baseline characteristics. The mean CMT of eyes in the former study was 525.4 µm, compared to 401.4 µm in the latter study. This disparity may be curtailed by long-term observation. Although improvement in BCVA did not immediately follow resolution of DME, improvement in CMT would be expected to contribute to the stabilization or improvement of BCVA in the long-run, as described in a previous study [4]. We hypothesized that macular grid/focal laser photocoagulation after IVTA would have its own role in 1) reduction of diabetic macular edema as a conventional concept of macular grid/focal photocoagulation and 2) maintenance of reduced macular thickness from IVTA. Estabrook et al. [13] reported that eyes with severe macular edema (>400 µm) responded poorly to macular grid/focal photocoagulation, while eyes with moderate macular edema (retinal thickness <400 µm) responded well. IVTA reduces macular thickness prior to macular grid/focal laser photocoagulation. We assume that macular grid/focal laser photocoagulation reduces retinal thickness by driving the equilibrium toward the absorption of intraretinal/subretinal fluid. A recent report from the DRCR network suggested that intravitreal ranibizumab with prompt or deferred laser therapy is more effective through at least two years than is prompt laser treatment alone or combination therapy with IVTA and macular grid/focal treatment. However, in a subgroup analysis limited to pseudophakic eyes, eyes treated with intravitreal triamcinolone combined with laser therapy showed comparable outcomes to those treated with intravitreal ranibizumab with prompt or deferred laser treatment [10]. In their analysis of all eyes (including phakic eyes), intravitreal triamcinolone combined with laser therapy failed to show effectiveness, unlike our main outcomes [10]. In their study, macular grid/focal photocoagulation was employed simultaneously with IVTA [10]. However, we prefer laser photocoagulation three weeks after the transitory reduction of CMT with IVTA to simultaneous application of laser photocoagulation and IVTA. We assume that the decreased foveal thickness and restoration of retinal transparency achieved by IVTA may selectively facilitate the delivery of laser energy to the photoreceptors and retinal pigment epithelia. Therefore, it is possible that the interval between IVTA and macular grid/focal photocoagulation can lead to dissimilar results.
In addition, intravitreal triamcinolone combined with laser treatment increased subsequent cataract surgery, which can induce pseudophakic macular edema of varying severity [14]. As a result, this might be a factor that increases the recurrence of DME. We carefully determined the timing of cataract surgery to minimize postoperative inflammation. All cataract surgeries were performed by an experienced cataract surgeon without complications after we confirmed complete resolution of macular edema and lack of neovascular activity. Uncomplicated cataract surgery and optimal timing may minimize postoperative inflammation. These may be unknown confounding factors that account for the difference in outcomes between this study and the recent study from the DRCR network [10].
Intravitreal administration of an anti-vascular endothelial growth factor (VEGF) agent is one of the most promising treatment modalities for DME and has several advantages compared to IVTA. Recent studies have demonstrated favorable results without significant complications, such as elevated intraocular pressure or cataract progression [15-17]. However, because DME recurrence after administration of an anti-VEGF agent is common, repeat administration is often required, which can be hazardous [18,19]. The long-term effectiveness of combination therapy for DME shown in this study may be helpful in attempts to maintain the effect with fewer injections, using modalities such as anti-VEGF and laser photocoagulation. Recently, a large clinical trial showed that a combination of intravitreal ranibizumab injection and prompt or deferred laser treatment resulted in greater visual improvement than did a combination of IVTA and prompt laser photocoagulation, although both treatments resulted in significant anatomical improvement [10]. Although anti-VEGF injection and laser photocoagulation demonstrated more favorable outcomes, considering the different mode of action, a combination of IVTA and laser photocoagulation may also be an alternative treatment option, particularly in pseudophakic eyes.
The primary weakness of this study is that it was originally designed as a prospective study with a six-month follow-up. Thus, after the initial six months, the follow-up intervals were irregular. Treatment for persistent or recurrent DME after the initial six months depended on the physician's discretion based on angiographic and tomographic findings, not on a given protocol. However, despite these weaknesses, because this study includes long-term results from a combination regimen, this report provides a long-term perspective on the clinical course of treatment after combination therapy for DME.
In summary, this study presented the superiority of combination therapy at six month and three year follow-ups. Although combination therapy showed more favorable results than IVTA monotherapy, DME recurrence was common. Therefore, we suggest that macular laser photocoagulation following resolution of edema through IVTA can be an alternative therapeutic option for the treatment of recurrent or intractable DME.
Figures and Tables
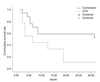 | Fig. 1Kaplan-Meier survival plot of diabetic macular edema recurrence. Seventeen eyes in the combination group and nine eyes in the intravitreal injection of triamcinolone acetonide (IVTA) group initially responded. Nine eyes in the combination group and one eye in the IVTA group completed the three-year follow-up without recurrence. Mean time to recurrence was 10.33 months (limited to 30 months) in the IVTA group and 19.88 months in the combination group (p = 0.027). |
Table 1
Demographic and clinical characteristics of patients who did and did not complete the three-year follow-up period

References
1. Early Treatment Diabetic Retinopathy Study research group. Photocoagulation for diabetic macular edema. Early Treatment Diabetic Retinopathy Study report number 1. Arch Ophthalmol. 1985. 103:1796–1806.
2. Bresnick GH. Diabetic maculopathy: a critical review highlighting diffuse macular edema. Ophthalmology. 1983. 90:1301–1317.
3. Lee CM, Olk RJ. Modified grid laser photocoagulation for diffuse diabetic macular edema: long-term visual results. Ophthalmology. 1991. 98:1594–1602.
4. Diabetic Retinopathy Clinical Research Network (DRCR.net). Beck RW, Edwards AR, et al. Three-year follow-up of a randomized trial comparing focal/grid photocoagulation and intravitreal triamcinolone for diabetic macular edema. Arch Ophthalmol. 2009. 127:245–251.
5. Jonas JB, Degenring RF, Kamppeter BA, et al. Duration of the effect of intravitreal triamcinolone acetonide as treatment for diffuse diabetic macular edema. Am J Ophthalmol. 2004. 138:158–160.
6. Jonas JB, Sofker A. Intraocular injection of crystalline cortisone as adjunctive treatment of diabetic macular edema. Am J Ophthalmol. 2001. 132:425–427.
7. Ciardella AP, Klancnik J, Schiff W, et al. Intravitreal triamcinolone for the treatment of refractory diabetic macular oedema with hard exudates: an optical coherence tomography study. Br J Ophthalmol. 2004. 88:1131–1136.
8. Kang SW, Sa HS, Cho HY, Kim JI. Macular grid photocoagulation after intravitreal triamcinolone acetonide for diffuse diabetic macular edema. Arch Ophthalmol. 2006. 124:653–658.
9. Lam DS, Chan CK, Mohamed S, et al. Intravitreal triamcinolone plus sequential grid laser versus triamcinolone or laser alone for treating diabetic macular edema: six-month outcomes. Ophthalmology. 2007. 114:2162–2167.
10. Diabetic Retinopathy Clinical Research Network. Elman MJ, Aiello LP, et al. Randomized trial evaluating ranibizumab plus prompt or deferred laser or triamcinolone plus prompt laser for diabetic macular edema. Ophthalmology. 2010. 117:1064–1077.e35.
11. Gillies MC, McAllister IL, Zhu M, et al. Intravitreal triamcinolone prior to laser treatment of diabetic macular edema: 24-month results of a randomized controlled trial. Ophthalmology. 2011. 118:866–872.
12. Kang SW, Park SC, Cho HY, Kang JH. Triple therapy of vitrectomy, intravitreal triamcinolone, and macular laser photocoagulation for intractable diabetic macular edema. Am J Ophthalmol. 2007. 144:878–885.
13. Estabrook EJ, Madhusudhana KC, Hannan SR, Newsom RS. Can optical coherence tomography predict the outcome of laser photocoagulation for diabetic macular edema? Ophthalmic Surg Lasers Imaging. 2007. 38:478–483.
14. Gillies MC, Islam FM, Larsson J, et al. Triamcinolone-induced cataract in eyes with diabetic macular oedema: 3-year prospective data from a randomized clinical trial. Clin Experiment Ophthalmol. 2010. 38:605–612.
15. Arevalo JF, Sanchez JG, Wu L, et al. Primary intravitreal bevacizumab for diffuse diabetic macular edema: the Pan-American Collaborative Retina Study Group at 24 months. Ophthalmology. 2009. 116:1488–1497. 1497.e1
16. Nagasawa T, Naito T, Matsushita S, et al. Efficacy of intravitreal bevacizumab (Avastin) for short-term treatment of diabetic macular edema. J Med Invest. 2009. 56:111–115.
17. Querques G, Bux AV, Martinelli D, et al. Short-term fluctuation of diabetic macular edema after intravitreal ranibizumab injection. Retina. 2009. 29:1274–1281.
18. Papadopoulou DN, Mendrinos E, Mangioris G, et al. Intravitreal ranibizumab may induce retinal arteriolar vasoconstriction in patients with neovascular age-related macular degeneration. Ophthalmology. 2009. 116:1755–1761.
19. Von Hanno T, Kinge B, Fossen K. Retinal artery occlusion following intravitreal anti-VEGF therapy. Acta Ophthalmol. 2010. 88:263–266.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download