Abstract
Purpose
Residual head tilt has been reported in patients with superior oblique muscle palsy (SOP) after surgery to weaken the inferior oblique (IO) muscle. The treatments for these patients have not received appropriate attention. In this study, we evaluated the superior rectus (SR) muscle recession as a surgical treatment.
Methods
The medical records of 12 patients with SOP were retrospectively reviewed. Each of these patients had unilateral SR muscle recession for residual head tilt after IO muscle weakening due to SOP. The residual torticollis was classified into three groups on the basis of severity: mild, moderate, or severe. Both IO muscle overaction and vertical deviation, features of SOP, were evaluated in all patients. The severity of the preoperative and postoperative torticollis and vertical deviation were compared using a paired t-test and Fisher's exact test.
Results
The torticollis improved in nine of 12 (75%) patients after SR muscle recession. The difference between the preoperative and postoperative severity of torticollis was statistically significant (p = 0.0008). After surgery, the mean vertical deviation was significantly reduced from 12.4 prism diopters to 1.3 prism diopters (p = 0.0003).
Superior oblique muscle palsy (SOP) is the most common cause of ocular torticollis. Although vertical deviation and abnormal head posture are the characteristic features of SOP, surgical correction is necessary to reduce the head tilt and resolve the diplopia [1-4]. Surgical weakening of the inferior oblique (IO) muscle is the most widely performed corrective procedure for SOP [1]. Previous studies on IO muscle weakening due to SOP have reported successful outcomes with respect to head tilt and associated vertical deviation [2-4]. However, the previous studies also report the persistence of residual torticollis after strabismus surgery for head tilt [5,6]. Lau et al. [6] reported that a substantial number of patients, approximately 30%, had significant residual torticollis after strabismus surgery for SOP. Davis et al. [5] reported residual symptomatic SOP in 37 patients after the first operation. However, procedures to correct the residual torticollis have not been fully studied or discussed. In this study, we investigated the effect of superior rectus (SR) muscle recession on residual torticollis. We discussed the efficacy of SR muscle recession with regard not only to the postoperative vertical deviation and head tilt, but also to its technical advantages over other procedures.
This study involved a retrospective chart review of 117 consecutive patients who underwent IO muscle weakening procedure as the primary surgical treatment for SOP at Seoul National University Children's Hospital between January 2004 and May 2010. A single surgeon (SJK) performed all of the surgeries. A diagnosis of SOP was made on the basis of the following observations: incomitant hypertropia, a positive head-tilt test, and evidence of superior oblique (SO) muscle underaction or IO muscle overaction. Since the residual head tilt of these patients had not improved for greater than six months after the initial IO muscle surgery, they then underwent surgery to correct the residual head tilt.
If vertical deviation was noted in the entire upper gaze and the ipsilateral gaze, SR muscle recession in the hypertropic eye in primary gaze was selected as the surgical method to correct the residual head tilt. The amount of SR muscle recession was determined from the degree of vertical deviation in the primary position. The recession was performed as planned when the forced duction and exaggerated traction tests conducted during surgery showed no restriction of the SR or IO muscle. After surgery, all patients were followed-up for at least three months and often for longer.
The preoperative and postoperative examinations included evaluation of the torticollis as well as the horizontal and vertical deviations at both distance and far vision. The residual IO muscle overaction was also evaluated and graded from 0 to 4. The degree of torticollis was determined using two methods. First, the degree of torticollis in primary gaze was visually rated as mild, moderate, or severe by one clinician (SJK). Secondly, a neck and face photograph of primary gaze was taken, and the angle between the vertical midlines of the head and neck was measured. Residual torticollis in patients was classified into the following three groups on the basis of the above measured angle: mild torticollis (equal to or less than 5°), moderate torticollis (6°-10°), and severe torticollis (>10°). In all patients, the evaluations of torticollis were consistent between the two methods, clinician estimation and measurement of angle in a photograph.
Both the horizontal and vertical deviations were determined using the alternative cover test at a distance of 33 cm and 6 m in the primary and the cardinal gaze positions, respectively. The deviations were also assessed by examination in the right and the left head-tilted positions. However, in one patient younger than two years of age, the Krimsky method was used. In addition, the Bielschowsky head-tilt test and indirect ophthalmoscopy of both eyes were conducted preoperatively to detect the presence of torsional abnormalities, which were also confirmed by fundus photography as previously described [7]. Preoperative patient facial photographs were taken in the primary gaze position. Two ophthalmologists evaluated these photographs to detect any facial asymmetry. Orthopedic surgeons also examined the patients to determine any orthopedic problems.
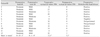
A residual head tilt was noted in 14 of the 117 (12%) patients who had IO muscle weakening due to SOP. Among these 14 patients, 12, including ten with congenital SOP and two with traumatic SOP, underwent unilateral SR muscle recession for residual head tilt. The demographics and clinical characteristics are summarized in Table 1.
As mentioned above, all patients in this study had previously undergone IO muscle weakening surgery for SOP (Table 1). Facial asymmetry was noted in six patients. An orthopedic surgeon fellow diagnosed asymmetry of the cervical paravertebral muscles in one patient. However, this asymmetry was insignificant and did not require treatment.
Before the SR muscle recession, the mean vertical deviation was 12.4 prism diopters (PD). Bielschowsly's head tilt test was positive in 90% of the patients. When the head was tilted toward the hypertropic eye, the mean vertical deviation was 21.6 PD. When the head was tilted in the opposite direction, the mean vertical deviation was 3.7 PD. Prior to SR muscle recession, the mean degree of IO muscle overaction was +0.7 (range, 0 to +2). No extorsion was noted in any hypertropic eye, as confirmed by fundus photography (Table 2).
All superior rectus muscle recessions were performed with no problems. During the surgery, a forced duction test was performed, and no restriction of any rectus muscle was noted. In addition, no IO muscle restriction was noted in the exaggerated traction test.
Table 3 lists the main outcomes of the SR surgery. Before the surgery, 91.7% of the patients (11 of 12) had a moderate degree of torticollis, while one patient (8.3%) had severe torticollis. After the surgery, a moderate degree of residual head tilt was noted in four (33%) patients, and no patient had severe torticollis. The torticollis improved in 75% of the patients, whereas no improvement was observed in the others. There was a significant difference between the preoperative and postoperative degrees of torticollis (p = 0.0008). In addition, the rectus muscle surgery significantly improved the mean vertical deviation from 12.4 PD to 1.3 PD (p = 0.0001).
Based on the results of this study, we suggest that SR muscle recession is an effective method to correct residual head tilt and vertical deviation after IO muscle weakening surgery in patients with SOP. Several studies have not only classified SOP, but also have reported surgical options [8-10]. However, only few studies have reported an appropriate treatment for residual head tilt after IO muscle weakening surgery for SOP [5]. A previous study reported that an additional IO muscle or superior oblique muscle surgery for residual head tilt provided symptomatic relief to 76% of the patients [5]. Our study reported a success rate of 75% after SR muscle recession, comparable to that reported by the previous study. SR muscle recession might be as effective as oblique muscle surgery for the treatment of residual head tilt after surgery for SOP. However, an additional IO muscle surgery might be technically complicated because of possible adhesions resulting from the first operation. Since these adhesions could be aggravated by re-operation, superior rectus muscle recession is more favorable for the treatment of residual head tilt.
In addition, the mean degree of IO muscle overaction was small (+0.7), while the mean vertical deviation was considerable (12.4 PD). Moreover, the exaggerated traction test for the operated eyes did not reveal either residual fibers or postoperative IO adhesions. Therefore, IO muscle surgery was not considered a favorable option for the patients of our study. Although Harada-Ito, a type of SO surgery, and its modified procedure have been considered effective for the treatment of excyclotorsion [11,12], no extorsion was detected in any hypertropic eye before the operation in our study, and thus, these two procedures were deemed unnecessary.
Our observation that SR muscle surgery can simultaneously reduce head tilt and vertical deviation should be investigated further with respect to the relationship between the SR muscle and SOP. From this viewpoint, Molinari and Ugrin [13] has recently reported SR muscle overaction/contracture syndrome in patients with SOP. According to their report, this syndrome was observed in 16.6% of all patients with unilateral SOP. A positive Bielschowsky head-tilt test is considered the most relevant sign of this syndrome [13], and Jampolsky [14] suggested recession of the involved superior rectus muscle for the treatment. In our study, a positive Bielschowsky head-tilt test was exhibited by 90% of the patients. Therefore, a possible combined SR muscle overaction/contracture syndrome can explain the successful surgical outcome of the SR muscle correction in our study. However, the forced duction test during surgery revealed no definite finding on the SR muscle. Nevertheless, the possibility of mild SR overaction/contracture, which were undetectable in the forced duction test, cannot be excluded. Further studies with a greater number of patients are required to evaluate the association of SR muscle overaction/contracture with residual head tilt after the IO muscle weakening procedure for SOP.
It has been widely accepted that head tilt in patients with SOP is a compensatory response to reduce vertical deviation. Therefore, if SR muscle recession can successfully reduce vertical deviation in patients with SOP, then the degree of torticollis may also decrease owing to a decrease in the compensatory response of head tilt. However, further investigation regarding other mechanisms that cause torticollis in patients with SOP is required in order to explain why three of our patients with no postoperative vertical deviation had a moderate degree of torticollis. Certain etiologies for torticollis were considered among our patients. One of the three patients had an orthopedic problem, cervical muscle asymmetry. Other causes of residual torticollis need to be explored further to explain the occurrence in the other two patients.
SR muscle recession may cause complications such as an elevation deficiency in the operated eye. In our study, the elevated deficiency was detected in only two patients, both of whom had a preoperative vertical deviation of 20 PD. It is possible that the larger amount of recession required in these patients compared to other cases may have caused the complication. However, the limitation on supraduction of the operated eye was insignificant in the two patients. After IO muscle weakening in patients with SOP, we believe that the efficacy of SR muscle recession for residual head tilt outweighs this complication.
Another surgical option, recession of the contralateral inferior rectus muscle to correct the vertical deviation and the compensatory head tilt, is a possibility. Knapp recommended this procedure for the treatment of SOP with large vertical deviation [10]. In addition, this method is preferred when there is no elevation deficiency in the operated eye. However, it was reported that the procedure can be complicated with operated eye lower lid retraction, which causes cosmetic problems and lagophthalmos with corneal exposure [15,16]. We believed that these complications may have been intolerable for the young patients in our study. Therefore, we preferred ipsilateral SR muscle recession.
In conclusion, we recommend that SR muscle recession be performed for the residual head tilt occurring after IO muscle weakening surgery for SOP. This procedure may be particularly preferred to an additional IO surgery if the vertical deviation is significant. However, little or no restriction or overaction of the IO muscle was noted in the present study.
Figures and Tables
Table 3
Head tilt and vertical deviation before and after the operation
PD = prism diopters.
*The operated eye became hypotropic after the recession; †Represented as mild : moderate : severe; ‡There was a significant difference between preoperative and postoperative severity of torticollis (p = 0.0008 by Fisher's exact test) and also between the mean preoperative and postoperative vertical deviation (p = 0.0001 by paired t-test).
References
1. Helveston EM, Mora JS, Lipsky SN, et al. Surgical treatment of superior oblique palsy. Trans Am Ophthalmol Soc. 1996. 94:315–328.
2. Simons BD, Saunders TG, Siatkowski RM, et al. Outcome of surgical management of superior oblique palsy: a study of 123 cases. Binocul Vis Strabismus Q. 1998. 13:273–282.
3. Toosi SH, von Noorden GK. Effect of isolated inferior oblique muscle myectomy in the management of superior oblique muscle palsy. Am J Ophthalmol. 1979. 88(3 Pt 2):602–608.
4. Von Noorden GK, Murray E, Wong SY. Superior oblique paralysis. A review of 270 cases. Arch Ophthalmol. 1986. 104:1771–1776.
5. Davis AR, Dawson E, Lee JP. Residual symptomatic superior oblique palsy. Strabismus. 2007. 15:69–77.
6. Lau FH, Fan DS, Sun KK, et al. Residual torticollis in patients after strabismus surgery for congenital superior oblique palsy. Br J Ophthalmol. 2009. 93:1616–1619.
7. Madigan WP Jr, Katz NN. Ocular torsion-direct measurement with indirect ophthalmoscope and protractor. J Pediatr Ophthalmol Strabismus. 1992. 29:171–174.
8. Graf M. Diagnosis and treatment of trochlear nerve palsy. Klin Monbl Augenheilkd. 2009. 226:806–811.
9. Knapp P. First annual Richard G. Scobee memorial lecture. Diagnosis and surgical treatment of hypertropia. Am Orthopt J. 1971. 21:29–37.
10. Knapp P, Moore S. Diagnosis and surgical options in superior oblique surgery. Int Ophthalmol Clin. 1976. 16:137–149.
11. Nishimura JK, Rosenbaum AL. The long-term torsion effect of the adjustable Harada-Ito procedure. J AAPOS. 2002. 6:141–144.
12. Ameri A, Anvari F, Jafari AK, et al. Intraoperative adjustable suture surgery for excyclotorsion: a modification of the harada-ito procedure. J Pediatr Ophthalmol Strabismus. 2009. 46:368–371.
13. Molinari A, Ugrin MC. Frequency of the superior rectus muscle overaction/contracture syndrome in unilateral fourth nerve palsy. J AAPOS. 2009. 13:571–574.
14. Jampolsky A. Superior rectus overaction/contracture syndrome. 1998. Buenos Aires: Ciba Vision, Novartis;193–206.
15. Pacheco EM, Guyton DL, Repka MX. Changes in eyelid position accompanying vertical rectus muscle surgery and prevention of lower lid retraction with adjustable surgery. J Pediatr Ophthalmol Strabismus. 1992. 29:265–272.
16. Kushner BJ. A surgical procedure to minimize lower-eyelid retraction with inferior rectus recession. Arch Ophthalmol. 1992. 110:1011–1014.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download