Abstract
Purpose
To evaluate the changes in anterior chamber depth (ACD) and angle width induced by phacoemulsification and intraocular lens (IOL) implantation in normal eyes using anterior segment optical coherence tomography (AS-OCT).
Methods
Forty-five eyes (45 patients) underwent AS-OCT imaging to evaluate anterior chamber configuration before and 2 days after phacoemulsification and IOL implantation. We analyzed the central ACD and angle width using different methods: anterior chamber angle (ACA), trabecular-iris angle (TIA), angle opening distance (AOD), and trabecular iris surface area (TISA) in the nasal and temporal quadrants. Comparison between preoperative and postoperative measurement was done using paired t-tests and each of the angle parameters was analyzed with Pearson correlation testing. Subgroup analyses according to the IOL and axial length were performed with a general multivariate linear model adjusted for age.
Results
Before surgery, the mean anterior chamber angle widths were 23.21 ± 6.70° in the nasal quadrant and 24.89 ± 7.66° in the temporal quadrant. The mean central ACD was 2.75 ± 0.43 mm. After phacoemulsification and IOL implantation, the anterior chamber angle width increased significantly to 35.16 ± 4.65° in the nasal quadrant (p = 0.001) and 36.03 ± 4.86° in the temporal quadrant (p = 0.001). Also, central ACD increased to 4.14 ± 0.31 mm (p = 0.001). AOD, TISA, and TIA increased significantly after cataract surgery and showed positive correlation with ACA.
Anterior segment cross-sectional imaging is essential in evaluating the anterior chamber configuration with quantitative data. Several methods have been studied and used for the diagnosis of glaucoma or other anterior segment pathology and quantification of angle configuration [1-11]. Ultrasound biomicroscopy (UBM) provides high-resolution images of the anterior chamber and is able to penetrate opaque media. With UBM, detailed images of the iridotrabecular angle and ciliary body can be obtained; these structures are not visible with a gonioscope [12-14]. However, the UBM transducer requires the eye to be immersed in a water bath of saline with the patient supine; the procedure is uncomfortable for the patient and requires a skilled examiner. Scheimpflug photography is a non-invasive and repeatable technique that uses a slit beam and a camera. However, because of its optical and acoustic characteristics, images must undergo processing and do not allow visualization of the actual angle recess [9,11,14].
Recently, anterior segment optical coherence tomography (AS-OCT) has emerged as a new imaging technique for the anterior segment that is non-invasive and non-contact. AS-OCT provides high resolution images by using a long wavelength (1,310 nm) of light; it offers rapid and easy quantitative analysis of various structures [12,15-17]. AS-OCT has exhibited good repeatability and reproducibility with low intraobserver and interobserver variability [18-21]. One limitation of AS-OCT is that it has incomplete penetration through the pigmented epithelium of the iris, thus making it difficult to obtain accurate images of the ciliary body, lens, and zonules behind the pigmented iris [17].
Cataract extraction with intraocular lens (IOL) implantation causes the anterior chamber angle to widen and the depth to deepen in glaucomatous and normal eyes [2,3,5,22-26]. Previous studies have used several methods to evaluate the changes before and after cataract surgery.
The object of this study was to analyze changes in the anterior chamber depth and angle width after phacoemulsification and IOL implantation in normal eyes using AS-OCT. We obtained quantitative data from normal Korean eyes as measured by AS-OCT and compared standardized parameters of anterior chamber configuration.
This prospective study comprised 45 eyes from 45 consecutive patients with cataract who underwent cataract surgery from February 2008 to November 2008. Patients with glaucoma, previous intraocular surgery, or other intraocular pathology were excluded.
All patients underwent routine ophthalmic examinations including visual acuity, Goldmann tonometry, slit-lamp biomicroscopy, and funduscopy. Refractive errors were measured as manifest refraction. Axial lengths were obtained using a Humphrey 820 model A-scan ultrasound unit (Humphrey Systems, Dublin, CA, USA). AS-OCT (Visante; Carl Zeiss Meditec, Dublin, CA, USA) was performed preoperatively and 2 days postoperatively. One examiner obtained all images under identical lighting conditions. For measurement, the pupil was not dilated and the patient was asked to sit and fixate on an indicator in the AS-OCT. Images of the nasal and temporal angle quadrants (0° and 180° meridians) were captured until the centration and quality were sufficient for analyzation.
The same surgeon (PKH) performed all phacoemulsification and IOL implantation under topical anesthesia. Phacoemulsification and foldable IOL implantation were performed through a 2.75 mm temporal clear corneal incision. The corneal incision was not sutured. Nine eyes received an SA60AT (Acrysof; Alcon, Fort Worth, TX, USA) IOL, 14 eyes received a Biovue (OII, Ontario, CA, USA) IOL, and 22 eyes received an IQ (Acrysof) IOL.
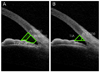
The best image was selected and analyzed using custom software (Iridocorneal Module; Carl Zeiss Meditec). The anterior chamber angle was calculated using two different definitions: 1) anterior chamber angle (ACA) - the angle between the iris tangential line and that of the posterior corneal surface with its apex in the angle recess (Fig. 1); and 2) trabecular-iris angle (TIA) - the angle between the arms passing through a point on the trabecular meshwork 500 µm from the scleral spur and a point perpendicularly opposite on the iris (Fig. 2) [7]. ACA width was also analyzed with standardized angle parameters after manual identification of the scleral spur: 1) angle opening distance (AOD) at 500 µm (AOD500) and AOD at 750 µm (AOD750) - distance of a perpendicular from the trabecular meshwork on the iris at a point 500 µm or 750 µm from the scleral spur; and 2) trabecular iris space area (TISA) up to 500 µm (TISA500) or 750 µm (TISA750) - the area bounded by the corneal endothelium, trabecular meshwork, and anterior iris surface out to a distance of 500 µm or 750 µm from the scleral spur (Fig. 2). ACD was defined as the distance from the endothelium at the center of the cornea to the anterior pole of the lens or IOL (Fig. 1).
Patients were divided into 3 groups according to the axial length of the globe: group 1 (axial length <23 mm); group 2 (axial length 23 to 26 mm); and group 3 (axial length >26 mm).
All statistical analyses were performed using SPSS ver. 12 (SPSS Inc., Chicago, IL, USA). Comparison between preoperative and postoperative angle parameters and ACD was done using a paired t-test. Analysis of each angle parameter was performed using Pearson correlation testing. Comparison according to the axial length and IOL type were performed using a general multivariate linear model adjusted for age. All p-values were 2-sided and were considered statistically significant when <0.05.
Of the 45 patients, 16 were men and 29 were women. The mean age was 67.8 ± 9.7 years (range, 32 to 83 years). All patients were diagnosed with senile cataract except for two middle-aged patients who had used corticosteroids for systemic diseases.
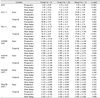
The mean preoperative ACD was 2.75 ± 0.43 mm. The mean postoperative ACD was 4.14 ± 0.31 mm at 2 days after cataract surgery, approximately 50.5% deeper than before surgery (p < 0.001). Changes in ACD and preoperative ACD showed a negative correlation (r = -0.680, p < 0.01) (Fig. 3).
All angle parameters analyzed with AS-OCT showed a significant increase after cataract surgery for both the nasal and temporal angles. The mean preoperative ACA was 23.21 ± 6.70° at the nasal angle and 24.89 ± 7.66° at the temporal angle. After cataract surgery, ACA increased to 35.16 ± 4.65° at the nasal angle and 36.03 ± 4.86° at the temporal angle, widening to 51.5% and 44.8%, respectively. An increase in ACA exhibited a significant negative correlation with preoperative ACA at both the nasal and temporal angles (r = -0.723, p < 0.01 at the nasal angle; r = -0.777, p < 0.01 at the temporal angle) (Fig. 3).
The mean preoperative TIA was 32.42 ± 12.64° at the nasal angle and 34.05 ± 14.68° at the temporal angle. Postoperatively, the TIA increased to 50.20 ± 7.66° at the nasal angle and 52.26 ± 8.38° at the temporal angle, widening 56.2% and 52.2%, respectively.
Standardized angle parameters were also significantly increased. Preoperative AOD500 was 0.341 ± 0.165 mm at the nasal quadrant and 0.370 ± 0.207 mm at the temporal quadrant. Postoperative mean AOD500 was 0.618 ± 0.153 mm at the nasal angle and 0.675 ± 0.204 mm at the temporal angle. AOD750 also increased from 0.477 ± 0.217 mm to 0.869 ± 0.180 mm at the nasal angle and from 0.544 ± 0.290 mm to 0.937 ± 0.264 mm at the temporal angle following cataract surgery. TISA500 at the nasal angle increased from 0.130 ± 0.057 mm2 to 0.228 ± 0.061 mm2 and TISA500 at the temporal angle increased from 0.141 ± 0.067 mm2 to 0.243 ± 0.073 mm2. TISA750 also increased from 0.231 ± 0.101 mm2 to 0.413 ± 0.098 mm2 at the nasal angle and from 0.257 ± 0.127 mm2 to 0.447 ± 0.131 mm2 at the temporal angle (Table 1).
This study demonstrated a statistically significant positive correlation between ACA and standardized angle parameters (TIA, AOD, and TISA) in the nasal and temporal quadrants (Table 2).
The changes in ACD and angle variables were not statistically different according to the type of implanted IOL when adjusted for age and axial length.
Patients were divided into three groups according to axial length. The mean axial length was 24.26 ± 2.15 mm (range, 21.77 to 31.90). The mean axial length for each group was 22.31 ± 0.33 mm in group 1 (n = 8), 24.00 ± 0.94 mm in group 2 (n = 32), and 29.32 ± 1.88 mm in group 3 (n = 5). Table 3 shows the subgroup analyses performed according to axial length. Patients with a short axial length (group 1) exhibited a shallow ACD and a narrow ACA both preoperatively and postoperatively. All other angle parameters were also smaller in group 1 before surgery. However, postoperative values were not significantly different between the groups, except for AOD750 at the temporal angle (p = 0.035). The mean changes after surgery between the groups were significantly different for ACA and TISA750 at the temporal angle and for TIA and AOD750 at both angles. Other values also showed a trend toward larger changes in group 1. This analysis was adjusted for age using a general linear model.
AS-OCT is a light-based system that rapidly provides high-resolution images. Its non-contact nature ensures patient comfort and allows for rapid image acquisition in the sitting position, without risk of mechanical distortion of the angle. It also allows quantitative and dynamic data analysis with high reproducibility and repeatability [2,3,12,14,16,18-23,27-30]. This study demonstrates changes in anterior segment configuration after phacoemulsification and IOL implantation in normal eyes as measured quantitatively by AS-OCT. We provided normative data of anterior segment parameters in normal eyes and also compared these parameters with each other.
This study confirmed angle widening of up to 51.5% (at the nasal angle) and chamber deepening of up to 50.5% after cataract surgery, as other studies have previously demonstrated [3,22,23,25,27]. Our data also revealed a negative correlation between preoperative ACD and the amount of increase of ACD and between preoperative angle parameters and the changes of these angle parameters following cataract surgery.
The mean preoperative ACD was 2.75 ± 0.43 mm and the mean preoperative ACA was 23.21 ± 6.70° at the nasal angle and 24.89 ± 7.66° at the temporal angle. These results are similar to results from other studies which have analyzed changes in ACD and ACA following cataract surgery [3]. Yi et al. [31] gathered ACD and ACA data in a normal Korean population without cataract. They included 81 healthy volunteers with a mean age of 22.3 ± 3.5 years (range, 18 to 33 years). The ACA in the nasal and temporal quadrants was 45.13 ± 5.89° and 46.18 ± 5.50° in the right eyes and 44.90 ± 5.94° and 46.67 ± 5.98° in the left eyes, respectively. The mean ACD was 3.32 ± 0.26 mm in the right eyes and 3.31 ± 0.28 mm in the left eyes [31]. These results were larger than our results. The patients in our study were considered to represent the normal population without intraocular abnormalities. However, the patients enrolled in this study were primarily elderly patients with cataractous lenses; the mean age of the patients was 67.8 ± 9.7 years (range, 32 to 83 years). Lens thickness increases with age and the anterior lens surface migrates toward the cornea [32]. Furthermore, many cataractous lenses are greater in volume and thickness compared to normal lenses [33]. As such, we believe this accounts for why the ACD and ACA in eyes with cataractous lenses in this study were smaller than those with normal lenses.
Two different methods were used in this study to measure the anterior chamber angle width. The first method, ACA, is simple and unrelated to scleral spur localization. However, due to the iris configuration it is sometimes difficult to determine the angle recession and to draw a tangential line to the iris surface. The other method, TIA, is regarded as a standardized parameter for measuring the trabecular meshwork opening. However, to obtain an exact value it is essential to localize the appropriate scleral spur. ACA and TIA are inherently different parameters, but they demonstrate a high association (r = 0.845, p < 0.01 at the nasal quadrant; r = 0.912, p < 0.01 at the temporal quadrant). The other parameters which measure the anterior chamber angle are AOD500 and AOD750. Localization of the scleral spur is essential for these parameters and manipulation of the scale bar increases the frequency of errors.
We obtained data for these different angle parameters and compared them amongst each other. All of the angle parameters showed a high degree of correlation (Table 2); we confirmed that these different angle parameters are highly associated with each other. Furthermore, it is not possible to determine which parameter is superior. Quantitative measurement of the angle is difficult due to its non-linear, 3-dimensional, dynamic configuration. Standardized angle parameters were defined artificially to allow quantitative measurement and to compare the angle configurations. As such, each parameter possesses merits and faults. Many studies have explored different methods for quantifying angle measurements. Definitions of the angle are only used to quantitatively measure the angle, so it is not necessary to determine superior methods of angle standardization. Our results confirmed that all of the methods we measured in this study showed a high correlation with each other, which suggests that results from studies using different angle measurement techniques likely have similar meanings.
Nasal and temporal angle parameters showed no statistically significant differences (data not shown). Some studies have shown that the temporal ACA was significantly larger than the nasal ACA as measured by AS-OCT and pentacam [3,31]. However, our data demonstrate that the temporal and nasal angle width and the amount of change were similar.
In this study we used three different kinds of IOLs and analyzed the data according to IOL type. There was no statistically significant difference in the studied variables among the three types of IOLs when adjusted for age and axial length (data not shown). This is concurrent with previous studies [3,34]. This result may be related to the similar properties of the IOLs we used; all of the IOLs in this study were acrylic, single-piece IOLs with an optic diameter of 6.0 mm.
We performed subgroup analysis according to axial length to investigate a possible association with anterior chamber parameters. As expected and in line with a previous report [35], ACD and angle parameters were significantly smaller in group 1 (axial length <23 mm) preoperatively. ACD and ACA remained significantly different after cataract surgery between the groups; however, other angle parameters were not significantly different, with the exception of AOD750 at the temporal quadrant. Changes between groups were statistically significant for ACA and TISA750 at the temporal angle and for TIA and AOD 750 at both angles; however, the other values demonstrated a similar trend. A larger number of patients is necessary to confirm these findings.
In accordance with Pavlin et al. [36], ACD was defined as the distance from the posterior surface of the center of the cornea to the anterior surface of the lens or IOL. Definitions of ACD can vary according to the reference structures (angle, pupil, and lens). A previous study revealed that lens-referenced ACD was more practical and precise [3]. This parameter is limited in that it includes some portion of the posterior chamber when measured in eyes with an IOL. As such, in this study the deepening of the anterior chamber could have been exaggerated.
To the best of our knowledge, this study is the largest report in a Korean population regarding anterior chamber configuration in cataractous eyes using AS-OCT before and after cataract surgery. Widening of the anterior angle and deepening of the anterior chamber depth in normal eyes has been well established in previous studies [3,23,25,27]. This study provides data on a relatively large number of patients regarding the comparison of many parameters used to quantitatively analyze anterior segment configuration; these parameters were found to be highly correlated with each other. Axial length is an important factor in anterior chamber measurements; it is associated not only with preoperative anterior chamber parameters, but also with changes in certain parameters such as TIA and AOD750.
Figures and Tables
 | Fig. 1Anterior segment optical coherence tomography image of the right eye of a 50-year-old woman before (A) and after (B) cataract surgery. Anterior chamber depth (ACD) was defined as the distance from the endothelium at the center of the cornea to the anterior pole of the lens or intraocular lens. ACA = anterior chamber angle. |
 | Fig. 2(A) The angle-opening distance (AOD) at 500 µm anterior to the scleral spur (AOD500) and the AOD at 750 µm anterior to the scleral spur (AOD750) were defined as the distance from the corneal endothelium to the anterior iris perpendicular to a line drawn along the trabecular meshwork at 500 µm or 750 µm from the scleral spur. The trabecular-iris space areas (TISA) at 500 µm or 750 µm from the scleral spur (TISA500, TISA750) were defined as the areas bounded by the corneal endothelium, trabecular meshwork, and anterior iris surface out to a distance of 500 µm or 750 µm from the scleral spur. (B) The trabecular-iris angle (TIA), defined as the angle measured with the apex in the scleral spur and the arms of the angle passing through a point on the trabecular meshwork 500 µm from the scleral spur and a perpendicular point on the iris. |
 | Fig. 3(A,B) Preoperative anterior chamber angle (ACA) measurements and changes in the angle following cataract surgery showed negative correlations in the nasal (A) and temporal (B) quadrants. (C) Preoperative anterior chamber depth (ACD) and postoperative changes in ACD also showed a negative correlation. |
References
1. Boker T, Sheqem J, Rauwolf M, Wegener A. Anterior chamber angle biometry: a comparison of Scheimpflug photography and ultrasound biomicroscopy. Ophthalmic Res. 1995. 27:Suppl 1. 104–109.
2. Dada T, Sihota R, Gadia R, et al. Comparison of anterior segment optical coherence tomography and ultrasound biomicroscopy for assessment of the anterior segment. J Cataract Refract Surg. 2007. 33:837–840.
3. Kucumen RB, Yenerel NM, Gorgun E, et al. Anterior segment optical coherence tomography measurement of anterior chamber depth and angle changes after phacoemulsification and intraocular lens implantation. J Cataract Refract Surg. 2008. 34:1694–1698.
4. Lam AK, Chan R, Woo GC, et al. Intra-observer and inter-observer repeatability of anterior eye segment analysis system (EAS-1000) in anterior chamber configuration. Ophthalmic Physiol Opt. 2002. 22:552–559.
5. Memarzadeh F, Tang M, Li Y, et al. Optical coherence tomography assessment of angle anatomy changes after cataract surgery. Am J Ophthalmol. 2007. 144:464–465.
6. Pavlin CJ, Foster FS. Plateau iris syndrome: changes in angle opening associated with dark, light, and pilocarpine administration. Am J Ophthalmol. 1999. 128:288–291.
7. Pavlin CJ, Ritch R, Foster FS. Ultrasound biomicroscopy in plateau iris syndrome. Am J Ophthalmol. 1992. 113:390–395.
8. Pavlin CJ, Sherar MD, Foster FS. Subsurface ultrasound microscopic imaging of the intact eye. Ophthalmology. 1990. 97:244–250.
9. Richards DW, Russell SR, Anderson DR. A method for improved biometry of the anterior chamber with a Scheimpflug technique. Invest Ophthalmol Vis Sci. 1988. 29:1826–1835.
10. Sakuma T, Sawada A, Yamamoto T, Kitazawa Y. Appositional angle closure in eyes with narrow angles: an ultrasound biomicroscopic study. J Glaucoma. 1997. 6:165–169.
11. Shibata T, Sasaki K, Sakamoto Y, Takahashi N. Quantitative chamber angle measurement utilizing image-processing techniques. Ophthalmic Res. 1990. 22:Suppl 1. 81–84.
12. Nolan W. Anterior segment imaging: ultrasound biomicroscopy and anterior segment optical coherence tomography. Curr Opin Ophthalmol. 2008. 19:115–121.
13. Radhakrishnan S, Goldsmith J, Huang D, et al. Comparison of optical coherence tomography and ultrasound biomicroscopy for detection of narrow anterior chamber angles. Arch Ophthalmol. 2005. 123:1053–1059.
14. Radhakrishnan S, Huang D, Smith SD. Optical coherence tomography imaging of the anterior chamber angle. Ophthalmol Clin North Am. 2005. 18:375–381.
15. Nolan W. Anterior segment imaging: identifying the landmarks. Br J Ophthalmol. 2008. 92:1575–1576.
16. Radhakrishnan S, Rollins AM, Roth JE, et al. Real-time optical coherence tomography of the anterior segment at 1310 nm. Arch Ophthalmol. 2001. 119:1179–1185.
17. Lee R, Ahmed II. Anterior segment optical coherence tomography: non-contact high resolution imaging of the anterior chamber. Tech Ophthalmol. 2006. 4:120–127.
18. Li H, Leung CK, Cheung CY, et al. Repeatability and reproducibility of anterior chamber angle measurement with anterior segment optical coherence tomography. Br J Ophthalmol. 2007. 91:1490–1492.
19. Mohamed S, Lee GK, Rao SK, et al. Repeatability and reproducibility of pachymetric mapping with Visante anterior segment-optical coherence tomography. Invest Ophthalmol Vis Sci. 2007. 48:5499–5504.
20. Muller M, Dahmen G, Porksen E, et al. Anterior chamber angle measurement with optical coherence tomography: intraobserver and interobserver variability. J Cataract Refract Surg. 2006. 32:1803–1808.
21. Radhakrishnan S, See J, Smith SD, et al. Reproducibility of anterior chamber angle measurements obtained with anterior segment optical coherence tomography. Invest Ophthalmol Vis Sci. 2007. 48:3683–3688.
22. Hayashi K, Hayashi H, Nakao F, Hayashi F. Changes in anterior chamber angle width and depth after intraocular lens implantation in eyes with glaucoma. Ophthalmology. 2000. 107:698–703.
23. Nolan WP, See JL, Aung T, et al. Changes in angle configuration after phacoemulsification measured by anterior segment optical coherence tomography. J Glaucoma. 2008. 17:455–459.
24. Nonaka A, Kondo T, Kikuchi M, et al. Angle widening and alteration of ciliary process configuration after cataract surgery for primary angle closure. Ophthalmology. 2006. 113:437–441.
25. Pereira FA, Cronemberger S. Ultrasound biomicroscopic study of anterior segment changes after phacoemulsification and foldable intraocular lens implantation. Ophthalmology. 2003. 110:1799–1806.
26. Dawczynski J, Koenigsdoerffer E, Augsten R, Strobel J. Anterior segment optical coherence tomography for evaluation of changes in anterior chamber angle and depth after intraocular lens implantation in eyes with glaucoma. Eur J Ophthalmol. 2007. 17:363–367.
27. Chang DH, Lee SC, Jin KH. Changes of anterior chamber depth and angle after cataract surgery measured by anterior segment OCT. J Korean Ophthalmol Soc. 2008. 49:1443–1452.
28. Leung CK, Chan WM, Ko CY, et al. Visualization of anterior chamber angle dynamics using optical coherence tomography. Ophthalmology. 2005. 112:980–984.
29. Leung CK, Cheung CY, Li H, et al. Dynamic analysis of dark-light changes of the anterior chamber angle with anterior segment OCT. Invest Ophthalmol Vis Sci. 2007. 48:4116–4122.
30. Nemeth G, Vajas A, Tsorbatzoglou A, et al. Assessment and reproducibility of anterior chamber depth measurement with anterior segment optical coherence tomography compared with immersion ultrasonography. J Cataract Refract Surg. 2007. 33:443–447.
31. Yi JH, Lee H, Hong S, et al. Anterior chamber measurements by pentacam and AS-OCT in eyes with normal open angles. Korean J Ophthalmol. 2008. 22:242–245.
32. Dubbelman M, van der Heijde GL, Weeber HA. The thickness of the aging human lens obtained from corrected Scheimpflug images. Optom Vis Sci. 2001. 78:411–416.
33. Williams DL. Lens morphometry determined by B-mode ultrasonography of the normal and cataractous canine lens. Vet Ophthalmol. 2004. 7:91–95.
34. Kim JS, Shyn KH. Periodic biometry in three types of posteriorly implanted IOLs: PMMA, silicone, and acrylic soft, by EAS-1000 Scheimpflug photography. J Korean Ophthalmol Soc. 2000. 41:2205–2210.
35. Hosny M, Alio JL, Claramonte P, et al. Relationship between anterior chamber depth, refractive state, corneal diameter, and axial length. J Refract Surg. 2000. 16:336–340.
36. Pavlin CJ, Harasiewicz K, Foster FS. Ultrasound biomicroscopy of anterior segment structures in normal and glaucomatous eyes. Am J Ophthalmol. 1992. 113:381–389.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download