Abstract
A 79-year-old male presented with left ocular pain. Evisceration and silicone ball implantation were performed after a diagnosis of phthisis. He returned six weeks later because of left facial erythematous swelling, tenderness, mild fever, chills and cough. His condition was diagnosed as orbital cellulitis. Despite two weeks of empirical antibiotic therapy, the symptoms worsened. A subsequent orbital computed tomography scan revealed enhanced soft tissue infiltrations in his left orbit and eyelid. Biopsy showed a diffusely infiltrating tumor of signet ring cell cytology. A systemic evaluation revealed multiple bone metastases. Based on this evidence, the patient was diagnosed with a very rare case of histiocytoid variant eccrine sweat gland carcinoma with multiple bone metastases.
The histiocytoid variant of eccrine sweat gland carcinoma is very rare, although the histiocytoid variant of eccrine sweat gland carcinoma (specifically, infiltrating signet ring carcinoma) occurring in the eyelid has been reported [1-6]. The histiocytoid variant is a malignant tumor diffusely infiltrating the dermis and subcutaneous tissue without epidermal involvement. Here, we report the first Korean case of a histiocytoid variant of eccrine sweat gland carcinoma, showing infiltrations of signet ring cell cytology and multiple bone metastases. The symptoms were initially misdiagnosed as orbital cellulitis after surgery.
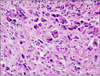
A 79-year-old male visited our clinic for the evaluation of left ocular pain that had recently worsened. His left eye was phthitic due to glaucoma. The patient had also previously undergone an endoscopic rectal polypectomy. Evisceration and silicone ball (18 mm) implantation were performed. He returned six weeks later with symptoms of mild fever, cough, and chills, as well as left facial erythema, swelling, and tenderness (Fig. 1). We diagnosed the symptoms as orbital cellulitis induced by recent evisceration surgery and the common cold. However, despite two weeks of empirical antibiotic therapy, the patient's symptoms worsened. An orbital computed tomography (CT) scan revealed enhanced soft tissue infiltrations in his left extraconal and intraconal spaces and a thickening of the left eyelid (Fig. 2). An incisional biopsy of the orbital tissue was performed through the superomedial portion of the conjunctiva. The tumor was gray-white colored and was not separated from the surrounding tissue on gross examination. Histopathology demonstrated cells with round to oblong nuclei, small distinct nucleoli, and relatively abundant granular amphophilic cytoplasm. Some cells had signet ring cytology, with a dominant cytoplasmic vacuole and an eccentrically placed, crescent-shaped nucleus (Fig. 3). Immunohistochemistry revealed that the tumor tissue was positive for cytokeratin and cytokeratin 7 but negative for cytokeratin 20.
Results of an abdominal ultrasound, abdominal-pelvic CT, and a whole body bone scan suggested no systemic involvement. Additionally, tumor marker tests were all within the normal ranges. However, brain magnetic resonance imaging and positron emission tomography revealed metastatic lesions on the left frontal and temporal lobes of the skull; nasal bone; left basal skull; right mandibular ramus and sternum; vertebra in the cervical, thoracic, lumbar and sacral regions; and the left ischium (Fig. 4). To rule out a secondary tumor from the previous rectal lesion, rectal biopsy was performed and revealed a benign adenoma confined to the mucosal layer. Consequently, the lesion in question was diagnosed as a primary malignant eccrine sweat gland carcinoma of the eye (a histiocytoid variant of eccrine sweat gland carcinoma) with multiple bone metastases. Although the patient was fully functional on the first visit, his general condition declined during the subsequent three months. The patient became bedridden, refused all recommended treatments, and received only conservative treatment.
Primary eccrine sweat gland carcinoma is a very rare tumor that most typically occurs in the eyelids of the elderly. There are three variants of this type of carcinoma: mucinous, adenoid cystic, and ductal [1-6]. The present case is of the third variant, ductal carcinoma. Ductal carcinomas are further classified into two categories based on the type of cell differentiation: well-differentiated ductal carcinoma featuring numerous signet ring cells are classified as signet ring carcinoma, while poorly-differentiated ductal carcinoma is classified as the histiocytoid variant. The tumor in question showed the characteristics of the latter form [1,2,4,7]. This histiocytoid variant of eccrine sweat gland carcinoma showed a histiocyte morphology rather than a signet ring cell morphology in the tumor burden, although histiocytoid tumors may contain foci of signet ring cell morphology, and vice versa [1,3]. Tumor cells in this case exhibited eosinophilic cytoplasm with intracytoplasmic vacuolations, characteristics similar to those of a histiocyte. The majority of tumor cells did not have the distinct, eccentric, scimitar-like nuclei of signet ring cells.
A primary histiocytoid variant of eccrine sweat gland carcinoma is a very rare neoplasm, with only eight cases having been reported in the literature [1,7]. In the cases reported, most tumor cells had abundant eosionophilic cytoplasm with intracytoplasmic vacuolations resembling histiocytes and a signet ring appearance [1,2,4,7,8]. The diagnosis of primary histiocytoid variant of eccrine sweat gland carcinoma is one of exclusion. Common primary foci include the breast, gastrointestinal tract, lung, skin, and urogenital tract. The most common sites are breast in women and lung in men [1,7,8]. Previously reported cases of the histiocytoid variant of eccrine sweat gland carcinoma follow an indolent course with slow and painless growth [1,2,7]. Only one of the eight cases showed metastasis, recurrence, and mortality [1]. However, these tumors can exhibit rapid growth with consequent pain. The case reported here had an unfavorable outcome with rapid progression, ocular pain, facial pain, and multiple bone metastases.
Most cases of primary eccrine sweat gland carcinoma described in the literature mainly appeared in the eyelid. However, Kramer et al. [3] described the eccrine sweat gland carcinoma in the orbit. Like Kramer et al. [3], the imaging studies in this case showed soft tissue infiltrations primarily involved in the orbit. Moreover, the subcutaneous infiltrations of the eyelid were also noted on the imaging studies. These facts suggested that the tumor mass in this case affected both the orbit and the eyelid.
The orbital imaging studies were not performed before the evisceration surgery because it was believed that the patient's accelerated ocular pain was induced by glaucoma. At his preoperative assessment, the patient's left eye was phthitic and appeared stable. After the evisceration surgery, the patient's facial pain and erythema were believed to be caused by orbital cellulitis. He had multiple risk factors for orbital infection: advanced age, recent evisceration surgery, silicone ball implantation, and symptoms of the common cold. In hindsight, the increased ocular pain could have been caused by the tumor growth occurring at the time of the evisceration surgery, rather than glaucoma. In other words, the ocular pain could have been cancer-related pain associated with the rapid tumor growth. It is difficult to determine the exact time of tumor occurrence because orbital imaging was not performed before the surgical procedure. We presumed that the patient's pre- and post-operative pain and orbital cellulitis may be related to the tumor growth. Furthermore, the rapid progression of the tumor may have been accelerated by the surgical procedure. As a result, the interval from the patient's initial visit with simple left ocular pain to the eventual diagnosis of primary eccrine sweat gland carcinoma was only three months. After the diagnosis, multiple metastases were also detected along the spine.
To our knowledge, this is the first Korean case of a histiocytoid variant of eccrine sweat gland carcinoma in the eye. Based on this case, we suggest taking an orbital imaging study prior to evisceration surgery in cases of abnormal ocular pain or rapid progression. In refractory cases of orbital cellulitis, aggressive follow-up may be necessary, including diagnostic confirmation through orbital imaging and tissue biopsy.
Figures and Tables
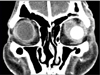 | Fig. 2Enhanced extraconal and intraconal infiltrations in the left orbit, and an inferolateral view of the silicone ball sphere in the eyelid. |
References
1. Mortensen AL, Heegaard S, Clemmensen O, Prause JU. Signet ring cell carcinoma of the eyelid - the monocle tumour. APMIS. 2008. 116:326–332.
2. Langel DJ, Yeatts RP, White WL. Primary signet ring cell carcinoma of the eyelid: report of a case demonstrating further analogy to lobular carcinoma of the breast with a literature review. Am J Dermatopathol. 2001. 23:444–449.
3. Kramer TR, Grossniklaus HE, McLean IW, et al. Histiocytoid variant of eccrine sweat gland carcinoma of the eyelid and orbit: report of five cases. Ophthalmology. 2002. 109:553–559.
4. Swinson B, Ryan F, Barrett AW, et al. Histiocytoid eccrine sweat gland carcinoma of the eyelid: report of a case. Clin Exp Dermatol. 2006. 31:786–789.
5. Hoppenreijs VP, Reuser TT, Mooy CM, et al. Syringomatous carcinoma of the eyelid and orbit: a clinical and histopathological challenge. Br J Ophthalmol. 1997. 81:668–672.
6. Krishnakumar S, Mohan ER, Babu K, et al. Eccrine duct carcinoma of the eyelid mimicking meibomian carcinoma: clinicopathological study of a case. Surv Ophthalmol. 2003. 48:439–446.
7. Jakobiec FA, Austin P, Iwamoto T, et al. Primary infiltrating signet ring carcinoma of the eyelids. Ophthalmology. 1983. 90:291–299.
8. Wollensak G, Witschel H, Böhm N. Signet ring cell carcinoma of the eccrine sweat glands in the eyelid. Ophthalmology. 1996. 103:1788–1793.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download