Abstract
This research focuses on four cases of patients having undergone eximer laser photorefractive surgery who were diagnosed with adenoviral keratoconjunctivitis during the postoperative period and who later developed epidemic keratoconjunctivitis (EKC)-like keratitis. Two of the patients had undergone laser-assisted subepithelial keratectomy (LASEK), one had undergone laser in situ keratomileusis and one had photorefractive keratectomy. After the surgery adenoviral keratoconjunctivitis and recurrent late-developing EKC-like keratitis were observed in the patients. Recurrent late-developing EKC-like keratitis occurred in one of the patients, who had received LASEK as many as three times. The others had only one or two episodes.The corneal infiltrates of keratitis mainly occurred in the central cornea. Successful resolution of recurrent late-developing EKC-like keratitis was achieved through the use of topical steroids without sequelae and the final best-corrected visual acuity was as good as the base line. These keratitis infiltrates have been presumed to represent an immune response to the suspected adenoviral antigens deposited in corneal stroma during the primary adenoviral infection. Previous reports argued that patients with a history of adenoviral ketatoconjunctivitis were succeptible to adenoviral keratoconjunctivitis becoming reactivated; however, in our research, our patients had their first adenoviral infections after the eximer laser photorefractive surgery and reactivation was confirmed. We recommend that attention be paid to adenoviral infection after laser refractive operations, because these patients seem to have more frequent recurrences.
Eximer laser photorefractive surgery is one of the most widely performed ophthalmic surgeries. Keratitis after such surgeries is a serious complication and is multifactorial in origin. Moreover, prior ocular herpes is a contraindication in the labeling of refractive surgery by the U.S. Food and Drug Administration (FDA) due to the reactivation of herpetic keratitis. Previous reports have shown the reactivation of presumed adenoviral keratitis after laser in situ keratomileusis (LASIK), excimer laser keratectomy [1,2]. In this study, we report four cases of eximer laser photorefractive surgery which resulted in adenoviral keratoconjunctivitis in the postoperative period and then a late recurrence of epidemic keratoconjunctivitis (EKC)-like keratitis.
In April 2007, a 35-year-old woman showed the symptom of decreased vision in both eyes. She had a clinical history of adenoviral keratoconjunctivitis in both eyes, diagnosed three weeks earlier, and photorefractive keratectomy (PRK) in both eyes, diagnosed in December 1999. During the initial visit, the uncorrected visual acuity was 20 / 40, the best-corrected visual acuity (BCVA) was 20 / 20 in both eyes and the refraction was +1.50 +1.00 × 175 in the right eye and +0.50 +1.25 × 25 in the left eye. Central subepithelial infiltrates in both eyes, some of which were on the previous infiltration sites, were seen during the slit lamp examination. There was no significant conjunctival hyperemia and in the anterior chamber reaction no abnormal findings were seen in the eyelid or conjunctivae. The tear break up time (TBUT) was within normal limits. Little areas of epithelium overlying the infiltrates were stained with a fluorescein solution. The patient had been treated with a 7-months taper of prednisolone acetate 0.1% in both eyes four times a day and, by the end of the treatment, the subepithelial infiltrates persisted only in a small region.
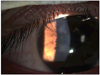
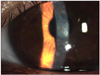
Four months after, in March 2008, the patient reported increased blurry vision in both eyes without conjunctival injection, pain, or tearing. Her BCVA was 20 / 30 in the right eye, 20 / 40 in the left eye and her refraction was -0.50 +1.00 × 175 in the right eye and -1.00 +1.25 × 25 in the left eye. Both of her cornea exhibited some small central subepithelial infiltrates (Fig. 1). She was treated with a 5-months taper of prednisolone acetate 0.1% in both eyes. There was significant improvement in her visual acuity. Her BCVA was 20 / 20 in the right eye and 20 / 25 in the left eye. Both central cornea had cleared, but some subepithelial opacity remained. On November 2008, two months after the last treatment, a subsequent third recrudescence of corneal inflammation occurred in both eyes and required treatment with prednisolone acetate 0.1%, which was tapered over a 2-month period. The sites of reactivated infiltrates were similar to previous lesion sites, but not all of them were in the same locations. Her vision had improved to the baseline and her corneal inflammation resolved, leaving only minimal opacity (Fig. 2). After discharging the use of prednisolone acetate 0.1%, cyclosporine A 0.05% (CsA, RestasisTM; Allergan Inc., Irvine, CA, USA) was started and further additional recurrence only recently occurred.
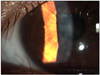
A 30-year-old woman was diagnosed in December 2008, showing decreased vision in both eyes. She had a clinical history of adenoviral keratoconjunctivitis in both eyes, diagnosed two weeks prior, and laser-assisted subepithelial keratectomy (LASEK) in both eyes diagnosed in August 2008. On the first visit, her BCVA was 20 / 40 in the right eye and 20 / 20 in the left eye, -1.00 +0.75 × 180 in the right eye and 20 / 20, +0.25 in the left eye. Some central subepithelial infiltrates, moderate conjunctival hyperemia in the both eyes (Fig. 3) were observed during the slit lamp examination. The sites of reactivated infiltrates were similar to previous lesion sites, but not all of them were in the same locations. There were no abnormal findings in the eyelids or conjunctivae, with the TBUT within normal limits. Little areas of epithelium overlying the infiltrates were stained with a fluorescein solution. The patient was treated with a 3-month taper of prednisolone acetate 0.1% in both eyes four times a day, resulting in subepithelial infiltrates persisting in only a small region. Her finalvision had improved to a BCVA of 20 / 20 in both eyes and the corneal inflammation resolved with minimal opacity (Fig. 4).
In June 2008, a 29-year-old woman showed symptom of decreased vision in her right eye. She had a clinical history of adenoviral keratoconjunctivitis in both eyes, diagnosed the previous year, and had LASEK in both eyes in January 2007, before adenoviral keratoconjunctivitis was found. In June 2008, her BCVA was 20 / 50, -0.75 +0.50 × 135 in the right eye and 20 / 20, -0.75 +0.50 × 95 in the left eye. The slitlamp examination disclosed some central subepithelial infiltrates in the both eyes, but there was no significant conjunctival hyperemia or anterior chamber reaction and there were no abnormal findings on the eyelid or conjunctivae, with the TBUT within normal limits. Little areas of epithelium overlying the infiltrates were stained with a fluorescein solution. The patient was treated with a 3-month taper of prednisolone acetate 0.1% four times a day. The subepithelial infiltrates persisted in only a small region. On October 2008, a subsequent second recrudescence of corneal inflammation occurred in her right eye, with some of the infiltrates on the sites of previous infiltrates. The infiltrates required treatment with prednisolone acetate 0.1% that was tapered over a 2-month period. Her vision improved and the EKC-like keratitis was resolved with minimal opacity. Finally, her vision improved to a BCVA of 20 / 20 in right eye.
In May 2009, a 23-year-old woman was examined, showing symptoms of decreased vision in her left eye. She had a clinical history of adenoviral keratoconjunctivitis in both eyes, diagnosed two weeks prior, and LASIK in both eyes, diagnosed in 2006. During the initial visit, her BCVA was 20 / 20 in her right eye and 20 / 30 in her left eye. Multiple subepithelial infiltration was found in her central cornea of her left eye on the slitlamp exam., but there was no significant conjunctival hyperemia or anterior chamber reaction. Furthermore, there were no abnormal findings on her eyelid or conjunctivae, and her TBUT was within normal limits. Little areas of epithelium overlying the infiltrates were stained with fluorescein solution. The patient was treated with a 2-month taper of prednisolone acetate 0.1% in her left eye four times a day and the subepithelial infiltrates persisted in only a small region. Her final vision had improved to a BCVA of 20 / 20 in both eyes. After discharging the use of prednisolone acetate 0.1%, cyclosporine A 0.05% (CsA, RestasisTM) was started and there was no further recurrence.
Summary of clinical courses of 4 cases is in Table 1. Adenoviral keratoconjunctivitis is a common eye infection that can induce subepithelial infiltrates, which can persist and recur. These infiltrates have been presumed to represent an immune response to suspected adenoviral antigens deposited in corneal stroma during the primary adenoviral infection [3].
Post-LASIK keratitis is a serious complication. FDA labeling advises that previous herpes keratitis is a contraindication of laser surgery, but no further specific instructions have been provided for other forms of keratitis. Campos et al. [4] and Pineda and Talamo [5] reported cases of patients who had undergone PRK and suffered from late-onset corneal haze following adenoviral keratoconjunctivitis, despite the fact that PRK was reported to eliminate central subepithelial corneal opacities and prevent recurrent keratitis within the treated area [6,7].
In previous reports on patients who had adenoviral ketatoconjunctivitis prior to undergoing LASIK, PRK reported that adenoviral ketatoconjunctivitis was reactivated after the surgery [1,2]. However, our patients had their first adenoviral infection episode after eximer laser photorefractive surgery and reactivation was confirmed. According to previous reports, it was recommended that careful preoperative history taking and physical evaluation should be undergone to detect even a remote history of prior episodes of adenoviral keratitis, and ophthalmologists should explain the possible reactivation of subepithelial infiltration to the patients [8]. In addition, we recommend paying attention to adenoviral infection after laser refractive operations, because these patients seem to have more frequencies of recurrence than patients who did not have eximer laser photorefractive surgery. Patients should receive warnings about adenoviral infection after laser refractive surgery.
Although no viral agent was isolated in our case, the clinical findings were consistent with previously reported adenoviral infections. The reactivation tendency of adenoviral keratitis was thought to be related to the eximer laser photorefractive surgery procedure; however, we found that the reactivation occurred when patients were under stressful conditions, such as physical fatigue and heavy drinking.
Recurrent adenoviral stromal keratitis is thought to represent a delayed hypersensitivity immune response to viral antigens in the corneal stroma [3]. The direct contact between epithelial cells and corneal stroma can cause abnormal results for corneal wound healing after PRK [6,7]. Moreover, hyperactive keratocytes or a loss of bowman's layer [5] may have induced the unusual responses after adenoviral keratoconjunctivitis in our patients. Thus, the patients who underwent eximer laser photorefractive surgery and did not have adenoviral keratitis before may have an increased possibility of reactivation of subepithelial infiltration, especially if they develop adenoviral keratoconjunctivitis after the surgery. Successful resolution of recurrent keratitis was achieved through the use of topical steroids without sequelae, both in our research and previous studies [1,2,8]. Withdrawal of topical corticosteroid could be a cause of the recurrence of inflammation [9]. Also, adenoviral keratoconjunctivitis can be complicated by a recurrence of subepithelial infiltrates with no evidence of an inciting factor. In two of our cases recurrence stopped after the use of cyclosporine A 0.05% (CsA, RestasisTM). Similar results were reported by Romanowski et al. [10], as topical cyclosporine A reduced adenoviral subepithelial immune infiltrates by anti-inflammatory and anti-immune effects, especially on T-cell activation.
Figures and Tables
 | Fig. 1Anterior segment photograhy showed multiple anterior stromal opacification after epidemic keratoconjucntivitis in case 1. |
 | Fig. 2After treating a 3rd recurrence, the corneal opacities were milder, but still remained (case 1). |
 | Fig. 3Anterior segment photograhy showed some subepithelial infiltrations after epidemic keratoconjunctivitis in case 2. |
References
1. Safak N, Bilgihan K, Gurelik G, et al. Reactivation of presumed adenoviral keratitis after laser in situ keratomileusis. J Cataract Refract Surg. 2002. 28:725–727.
2. Jabbur NS, O'Brien TP. Recurrence of keratitis after excimer laser keratectomy. J Cataract Refract Surg. 2003. 29:198–201.
3. Fite SW, Chodosh J. Photorefractive keratectomy for myopia in the setting of adenoviral subepithelial infiltrates. Am J Ophthalmol. 1998. 126:829–831.
4. Campos M, Takahashi R, Tanaka H, et al. Inflammation-related scarring after photorefractive keratectomy. Cornea. 1998. 17:607–610.
5. Pineda R, Talamo JH. Late onset of haze associated with viral keratoconjunctivitis following photorefractive keratectomy. J Refract Surg. 1998. 14:147–151.
6. Marshall J, Trokel SL, Rothery S, Krueger RR. Long-term healing of the central cornea after photorefractive keratectomy using an excimer laser. Ophthalmology. 1988. 95:1411–1421.
7. Meyer JC, Stulting RD, Thompson KP, Durrie DS. Late onset of corneal scar after excimer laser photorefractive keratectomy. Am J Ophthalmol. 1996. 121:529–539.
8. Randleman JB, Hewitt SM, Stulting RD. Delayed reactivation of presumed adenoviral subepithelial infiltrates after laser in situ keratomileusis. Cornea. 2004. 23:302–305.
9. Laibson PR, Dhiri S, Oconer J, Ortolan G. Corneal infiltrates in epidemic keratoconjunctivitis. Response to double-blind corticosteroid therapy. Arch Ophthalmol. 1970. 84:36–40.
10. Romanowski EG, Pless P, Yates KA, Gordon YJ. Topical cyclosporine A inhibits subepithelial immune infiltrates but also promotes viral shedding in experimental adenovirus models. Cornea. 2005. 24:86–91.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download