Abstract
Three-dimensional computed tomographic (3D-CT) angiography is a widespread imaging modality for intracranial vascular lesions. However, 3D-CT angiograms of an anterior communicating artery aneurysm associated with acute retrobulbar optic neuropathy have not been previously described. We present 3D-CT angiograms of an aneurysm of the anterior communicating artery that caused subarachnoid hemorrhage and vision loss in a 39-year old man. The 3D-CT angiograms were consistent with findings identified directly during surgery.
Three-dimensional computed tomographic (3D-CT) angiography has recently gained popularity for diagnosing intracranial vascular disease [1]. However, to our knowledge 3D-CT angiographic images of an anterior communicating artery aneurysm associated with acute retrobulbar optic neuropathy have never been reported. Here, we report a case of a ruptured anterior communicating artery aneurysm causing acute retrobulbar optic neuropathy that was examined by 3D-CT angiography.
A 39-year-old man presented to the emergency department of Soonchunhyang University Bucheon Hospital with disorientation and severe headache. Brain CT scans demonstrated subarachnoid hemorrhage. 3D-CT angiography of the brain (Somatom Sensation 16; Siemens, Forchheim, Germany) revealed a large aneurysm arising from the junction of the right anterior cerebral and the anterior communicating arteries that was oriented downward (Fig. 1A-1C). This finding prompted emergent neurosurgical intervention, during which the aneurysmal neck was clipped successfully (Fig. 1D). On the fifth postoperative day, the patient's mental status had improved and he complained of right eye vision loss. On ophthalmologic examination, the patient's visual acuity was no light perception (NLP) OD and 1.0 OS and his right pupil was nonresponsive. In retrospect, the patient recalled noticing a visual field defect encroaching from the inferior field in the right eye 10 days before admission, but he thought it was a manifestation of headache. The results of external, motility, and slit lamp examinations were all normal. The results of dilated fundus examinations were normal in both eyes, and the optic nerves in particular appeared normal. After three months, the vision in the patient's right eye remained NLP, and atrophy of the right optic nerve had occurred.
With recent advances of CT and magnetic resonance imaging, the diagnosis and treatment of cerebrovascular disease have become more accurate and effective. Acute retrobulbar optic neuropathy due to an anterior communicating artery aneurysm is rare, and to our knowledge 3D-CT angiographic images of this condition have never been reported.
Although sudden unilateral visual loss combined with signs of retrobulbar optic nerve dysfunction suggests a diagnosis of optic neuritis, especially when associated with normal looking discs, vascular and compressive lesions may be considered in certain cases. Diagnosis was straightforward in the present case. The patient presented with altered mental status and headache. Conventional CT revealed vascular pathology, and the choice of advanced vascular imaging modality was left to the physician. Although conventional digital subtraction angiography (DSA) is considered the most sensitive tool for detection of intracranial aneurysms, we did not perform DSA because it is an invasive study. Furthermore, considering the potential delays in time required to assemble the angiography team and perform the angiogram, CT angiography is often faster and is comparably accurate [2]. Magnetic resonance angiogram is another option, and it has advantages for the evaluation of cerebrovascular lesions. However, in our case, CT angiography was perceived to be faster and less likely to induce claustrophobia [3].
The choice of treatment modality is also worthy of discussion. Although endosaccular occlusion of the intracranial aneurysm was considered in the present case, urgent decompression of the aneurysm could not be achieved by this treatment because of the volume effect of the coils. In our patient, immediate decompression was mandatory and emergent surgical decompression with clipping of the aneurysm was identified as the treatment most likely to rescue vision [4].
Unfortunately, despite successful surgical decompression, the patient's vision did not recover. There are several explanations for monocular visual loss due to a ruptured anterior communicating artery aneurysm, including direct bleeding into the optic nerve, direct compression by the aneurysm [5], and interruptions of blood flow to arteries supplying posterior portions of the optic nerve as a result of either the subarachnoid hemorrhage itself, subsequent vasospasm, or the surgical clipping of the aneurysm [6]. The previous recognition of an inferior visual field defect 10 days before the attack suggests that direct compression of the optic nerve by the aneurysm was contributory.
Figures and Tables
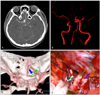 | Fig. 1Preoperative brain three-dimensional (3D) computed tomographic angiography images. (A) Enhanced axial view shows an aneurysm arising from the junction between the right anterior cerebral artery (ACA) and anterior communicating artery (AComA). (B) Vessel subtractional view shows a large aneurysm in the right ACA at the AComA junction oriented primarily downward. (C) 3D views show the large aneurysm arising from the junction of the right ACA and AComA, oriented primarily downward (blue arrow) toward the right optic nerve (green arrow). (D) Intra-operative view shows the right optic nerve (green arrow), internal carotid artery (blue arrow) and frontal lobe (blue star). After clipping, the ruptured aneurysm with its clip (green star) can be seen arising from the junction between the right ACA and AComA and the pinkish optic nerve (green arrow). |
Acknowledgements
We thank Dr. Nancy J. Newman (Director, Section of Neuro-Ophthalmology, Department of Ophthalmology, Emory University, Atlanta, GA, USA) for her critical review and proofreading of this manuscript.
References
1. Lovblad KO, Altrichter S, Viallon M, et al. Neuro-imaging of cerebral ischemic stroke. J Neuroradiol. 2008. 35:197–209.
2. Alberico RA, Patel M, Casey S, et al. Evaluation of the circle of Willis with three-dimensional CT angiography in patients with suspected intracranial aneurysms. AJNR Am J Neuroradiol. 1995. 16:1571–1578.
3. Thijs V. Imaging techniques for acute ischemic stroke: nice gadgets or essential tools for effective treatment? Neuroradiology. 2010. 52:169–171.
4. Craenen G, Brown SM, Freedman KA, et al. Rapid, painless unilateral vision loss in a 37-year-old healthy woman. Surv Ophthalmol. 2004. 49:343–348.
5. Chan JW, Hoyt WF, Ellis WG, Gress D. Pathogenesis of acute monocular blindness from leaking anterior communicating artery aneurysms: report of six cases. Neurology. 1997. 48:680–683.
6. Hara N, Mukuno K, Ohtaka H, Shimizu K. Ischemic optic neuropathy associated with subarachnoid hemorrhage after rupture of anterior communicating artery aneurysm. Ophthalmologica. 2003. 217:79–84.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download