This article has been
cited by other articles in ScienceCentral.
Abstract
Purpose
To introduce the clinical utility of the absolute value of the reconstructed waveform method in the analysis of multifocal visual evoked potential (mfVEP).
Methods
The mfVEP with 4-channel recording was performed using RETIscan® on 10 eyes of 10 normal subjects. Amplitudes were obtained from ring-shaped 6 areas and 4 sectors. The best visual evoked potential (VEP) response method and the absolute value of the reconstructed waveform method were compared in terms of analysis of the amplitudes. In order to assess the false positive rate of the examination, stimuli were administered with one-half of the cathode ray tube (CRT) monitor completely covered and the results were compared using 2 methods.
Results
The amplitudes in 6 areas and 4 sectors analyzed with the best VEP response method and the absolute value of the reconstructed waveform method showed no statistical difference (p > 0.05). The amplitude in the stimuli-blocked area of the absolute value of the reconstructed waveform method was smaller than that of the best VEP response method (p < 0.05) and the amplitude of the stimuli area showed no substantial difference between two methods (p > 0.05).
Conclusions
The absolute value of the reconstructed waveform method has similar reproducibility and lower level of false positives relative to the best VEP response method. Therefore, it can be considered as a useful method in the analysis of the mfVEP.
Go to :

Keywords: Absolute value of the reconstructed waveform method, Best visual evoked potential response method, Multifocal visual evoked potential
The multifocal visual evoked potential (mfVEP) is obtained from electric responses which are generated in a specific region via a cross-correlation following the simultaneous presentation of stimuli to the various regions of the visual field according to the pseudo-random sequence [
1]. Relative to conventional visual evoked potential, the mfVEP is made up of electric responses generated from a wide region of the visual field, and is capable of detecting a broad range of optic nerve damage. It can also detect local defects by providing the local electric responses from the visual field. Therefore, the clinical utility of the mfVEP has recently been extended as a diagnostic tool in optic neuritis, glaucoma and ischemic optic neuropathy [
2-
5].
Local mfVEP responses are obtained in a relatively short time due to the fast mfVEP sequence; each mfVEP response is not simply a 'little conventional visual evoked potential (VEP).' The pseudo-random sequence is chosen in a certain way and local mfVEP responses of multiple sectors are calculated with a sophisticated mathematical algorithm. Therefore, there is no standardized analytical method, and manufacturers of multifocal equipment use different analytical methods for extracting the multifocal responses [
6]. The best VEP response method is now extensively employed to gather and analyze all the waveforms recorded in each channel. This method selects the best response, which has the largest amplitude among visual evoked potentials recorded in each channel. Therefore, it is difficult to use the best VEP response to represent the entire range of visual evoked potential, because a large amplitude noise can be analyzed as the optical response. To remedy of these drawbacks, the absolute value of the reconstructed waveform method was newly devised. The absolute value of the reconstructed waveform method reconstructs new waveforms and calculates the approximation of the largest amplitude of visual evoked potential.
In this study, the mfVEP was conducted on the normal eyes. The amplitudes of waveforms were compared between the best VEP response method and the absolute value of the reconstructed waveform method according to 6 areas from the foveal center, 4 sectors and presence of stimulus. The aim of this study was to evaluate the clinical utility of the absolute value of the reconstructed waveform method in the analysis of the mfVEP.
Materials and Methods
Ten normal subjects who visited our clinic from May to June in 2008 with no known systemic disease and ophthalmic disease participated in this study. Ten normal subjects included 5 males and 5 females, ranging in age from 25 to 32 years (mean, 28 years). Best corrected visual acuity of all subjects was 1.0. After correction of refractive errors, the right eye of each subject was examined without pupil dilatation.
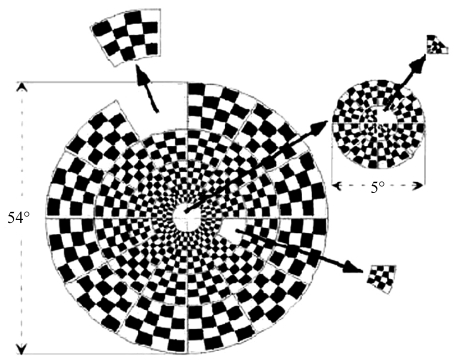
The mfVEP was conducted using RETIscan® (Roland, Brandenburg, Germany). The distance to the 21-inch color cathode ray tube (CRT) monitor was 30 cm, which corresponded to a total subtense of the stimulus of 54°. The stimulus consisted of 60 sectors, each with 16 checks, 8 white checks and 8 black checks. Luminance of the white check was 200 cd/m
2 and luminance of the black check was <1 cd/m
2, producing a Michelson contrast of 99%. The visual stimuli were generated on a computer screen with a repetition rate of 50 Hz and the pattern of reversals for each sector followed a pseudo-random sequence. The sectors and the checks were scaled, based on cortical magnification factor, to be of approximately equal effectiveness for cortical stimulation with a gradual increase in check size from the center to outer segments (
Fig. 1). Background luminance of the screen was maintained at a maximal level of 200 cd/m
2.
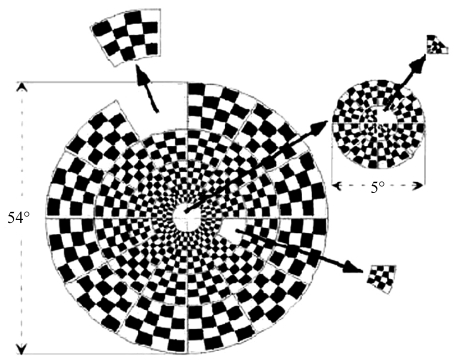 | Fig. 1The schematic representation of multifocal visual evoked stimulus. Each of the 60 sectors of the display is an independent stimulus with 16 checks, 8 black and 8 white. 
|
Gold cup electrodes were placed on the occipital scalp using electroencephalography (EEG) paste to minimize the impedance to less than 5 kΩ. After preliminary experiments with multiple electrode positions and combinations, four bipolar channels with different orientations were determined which consistently produced larger signals, and when combined provided the best coverage of all points in the visual field [
7]. These positions were then employed in this study. Two active electrodes (Oz) were placed along the vertical midline 4 cm above the inion and 3 cm below the inion. Two additional active electrodes were placed 4 cm on either side of the inion. A forehead electrode placed at the glabella served as the reference electrode (Fz) and an earlobe electrode served as the ground electrode (Cz) (
Fig. 2). These electrode placements were based on the 4-channel recording of Klistorner and Graham [
7]. The distance between electrode and inion was modified based on anatomical consideration of the cortical configurations in Koreans. At present, this modified 4-channel recording was the most widely employed technique for the mfVEP recording.
 | Fig. 2The positions of four active electrodes (A-D) and inion (red circle) and the configuration of the four channels of recording of the multifocal visual evoked potential. 
|
The range of amplitude was ±100 µV. The low- and high-frequency cut-offs were set to 1 Hz and 30 Hz, respectively. The result curve length was 333 ms. Two minutes 20 seconds was required for one cycle, and four cycles were carried out for each subject. The signals were bandpass filtered at 50 and 100 Hz to remove noises in the process of extracting waveforms. The same stimuli were administered to all subjects with the same electrode positions to obtain the mfVEP responses. The extracted waveforms were analyzed via two methods, namely the best VEP response method and the absolute value of the reconstructed waveform method.
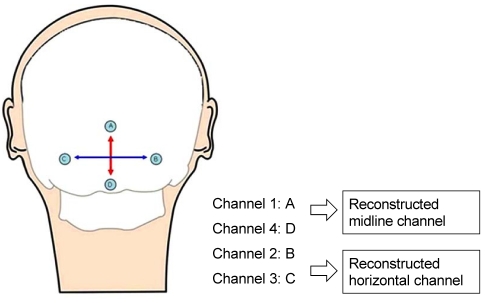
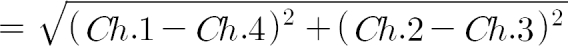
The best VEP response method was the custom-designed program of RETIscan®. The waveform of maximal amplitude among various waveforms recorded in each channel was selected. In contrast, the absolute value of the reconstructed waveform method was designed to calculate the approximation of maximal amplitude of visual evoked potential. A midline channel was reconstructed as the difference between channel 1 and channel 4. A horizontal channel was reconstructed as the difference between channel 2 and channel 3. A new waveform was acquired via calculation with the absolute values recorded in two reconstructed channels. A new formula was designed to calculate the average of absolute values of visual evoked potentials and the approximation of maximal amplitude (
Fig. 3).
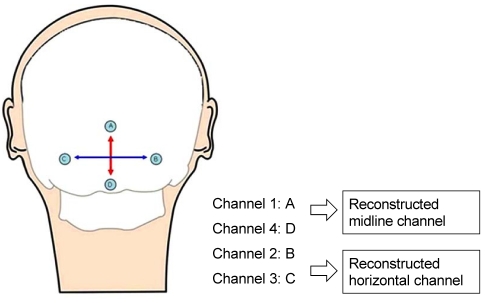 | Fig. 3The schematic representation of the absolute value of the reconstructed waveform method. A midline channel is reconstructed as the difference between channel 1 and channel 4. A horizontal channel is reconstructed as the difference between channel 2 and channel 3. The positions of the four active electrodes (A-D) are shown. 
|
A formula of the absolute value of the reconstructed waveform method was as follows.
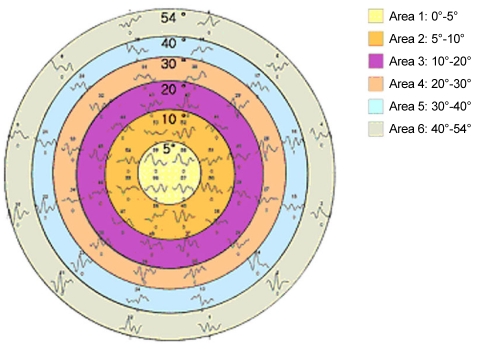
The amplitudes of waveforms were analyzed via the absolute value of the reconstructed waveform method and the best VEP response method. Each amplitude was compared according to the ring-shaped 6 areas and 4 sectors to find the reproducibility of the absolute value of the reconstructed waveform method. The ring-shaped 6 areas were determined by the distance from the foveal center, that is, 0°-5° (area 1), 5°-10° (area 2), 10°-20° (area 3), 20°-30° (area 4), 30°-40° (area 5), 40°-54° (area 6) (
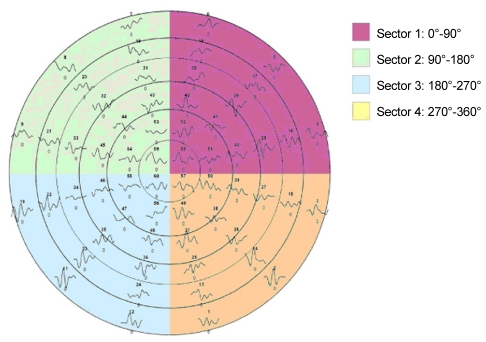
Fig. 4). The 4 sectors were determined by horizontal meridian, that is, 0°-90° (sector 1), 90°-180° (sector 2), 180°-270° (sector 3), 270°-360° (sector 4) (
Fig. 5).
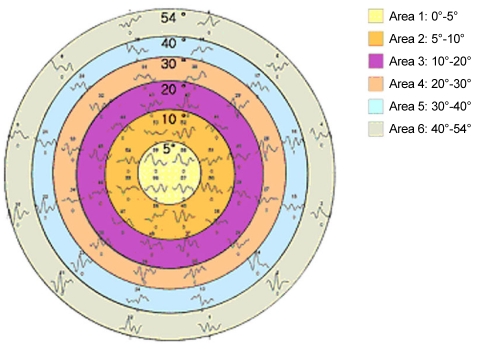 | Fig. 4Areas 1 to 6 according to the distance from the foveal center are represented in the schematic diagram. 
|
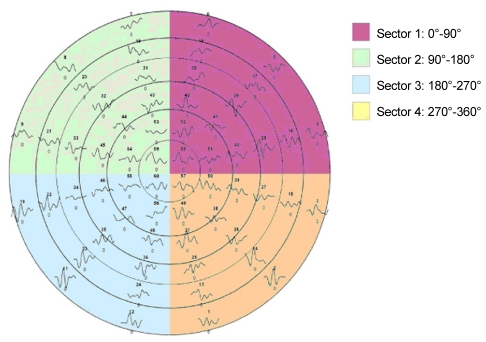 | Fig. 5Sectors 1 to 4 as determined by the horizontal meridian are represented in the schematic diagram. 
|
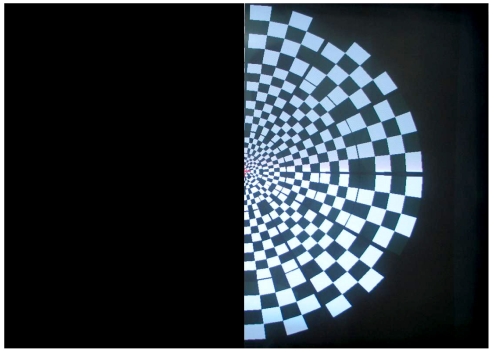
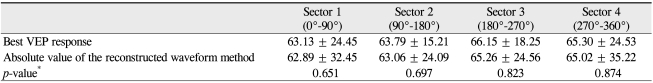
The mfVEP has small amplitudes and waveforms can be easily affected by noise. In order to assess the false positive rate of the examination, stimuli were administered with one-half of the CRT monitor covered completely. The amplitudes of waveforms in the stimuli-blocked nasal area and stimuli-unblocked temporal area were compared using the two aforementioned methods (
Fig. 6).
 | Fig. 6The schematic representation of cathode ray tube (CRT) monitor with nasal side covered completely. Stimuli were administered with one-half of the CRT monitor covered completely to stimulate the temporal retina of right eye to determine the false positives of the examination. 
|
Statistical analysis was performed using Mann-Whitney U-test in SPSS ver. 14.0 (SPSS Inc., Chicago, IL, USA). A p-value of less than 0.05 was considered statistically significant.
Go to :

Results
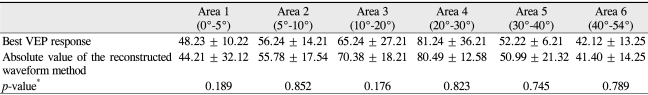
Comparing the amplitudes of waveforms analyzed with the best VEP response method and the absolute value of the reconstructed waveform method according to the area from the foveal center, we detected no statistical differences between the two methods (
p > 0.05) (
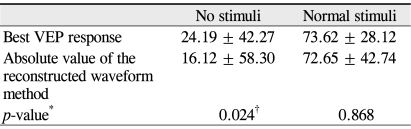
Table 1).
Table 1
The mean amplitude (nV) divided into areas analyzed via the best VEP response method and the absolute value of the reconstructed waveform method
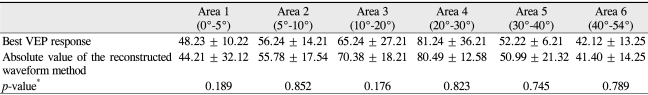

The amplitude of waveform in area 1 is slightly larger in the best VEP response method (p = 0.189). On the contrary, the absolute value of the reconstructed waveform method assessed the amplitude of waveform in area 3 slightly larger than the best VEP response method, however this was not a significant difference (p = 0.176).
The amplitudes of waveforms analyzed with the best VEP response method and the absolute value of the reconstructed waveform method were compared according to the sectors. The amplitudes of waveforms in all sectors were highly assessed via the best VEP response method, but no significant differences were noted between the two methods (
p > 0.05) (
Table 2).
Table 2
The mean amplitude (nV) divided into sectors analyzed via the best VEP response method and the absolute value of the reconstructed waveform method
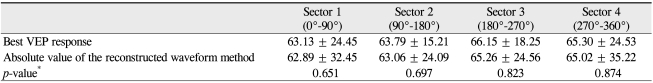

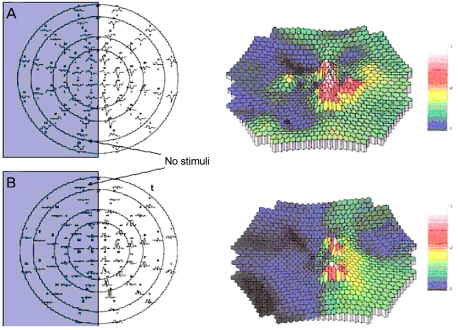
The two methods were compared according to the presence of stimuli. The absolute value of the reconstructed waveform method assessed the amplitude of waveform in the stimuli-blocked nasal area substantially smaller than the best VEP response method (
p < 0.05) (
Table 3 and
Fig. 7). The amplitude of waveform in the stimuli-unblocked temporal area was also smaller in the absolute value of the reconstructed waveform method, but no statistical significance was noted (
p > 0.05) (
Table 3).
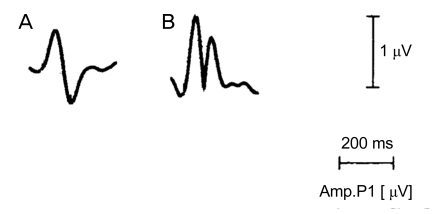
 | Fig. 7The mean amplitude analyzed by the absolute value of the reconstructed waveform method (B) in the stimuli-blocked area was smaller than that by the best visual evoked potential response method (A). 
|
Table 3
The mean amplitude (nV) according to presence of stimuli analyzed via the best VEP response method and the absolute value of the reconstructed waveform method

Go to :

Discussion
An evoked potential is an electrical response recorded from the motor nervous system or sensory nervous system following presentation of a stimulus when a proper stimulus such as electrical stimulus is given to activate a nervous system. VEP is an evoked potential caused by a visual stimulus and is recorded at the scalp, using standard EEG technique [
8]. Visual evoked response (VER), and visual evoked cortical potential (VECP) are interchangeably used. VEP can provide important diagnostic information with regard to the functional integrity of the visual system. Therefore, VEP has been used as a useful objective test in the diagnosis of multiple sclerosis, optic neuritis and assessment of non-organic visual loss. Even when a disease involving the visual pathway is suspected or if a fundus examination is impossible due to media opacity, VEP is usefully employed [
8-
10].
However, clinical use of VEP has limitation in several ways. First, the pattern reversal VEP can be recorded to a display of at least 15° in diameter. Thus, local defects can easily be missed. Second, the bright flash VEP uses full-field illumination and elicits a mass response from the anterior visual pathway. Thus, responses from abnormal regions of the field are summed with those from normal regions. Furthermore, the pattern reversal VEP is dominated by responses from the lower field in most individuals. Thus, large defects in the upper field can be missed with the conventional VEP. In general, the lack of spatial information limits the usefulness of the technique [
6,
11-
15].
On the contrary, the mfVEP provides local VEP responses from the visual field. The technique combines conventional VEP recording techniques with a display that is subdivided into a number of regions, each of which has an independent stimulus controlled by specialized software [
6]. The mfVEP responses consist of responses extracted from the 40 to 50° radius of the visual field. The mfVEP can detect a broader range of optic damage than conventional VEP. Moreover, the mfVEP can provide local defects without summing with responses from abnormal and normal regions compared with the flash VEP. The mfVEP is widely used as an adjunctive tool in the diagnosis of glaucoma, ischemic optic neuropathy and retinal vessels disease as well as optic neuritis due to these advantages [
2-
5]. Hood et al. [
16] tested 20 patients with unilateral field losses owing to either ischemic optic neuropathy or glaucoma, and compared the mfVEP amplitude with the results of a Humphrey visual field (HVF) test. They reported that the interocular ratio of the mfVEP amplitudes was strongly correlated with the difference between HVF values of the two eyes, and this correlation improved with increased signal-to-noise ratio (SNR). Hood et al. [
4] also obtained HVF and the mfVEP recordings from three patients with visual field defects due to optic neuritis, and reported that the mfVEP can be employed to track the change of local optic nerve damage.
Surface potential fields produced by cortical activity are described by an equivalent dipole source perpendicular to the cortical surface. On the basis of cortical topography, horizontally oriented bipolar electrodes straddling the inion are optimal for registration of the horizontally oriented dipoles. The evoked potential of a particular region is recorded in a single channel corresponding to a single dipole source, and a single channel recording cannot obtain every evoked potential of cortical dipole because of three dimensional structure of visual cortex [
7,
13,
17]. Therefore, multi-channel recording is necessary to record all visual evoked potentials of 50° radius of the visual field. Slotnick et al. [
18] found each dipole was contralateral to the corresponding stimulus patch of primary visual cortex. A retinotopic map of primary visual cortex was obtained with two techniques, a multi-stimulus array and multi-electrode VEP dipole source localization. The dipole retinotopic organization and continuity across the horizontal meridian indicated that this multi-channel recording revealed primary visual cortex activation.
Analytic tools were devised to collect and analyze all waveforms from each channel in multi-channel recording. The best VEP response method of RETIscan® and the best array method of VERIS system™ (Electro-Diagnostic Imaging, Redwood City, CA, USA) are the typical examples used for the analysis of the mfVEP. The best of the responses from all channels were analyzed and response with the largest SNR was selected in the best array method [
19,
20]. The VEPs of cortical dipoles are recorded in each channel by using dipole source localization procedures in RETIscan®. For example, the amplitude of VEP recorded with the midline channel is proportional to cos α. The amplitude of VEP recorded with the lateral channel is proportional to sin α [
21] (
Fig. 8). The best VEP response method selects the best response, which has the largest amplitude among the VEPs recorded in each channel in this fashion. This method shows the full range of responses but unselected local responses can result in errors in the analysis of the mfVEP. Moreover, noise with a large amplitude can be analyzed as the best response.
 | Fig. 8A schematic diagram for determining the orientation of a dipole. Each circle indicates the location of an electrode. α is angle between a dipole and the midline channel. Cos α is obtained from the coefficient from the midline channel and sin α is obtained from the coefficient from the lateral channel. 
|
The absolute value of the reconstructed waveform method was devised to analyze the VEPs of cortical dipoles themselves. A midline channel is reconstructed as the difference between channel 1 and channel 4. A horizontal channel is reconstructed as the difference between channel 2 and channel 3. A new formula is devised to acquire the new waveform from the absolute values of these two reconstructed channels and to approximate the largest amplitude of VEP. This method tried to reproduce the amplitude as close as possible to the real largest amplitude, and the reproduced waveform is slightly different from the real waveform. All waveforms have positive deflection because the new waveform is obtained from the absolute value. Therefore, the comparison between the two methods was conducted using amplitude, not waveform (
Fig. 9).
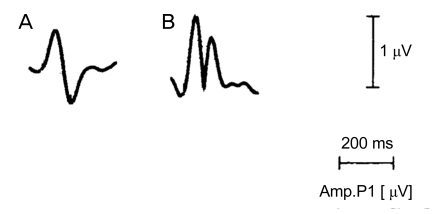 | Fig. 9Waveforms of the visual evoked potential (VEP) response in two methods: waveform (A) analyzed by the best VEP response method and waveform (B) analyzed by the absolute value of the reconstructed waveform method showing the positive deflection. 
|
The amplitude of the waveform analyzed via the best VEP response method and the absolute value of the reconstructed waveform method showed no significant difference according to 6 areas and 4 sectors. In this regard, the absolute value of the reconstructed waveform method is believed to have reproducibility similar to that of the best VEP response method. The amplitude of the waveform in the stimuli-blocked area is assessed as smaller via the absolute value of the reconstructed waveform, and this method is also believed to result in fewer false positives. We attempted to compare the amplitudes of 60 sectors in order to quantify false positives, but amplitudes were too small to allow a real signal to be differentiated from noise, thus the false positive rate could not be calculated.
This study did not compare the results between the two methods according to the stimulus time. A test for each subject required approximately 9 minutes for each cycle, with four cycles in total in this study, but a test time has not yet been standardized. Hood et al. [
19] established a test time of at least 28 minutes - 7 minutes for each cycle with four cycles in total. Chen et al. [
22] established a test time of 14 minutes - 7 minutes for each cycle with two cycles in total. If the shortest appropriate stimulus time to obtain the proper waveforms can be established, the mfVEP could be employed more widely and easily in the clinics. Zhang et al. [
23] suggested that the mean noise window SNR value should be equal to or better than approximately 0.5 by comparing the waveform between two eyes to improve the quality of the mfVEP records. In this respect, an interocular comparison of the mfVEP is clearly necessary. They also suggested the several techniques to reduce the contamination of records by the alpha wave, which was the low frequency wave generated from the occipital lobe in the relaxed state. First, the experimenter can continuously monitor the VEP records and provide feedback to the subject. Second, attempts should be made to keep the resistance of all electrodes as low, and as similar as possible.
In conclusion, the absolute value of the reconstructed waveform method has good reproducibility and relatively lower level of false positives. This method can be a useful tool in analyzing the mfVEP and detecting the abnormalities of the visual system. Further studies are required to determine the clinical utility of the absolute value of the reconstructed waveform method via application to animal or human patients.
Go to :






 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download