Abstract
A 60-year-old man with bilateral corneal opacity underwent cataract extraction surgery involving the use of a limbal relaxing incision in his left eye. He had lower lid ectropion and lagophthalmos in both eyes. Eleven days after the surgery, a slit-lamp examination revealed a neurotrophic corneal ulcer with a punch-out epithelial defect and rolled edges at the center of the pre-existing corneal opacity. The patient was treated with sodium hyaluronate, autologous serum, and oral doxycycline. Six weeks after the surgery an improvement in corneal sensation was observed and the neurotrophic corneal ulcer subsequently healed over the course of one year. In this report, we present a case of neurotrophic keratitis that occurred after performing cataract surgery concurrent with a limbal relaxing incision. As such, we suggest that limbal relaxing incisions should be performed cautiously in patients with causative risk factors for corneal hypesthesia.
Astigmatism control is now regarded as an important component in optimizing visual outcomes after cataract surgery [1]. Limbal relaxing incisions appear to be a safe and effective technique for reducing postoperative corneal astigmatism [2,3]. Neurotrophic keratitis is a degenerative disorder of the corneal epithelium that results from the loss or absence of corneal sensation. The most common cause of this disorder is corneal hypoesthesia associated with herpes virus infection [4]. However, neurotrophic keratitis can develop after cataract surgery [5,6]. This report describes a case of a neurotrophic corneal ulcer following cataract surgery during which a limbal relaxing incision was made to treat astigmatism.
A 60-year-old man underwent an uneventful cataract surgery on his left eye, which involved the performance of a 3 mm clear corneal incision on the superior nasal side in another hospital. In order to correct the left eye astigmatism, a limbal relaxing incision was made opposite the corneal incision wound. This incision was 0.5 mm deep with a 70° arc width along the keratometric steep axis (135°). The patient had a history of bilateral severe conjunctivitis during childhood and had right facial nerve palsy 20 years ago. At the time of surgery he had lower lid ectropion and lagophthalmos in both eyes.
On postoperative day 11 the patient developed abrupt-onset ocular pain in his left eye. Slit-lamp biomicroscopy revealed a punch-out epithelial defect (1.5 × 1.5 mm) with a border of hazy epithelium along with stromal edema on the pre-existing corneal opacity near the limbal relaxing incision consistent with clinical stage 2 neurotrophic keratitis (Fig. 1) [7]. The best corrected visual acuity (BCVA) was 20 / 200 (-0.25 diopters [D] -1.00 D × 45) in the left eye. Topical preservative-free sodium hyaluronate (0.3% [w/v]) and topical levofloxacin (5 mg/mL) were prescribed to be administered four times daily. Laboratory examination confirmed no bacterial growth, and serological results were negative for collagen vascular disease.
A corneal sensitivity test using a Cochet-Bonnet esthesiometer (Luneau Ophthalmology, Chartres Cedex, France) revealed decreased sensation in the inferior and infero-temporal areas of the left cornea compared to other locations in the left cornea and to all locations in the right (non-operated) cornea (p < 0.05) (Table 1). Interestingly, areas of the non-operated cornea varied in sensitivity. Tests revealed decreased sensation at the center of opacity in the inferior areas as compared to other locations on the non-operated cornea (p < 0.05) (Table 1).
The size of the epithelial defect had decreased to 1.0 × 1.0 mm by postoperative day 13, at which time the patient's BCVA was 20 / 70 (-0.25 D -1.50 D × 45) in the left eye. At 4 weeks post-operation, the patient's vision had improved to 20 / 50 (-0.25 D -1.50 D × 45°), but the epithelial defect had not improved. By the 6th week, the patient's vision had improved to 20 / 30 (-0.25 D -1.50 D × 45°), but the epithelial defect persisted. The corneal sensation in the infero-temporal cornea had improved (Fig. 2), but remained lower than that observed at other locations in the left cornea and at all locations in the right cornea, until 5 months after surgery (Table 1).
The patient was admitted to our hospital 10 months after surgery, at which time he presented with a BCVA of 20 / 40 (+0.75 D -5.00 D × 40) in his left eye. Slit-lamp biomicroscopy revealed an oval-shaped epithelial thinning (1.5 × 1.5 mm) and some erosion of the pre-existing corneal opacity (Fig. 3). The corneal sensation was 50.0 mm at all locations in both corneas, with the exception of the infero-temporal cornea of the left eye, where it was 40.0 mm. The patient was treated with 50% (v/v) autologous serum eye drops 8 times daily [8] and 100 mg of oral doxycycline twice a day for 2 months. At the most recent follow-up, the patient showed no symptoms, and the BCVA for his left eye remained at 20 / 40 (+0.75 D -5.00 D × 40). Slit-lamp biomicroscopy indicated that the corneal epithelium had completely healed. The corneal sensation of the infero-temporal cornea in the left eye was 45.0 mm.
This report describes a case of neurotrophic corneal ulcer development following cataract surgery that involved the use of a limbal relaxing incision in a patient with corneal opacity. At 11 days post-operation, stage 2 neurotrophic keratitis was observed on the previous corneal opacity. Corneal sensation in this area improved from 6 weeks after surgery, but did not fully recover to that of other corneal locations. The neurotrophic corneal ulcer healed over the course of 1 year.
Injury to the corneal nerve fibers can impair corneal healing [4]. Cataract extraction surgery requires a corneal incision which can cause corneal nerve injury and hyphoesthesia [9,10]. The amount of mechanical disruption of corneal nerve fibers is a function of the length of the corneal incision [10]. Previous studies reported that detrimental changes in all parameters of corneal sensitivity were immediately detected after phacoemulsification with a clear corneal incision, and that corneal sensitivity did not return to preoperative levels until 3 months after the procedure [11,12]. In the case reported herein, a 3 mm clear corneal incision was created on the superior nasal side, while a limbal relaxing incision consisting of a 70° arc width was generated along the keratometric steep axis (135°) on the opposite side of the corneal incision. At 11 days after surgery, stage 2 neurotrophic keratitis was observed on the previous corneal opacity in the infero-temporal region of the cornea, adjacent to the limbal relaxing incision. A corneal sensitivity test revealed decreased sensation in the corneal ulcer area adjacent to the limbal relaxing incision of the left cornea compared to other locations in the left cornea and to all locations in the right (non-operated) cornea (Table 1). Corneal sensation in this area improved from 6 weeks after surgery, but did not fully recover to that of other corneal locations. Therefore, long limbal relaxing incisions used as an adjuvant may contribute to decreased corneal sensation to a significantly greater extent than the generation of a clear corneal incision alone, resulting in development of a neurotrophic corneal ulcer.
This patient presented symptoms indicative of corneal opacity in both eyes. The corneal sensitivity at the center of the opacity in the non-operated eye was found to be below normal levels, suggesting that the corneal sensitivity of the operated eye was also lower than normal prior to surgery. The patient had a history of bilateral severe conjunctivitis during childhood and right facial nerve palsy 20 years ago. He had lower lid ectropion and lagophthalmos in both eyes. We hypothesize that he might have exposure keratitis resulting in corneal hypesthesia in inferior locations. The operated eye displayed severely decreased corneal sensation after surgery compared to the non-operated eye. Improved sensation in the neurotrophic ulcer area occurred very slowly, and at 10 months after surgery the sensation remained below the level of that in the non-operated eye.
The current therapeutic options for neurotrophic keratitis include intensive artificial tear supplements, punctal occlusion, contact lenses, and appropriate management of adnexal disease. In our patient, the corneal hypoesthesia and the epithelial defect took nearly one year to resolve. The corneal lesion improved steadily in response to the administration of 50% (v/v) autologous serum eye drops. Autologous serum contains growth factors, vitamins, and immunoglobulins that are believed to improve neurotrophic keratitis [13,14].
A limitation of this study was that corneal sensation was not measured preoperatively. The patient was referred to us after the cataract operation. We believe that corneal sensation should be measured before performing cataract surgery that involves the use of limbal relaxing incisions, especially in patients with neurotrophic keratitis risk factors such as pre-existing exposure keratitis, herpes simplex keratitis, diabetes, or old age. Depending on the patient's characteristics, it may be more appropriate to use other methods of astigmatism correction, such as toric intraocular lens insertion.
This report describes the development of neurotrophic keratitis following phacoemulsification surgery involving the use of a long limbal relaxing incision. The neurotrophic corneal ulcer healed over the course of one year, but the corneal hypesthesia did not recover to the level of the non-operative eye. Limbal relaxing incisions, which are accepted as an effective and safe method for correcting astigmatism during cataract surgery, should be performed with caution in patients with decreased corneal sensation.
Figures and Tables
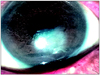 | Fig. 1Slit-lamp biomicroscopy on postoperative day 11. Note the punch-out epithelial defect (1.5 × 1.5 mm) with a border of hazy epithelium and stromal edema on the pre-existing corneal opacity, consistent with clinical stage 2 neurotrophic keratitis. |
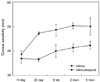 | Fig. 2The postoperative change in the mean corneal sensitivity. These data show the sensitivity of the inferior and infero-temporal cornea over the span of the first five months following surgery. |
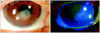 | Fig. 3Slit-lamp biomicroscopy at 10 months post-surgery. Note the oval-shaped epithelial thinning (1.5 × 1.5 mm) (A) and some erosion of the pre-existing corneal opacity (B). |
Acknowledgements
This study was supported by a grant from the Korea Healthcare Technology R&D Project, Ministry for Health, Welfare & Family Affairs, Republic of Korea (A090136).
References
1. Mamalis N. Correction of astigmatism during cataract surgery. J Cataract Refract Surg. 2009. 35:403–404.
2. Bayramlar HH, Dağlioğlu MC, Borazan M. Limbal relaxing incisions for primary mixed astigmatism and mixed astigmatism after cataract surgery. J Cataract Refract Surg. 2003. 29:723–728.
3. Kim HJ, Kim JW, Ahn JE. Limbal relaxing incision combined with cataract surgery reducing preoperative corneal astigmatism. J Korean Ophthalmol Soc. 2002. 43:1892–1900.
4. Davis EA, Dohlman CH. Neurotrophic keratitis. Int Ophthalmol Clin. 2001. 41:1–11.
5. John T. Corneal sensation after small incision, sutureless, one-handed phacoemulsification. J Cataract Refract Surg. 1995. 21:425–428.
6. Kohlhaas M, Stahlhut O, Tholuck J, Richard G. Development of corneal sensitivity after phacoemulsification with scleral tunnel incision. Klin Monbl Augenheilkd. 1997. 211:32–36.
7. Bonini S, Rama P, Olzi D, Lambiase A. Neurotrophic keratitis. Eye (Lond). 2003. 17:989–995.
8. Jeng BH, Dupps WJ Jr. Autologous serum 50% eyedrops in the treatment of persistent corneal epithelial defects. Cornea. 2009. 28:1104–1108.
9. Kohlhaas M. Corneal sensation after cataract and refractive surgery. J Cataract Refract Surg. 1998. 24:1399–1409.
10. Lyne A. Corneal sensitivity after surgery. Trans Ophthalmol Soc U K. 1982. 102(pt 2):302–305.
11. Khanal S, Tomlinson A, Esakowitz L, et al. Changes in corneal sensitivity and tear physiology after phacoemulsification. Ophthalmic Physiol Opt. 2008. 28:127–134.
12. Kim YM, Kim SW, Kim TI, et al. The change of corneal sensitivity and recovery of corneal nerve after cataract surgery. J Korean Ophthalmol Soc. 2007. 48:13–18.
13. Quinto GG, Campos M, Behrens A. Autologous serum for ocular surface diseases. Arq Bras Oftalmol. 2008. 71:6 Suppl. 47–54.
14. Matsumoto Y, Dogru M, Goto E, et al. Autologous serum application in the treatment of neurotrophic keratopathy. Ophthalmology. 2004. 111:1115–1120.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download