Abstract
Purpose
To compare the short-term effects of intravitreal triamcinolone acetonide (IVTA) with those of intravitreal bevacizumab (IVB) injection for diabetic macular edema (DME).
Methods
The present retrospective, comparative case study included 58 eyes of 35 consecutive patients (IVTA group, 20 eyes; IVB group, 38 eyes) with DME. IVTA (4 mg) or IVB (1.25 mg) injection was performed under local anesthesia. The effects of injection for DME were evaluated using best-corrected visual acuity (BCVA), central macular thickness (CMT) by optical coherence tomography and intraocular pressure (IOP) by applanation tonometer. Patients underwent eye examinations, including BCVA, CMT, and IOP at pre-injection, 2, 4, and 8 weeks after injection.
Results
BCVA (logarithm of the minimum angle of resolution) ± SD at pre-injection, 2, 4, and 8 weeks after injection was 0.67 ± 0.40, 0.56 ± 0.35 (p = 0.033), 0.55 ± 0.33 (p = 0.041), and 0.43 ± 0.31 (p = 0.001) in the IVTA group and 0.51 ± 0.31, 0.42 ± 0.26 (p = 0.003), 0.43 ± 0.32 (p = 0.001), and 0.43 ± 0.27 (p = 0.015) in the IVB group, respectively. CMT (µm) ± SD at pre-injection, 2, 4, and 8 weeks after injection was 400.4 ± 94.9, 332.8 ± 47.4 (p = 0.002), 287.5 ± 49.1 (p = 0.007), and 282.5 ± 49.6 (p = 0.043) in the IVTA group and 372.6 ± 99.5, 323.2 ± 72.4 (p = 0.077), 360.9 ± 50.3 (p = 0.668), 368.2 ± 88.6 (p = 0.830) in the IVB group, respectively.
Macular edema is the most important manifestation of non-proliferative diabetic retinopathy and is a predominant cause of legal blindness in diabetic patients [1]. Among treatments under investigation for diabetic macular edema (DME), intravitreal injection of triamcinolone acetonide [2-9] and anti-angiogenic agents, such as bevacizumab [10,11], pegaptanib [12] and ranibizumab [13], have been reported to have favorable short-term anatomical and visual results in patients with DME. Recently, several promising results have been shown in different studies regarding the treatment of refractory diabetic macular edema with intravitreal triamcinolone acetonide (IVTA) and intravitreal bevacizumab (IVB) [4,14,15]. Due to the promising preliminary study results, the anatomical and visual acuity outcomes associated with IVTA in the management of DME were compared with those of IVB in the present study.
The present retrospective, comparative case study included 58 eyes of 35 consecutive patients (IVTA group, 20 eyes; IVB group, 38 eyes) with DME. The major inclusion criteria for the study included 1) decreased best-corrected visual acuity (BCVA) caused by DME, 2) definite retinal thickening resulting from DME on clinical examination involving the center of the macula and assessed to be the main cause of visual loss, and 3) DME confirmed via slit-lamp biomicroscopy or retinal thickness measured on 300 µm optical coherence tomography (OCT) or fluorescein angiography. Exclusion criteria included 1) macular edema with vitreous hemorrhage, 2) history of cataract surgery and/or vitrectomy within the previous six months or during the treatment period for diabetic macular edema, 3) prior treatment with IVTA or IVB (at any time): peribulbar steroid injection within the previous six months, photocoagulation for DME within the previous three months, 4) other ocular comorbidity that might exert influence on macular thickness or visual acuity such as central retinal vein occlusion, branch retinal vein occlusion, or uveitis, severe macular ischemia, and 5) history of previous glaucoma treatment such as medical and/or surgical treatment. Intravitreal injection of triamcinolone acetonide 4 mg or bevacizumab 1.25 mg injection was performed with a 30-gauge needle through the inferotemporal quadrant under sterile conditions using local anesthesia. The effects of intravitreal injection for DME were evaluated according to BCVA and central macular thickness (CMT) using OCT (Stratus Zeiss Humphrey, San Leandro, CA, USA). OCT images were acquired using the fast macular thickness map scan conducted by a single skilled examiner, and macular thickness was measured via retinal map analysis for the calculation of average macular thickness. BCVA measurements were based on the Snellen chart and were converted to the logarithm of the minimum angle of resolution (logMAR) scale for statistical evaluation. Patients underwent eye examinations, including intraocular pressure (IOP) with a tonopen applanation tonometer, BCVA, stereoscopic biomicroscopy of the macula, and CMT measurement using OCT at pre-injection, as well as 2, 4, and 8 weeks after injection. After examination of OCT, repeated injections were performed for patients with decreased visual acuity. Glycosylated hemoglobin (HbA1c) and history of hypertension were measured at baseline.
The data were analyzed using SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA). Comparisons within a group were analyzed using the Wilcoxon signed rank test, paired t-test, and the chi square test, and comparisons between the two groups were analyzed using the Mann-Whitney test. All p-values of less than 0.05 were considered statistically significant compared to those pre-injection.
The groups treated with IVTA and IVB consisted of 20 eyes (male eyes, 8; female eyes, 12) and 38 eyes (male eyes, 24; female eyes, 14 eyes), respectively. The mean ages ± SD of the IVTA and IVB groups were 57.1 ± 10.8 years and 59.3 ± 12.1 years, respectively. The differences in mean age, gender ratio, hypertension, HbA1c, baseline BCVA, CMT, and IOP between the two groups were not statistically significant (Table 1).
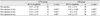
In the IVTA group, BCVA (logMAR) ± SD at pre-injection, 2, 4, and 8 weeks after injection was 0.67 ± 0.40, 0.56 ± 0.35 (p = 0.033), 0.55 ± 0.33 (p = 0.041), and 0.43 ± 0.31 (p = 0.001), respectively. The effects of IVTA on BCVA were consistent throughout the follow-up periods compared with the pre-injection status. In the IVB group, BCVA (logMAR) ± SD at pre-injection, 2, 4, and 8 weeks after injection was 0.51 ± 0.31, 0.42 ± 0.26 (p = 0.003), 0.43 ± 0.32 (p = 0.001), and 0.43 ± 0.27 (p = 0.015), respectively. BCVA at 2, 4, and 8 weeks after injection in the IVB group showed significant improvement compared with the BVCA at pre-injection. The absolute value of BCVA improved more in the IVTA group than it did in the IVB group. BCVA was significantly better in the IVTA group during the follow-up period than it was in the IVB group (p < 0.05) (Table 2).
In the IVTA group, CMT (µm) ± SD values at pre-injection, 2, 4, and 8 weeks after injection was 400.4 ± 94.9, 332.8 ± 47.4 (p = 0.002), 287.5 ± 49.1 (p = 0.007), and 282.5 ± 49.6 (p = 0.043), respectively. In the IVB group, CMT (µm) ± SD values at pre-injection, 2, 4, and 8 weeks after injection was 372.6 ± 99.5, 323.2 ± 72.4 (p = 0.077), 360.9 ± 50.3 (p = 0.668), and 368.2 ± 88.6 (p = 0.830), respectively. The percentages of reduced CMT compared with that at pre-injection in the IVTA group at 2, 4, and 8 weeks after injection were 17.9%, 28.2%, and 29.5%, and those in the IVB group were 13.3%, 3.2%, and 1.2%, respectively. The absolute value of CMT improved more in the IVTA group than it did in the IVB group. The reduction of CMT was statistically significant in the IVTA group throughout the follow-up period, but this was not true in the IVB group. The IVTA group showed a significant reduction in CMT during the follow-up period compared with that in the IVB group (p < 0.05) (Fig. 1).
Increased IOP (mmHg) values due to IVTA at pre-injection, 2, 4, and 8 weeks after injection was 14.9 ± 2.99, 16.4 ± 3.05 (p = 0.086), 16.4 ± 2.03 (p = 0.026), and 18.3 ± 3.95 (p = 0.002), respectively. The IOP (mmHg) of IVB at pre-injection and 2, 4, and 8 weeks after injection was 16.1 ± 3.34, 15.4 ± 2.75 (p = 0.244), 16.0 ± 2.86 (p = 0.896), and 16.4 ± 2.20 (p = 0.596), respectively. In the IVTA group, a significant IOP increase was observed at 4 and 8 weeks after injection compared with the pre-injection level. Additionally, two patients showed an IOP increase requiring reduction treatment at eight weeks after injection which normalized after temporary topical eye drop treatment. However, in the IVB group, there was no significant IOP increase or patient requiring IOP reduction treatment. The IVTA group had a significant IOP increase during the follow-up period compared with that in the IVB group (p < 0.05) (Fig. 2).
Macular edema is the main cause of decreased visual acuity for several diseases. Approximately 10% of all diabetic patients manifest macular edema, with 40% of the patients showing involvement of the center of the macula [16].
Paccola et al. [17] reported that a more favorable BCVA improvement was observed with IVTA compared with that of IVB as early as four weeks after treatment and persisting up to 12 weeks. Similarly, other reports have shown significant visual acuity improvements at the same study points after IVTA [4,7,8]. In the present study, BCVA of the IVTA group improved significantly at 2, 4, and 8 weeks after injection, as in previous reports [4,7,8,17]. The BCVA in the IVB group showed improvement during the eight weeks after injection compared to the pre-injection status. However, BCVA was slightly decreased at four and eight weeks after injection compared with that at two weeks after injection. This BCVA result in the IVB group is more shorter than previous reports [7,18,19].
There are several possible reasons for the reduced effectiveness compared to those of other reports [7,18,19]. In our clinic, IVB injection was performed with the previously multiple-fractionated bevacizumab syringe. The preloaded syringe was stored at 4℃ in the dark. This method was based on a recent study showing that refrigerated bevacizumab can be stored for up to three weeks at 4℃ without loss of efficacy and can remain sterile for up to six months at 4℃ [20-22]. However, in our clinic, after withdrawal of multiple doses from the single-use vial, inadvertent change in the anti-vascular endothelial growth factor (VEGF) antibody concentration or activity may have resulted. This reduction in effective anti-VEGF antibody concentration may have lead to a decreased effect of IVB. Therefore, the BCVA was significantly better in the IVTA group than it was in the IVB group during the follow-up period (p < 0.05). The result from the present study is similar to those of previous reports; the effects of IVTA were more prominent with longer duration compared to those of IVB [17,19].
Paccola et al. [17] reported that a single IVTA had more effect on reduction of CMT in patients with DME compared with one IVB during an eight-week period. Oh et al. [18] also reported that CMT reduction was maintained until three months after IVTA injection, while in the IVB group, CMT reduction was maintained until two months after injection. Massin et al. [6] also demonstrated a significant reduction of CMT for at least three months. In the current study, CMT reduction was significantly maintained until eight weeks after the IVTA injection, while the CMT in the IVB group began to decrease four weeks after IVB injection. This CMT reduction effect in the IVTA group is similar to those in previous reports; however the CMT reduction effect in the IVB group is less prominent with a shorter duration compared to those of previous reports. The reason for the CMT result in the IVB group may be the same reason as that provided for the BCVA result. Furthermore, the CMT reduction effect in the IVB group was statistically insignificant throughout eight weeks after IVB injection, unlike other reports showing statistical significance [17-19].
Previous reports regarding the effects of IVB in DME showed a correlation between BCVA and CMT and statistical significance of recovery of BCVA and CMT [10,11,17-19]. However, in the present study, a correlation between BCVA and CMT was not observed because improvement of BCVA in the IVB group was statistically significant, while CMT reduction was statistically insignificant. Therefore, a further study regarding the reasons for the discordance between BCVA and CMT should be performed.
Possible causes of differences between the IVTA and IVB groups in the duration and effectiveness may include the following: 1) bevacizumab only has an effect on inhibition of VEGF, while 2) triamcinolone acetonide has multiple effects such as inhibiting the expression of both VEGF and the VEGF gene and inhibition of inflammatory cytokines associated with vascular permeability [23]. All of the above-mentioned reasons also may have had an effect on the results of the current study.
The complications of IVTA included IOP elevation, cataract formation or progression, retinal detachment, and endophthalmitis. Among the complications, IOP elevation is the most common [24-27]. Oh et al. [18] reported that five of 40 eyes developed temporary IOP elevation and required temporary treatment. Martidis et al. [4] also reported cataract progression and increased incidence of glaucoma after IVTA. In the current study, two patients in the IVTA group showed IOP increase requiring treatment at eight weeks which normalized after temporary treatment. However, no cataract formation or progression which affected visual acuity was observed in either group during the follow-up period. In the IVB group, there was no significant IOP increase or patient requiring IOP reduction treatment. The difference in IOP increase effect among the two groups was statistically significant during the follow-up period (p < 0.05). Audren et al. [28] reported that, although no remarkable complication due to intravitreal injection was observed during the follow-up period, IVTA has potential side effects including an increase in IOP and cataract development.
Chan et al. [29] reported that, even if the ocular hypertensive effects were similar between the injection types, the cumulative effects of the intraocular steroids would lead to increased cataractogenesis, and each injection exposes the eye to the small but serious risk of infective endophthalmitis. Retrospective reports of IVTA injection indicate a per-injection endophthalmitis risk between 0% and 0.87% [30-33]. Studies regarding the endophthalmitis incidence of IVB reportd a 0.019% to 0.16% incidence after injections [34-37]. Severe complications such as infectious endophthalmitis or retinal detachment were not observed within the follow-up period in either group in the present study.
Consequently, both the IVTA and IVB treatments were effective for recovery of visual loss caused by diabetic retinopathy. However, the effects of IVTA for BCVA were more favorable than those of the IVB and were consistent throughout eight weeks after injection. IVTA significantly reduced the CMT during eight weeks after injection, while IVB did not have a significant impact on CMT during the follow-up period.
Figures and Tables
Fig. 1
Change in central macular thickness (CMT, µm) after intravitreal triamcinolone acetonide (IVTA) and intravitreal bevacizumab (IVB) injections during the follow-up period. In the IVTA group, significant reduction in CMT was observed throughout the follow-up period compared with the pre-injection level (p < 0.05). In the IVB group, reduction of CMT was not statistically significant (p < 0.05). The IVTA group had a significant reduction of CMT during the follow-up period compared with that in the IVB group (p < 0.05).

Fig. 2
Change in intraocular pressure (IOP, mmHg) after intravitreal triamcinolone acetonide (IVTA) and intravitreal bevacizumab (IVB) injections during the follow-up period. In the IVTA group, significant IOP elevation at 4 and 8 weeks after injection was observed compared with the pre-injection level (p < 0.05). In the IVB group, no significant IOP elevation was observed. The IVTA group had a significant increase in IOP during the follow-up period compared with that in the IVB group (p < 0.05).

Table 1
Baseline characteristics
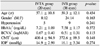
IVTA = intravitreal triamcinolone acetonide; IVB = intravitreal bevacizumab; BCVA = best-corrected visual acuity; logMAR = logarithm of the minimum angle of resolution; CMT = central macular thickness; IOP = intraocular pressure.
*Tested using the chi-square test; †Tested using the Mann-Whitney test.
Acknowledgements
This work was supported by the Institute for Medicine research grant of Kosin University College of Medicine, 2008.
References
1. William EB. Tasman W, Jaeger EA, editors. Diabetic retinopathy. Duane's clinical ophthalmology on CD-ROM. 2004. Philadelphia: Lippincott Williams & Wilkins;Chapter 30.
2. Jonas JB, Sofker A. Intraocular injection of crystalline cortisone as adjunctive treatment of diabetic macular edema. Am J Ophthalmol. 2001. 132:425–427.
3. Audren F, Lecleire-Collet A, Erginay A, et al. Intravitreal triamcinolone acetonide for diffuse diabetic macular edema: phase 2 trial comparing 4 mg vs 2 mg. Am J Ophthalmol. 2006. 142:794–799.
4. Martidis A, Duker JS, Greenberg PB, et al. Intravitreal triamcinolone for refractory diabetic macular edema. Ophthalmology. 2002. 109:920–927.
5. Jonas JB. Intravitreal triamcinolone acetonide for diabetic retinopathy. Dev Ophthalmol. 2007. 39:96–110.
6. Massin P, Audren F, Haouchine B, et al. Intravitreal triamcinolone acetonide for diabetic diffuse macular edema: preliminary results of a prospective controlled trial. Ophthalmology. 2004. 111:218–224.
7. Sutter FK, Simpson JM, Gillies MC. Intravitreal triamcinolone for diabetic macular edema that persists after laser treatment: three-month efficacy and safety results of a prospective, randomized, double-masked, placebo-controlled clinical trial. Ophthalmology. 2004. 111:2044–2049.
8. Bonini-Filho MA, Jorge R, Barbosa JC, et al. Intravitreal injection versus sub-Tenon\'s infusion of triamcinolone acetonide for refractory diabetic macular edema: a randomized clinical trial. Invest Ophthalmol Vis Sci. 2005. 46:3845–3849.
9. Karacorlu M, Ozdemir H, Karacorlu S, et al. Intravitreal triamcinolone as a primary therapy in diabetic macular oedema. Eye (Lond). 2005. 19:382–386.
10. Haritoglou C, Kook D, Neubauer A, et al. Intravitreal bevacizumab (Avastin) therapy for persistent diffuse diabetic macular edema. Retina. 2006. 26:999–1005.
11. Arevalo JF, Fromow-Guerra J, Quiroz-Mercado H, et al. Primary intravitreal bevacizumab (Avastin) for diabetic macular edema: results from the Pan-American Collaborative Retina Study Group at 6-month follow-up. Ophthalmology. 2007. 114:743–750.
12. Cunningham ET Jr, Adamis AP, Altaweel M, et al. A phase II randomized double-masked trial of pegaptanib, an anti-vascular endothelial growth factor aptamer, for diabetic macular edema. Ophthalmology. 2005. 112:1747–1757.
13. Chun DW, Heier JS, Topping TM, et al. A pilot study of multiple intravitreal injections of ranibizumab in patients with center-involving clinically significant diabetic macular edema. Ophthalmology. 2006. 113:1706–1712.
14. Jonas JB, Kreissig I, Sofker A, Degenring RF. Intravitreal injection of triamcinolone for diffuse diabetic macular edema. Arch Ophthalmol. 2003. 121:57–61.
15. Ciardella AP, Klancnik J, Schiff W, et al. Intravitreal triamcinolone for the treatment of refractory diabetic macular oedema with hard exudates: an optical coherence tomography study. Br J Ophthalmol. 2004. 88:1131–1136.
16. Kim HK, Han YB. Laser photocoagulation in diabetic macular edema. J Korean Ophthalmol Soc. 1992. 33:759–763.
17. Paccola L, Costa RA, Folgosa MS, et al. Intravitreal triamcinolone versus bevacizumab for treatment of refractory diabetic macular oedema (IBEME study). Br J Ophthalmol. 2008. 92:76–80.
18. Oh SB, Moon JW, Kim HC. Comparison of effects of intravitreal triamcinolone and bevacizumab in the treatment of diabetic macular edema. J Korean Ophthalmol Soc. 2009. 50:1190–1196.
19. Kim HD, Choi KS, Lee SJ. Combined therapy of intravitreal bevacizumab and posterior subtenon triamcinolone acetonide injection in diabetic macular edema. J Korean Ophthalmol Soc. 2009. 50:1652–1656.
20. Bakri SJ, Snyder MR, Pulido JS, et al. Six-month stability of bevacizumab (Avastin) binding to vascular endothelial growth factor after withdrawal into a syringe and refrigeration or freezing. Retina. 2006. 26:519–522.
21. Ornek K, Karahan ZC, Ergin A, et al. Bevacizumab sterility in multiple doses from a single-use vial. Ann Pharmacother. 2008. 42:1425–1428.
22. Chen YH, Wu PC, Shiea J, et al. Evaluation of the sterility, stability, and efficacy of bevacizumab stored in multiple-dose vials for 6 months. J Ocul Pharmacol Ther. 2009. 25:65–69.
23. Diabetic Retinopathy Clinical Research Network. A randomized trial comparing intravitreal triamcinolone acetonide and focal/grid photocoagulation for diabetic macular edema. Ophthalmology. 2008. 115:1447–1449. 1449.e1–1449.e10.
24. McCuen BW 2nd, Bessler M, Tano Y, et al. The lack of toxicity of intravitreally administered triamcinolone acetonide. Am J Ophthalmol. 1981. 91:785–788.
25. Moshfeghi DM, Kaiser PK, Scott IU, et al. Acute endophthalmitis following intravitreal triamcinolone acetonide injection. Am J Ophthalmol. 2003. 136:791–796.
26. Nelson ML, Tennant MT, Sivalingam A, et al. Infectious and presumed noninfectious endophthalmitis after intravitreal triamcinolone acetonide injection. Retina. 2003. 23:686–691.
27. Roth DB, Chieh J, Spirn MJ, et al. Noninfectious endophthalmitis associated with intravitreal triamcinolone injection. Arch Ophthalmol. 2003. 121:1279–1282.
28. Audren F, Erginay A, Haouchine B, et al. Intravitreal triamcinolone acetonide for diffuse diabetic macular oedema: 6-month results of a prospective controlled trial. Acta Ophthalmol Scand. 2006. 84:624–630.
29. Chan CK, Mohamed S, Shanmugam MP, et al. Decreasing efficacy of repeated intravitreal triamcinolone injections in diabetic macular oedema. Br J Ophthalmol. 2006. 90:1137–1141.
30. Konstantopoulos A, Williams CP, Newsom RS, Luff AJ. Ocular morbidity associated with intravitreal triamcinolone acetonide. Eye (Lond). 2007. 21:317–320.
31. Khairallah M, Zeghidi H, Ladjimi A, et al. Primary intravitreal triamcinolone acetonide for diabetic massive macular hard exudates. Retina. 2005. 25:835–839.
32. Bucher RS, Hall E, Reed DM, et al. Effect of intravitreal triamcinolone acetonide on susceptibility to experimental bacterial endophthalmitis and subsequent response to treatment. Arch Ophthalmol. 2005. 123:649–653.
33. Westfall AC, Osborn A, Kuhl D, et al. Acute endophthalmitis incidence: intravitreal triamcinolone. Arch Ophthalmol. 2005. 123:1075–1077.
34. Wu L, Martinez-Castellanos MA, Quiroz-Mercado H, et al. Twelve-month safety of intravitreal injections of bevacizumab (Avastin): results of the Pan-American Collaborative Retina Study Group (PACORES). Graefes Arch Clin Exp Ophthalmol. 2008. 246:81–87.
35. Fintak DR, Shah GK, Blinder KJ, et al. Incidence of endophthalmitis related to intravitreal injection of bevacizumab and ranibizumab. Retina. 2008. 28:1395–1399.
36. Mason JO 3rd, White MF, Feist RM, et al. Incidence of acute onset endophthalmitis following intravitreal bevacizumab (Avastin) injection. Retina. 2008. 28:564–567.
37. Diago T, McCannel CA, Bakri SJ, et al. Infectious endophthalmitis after intravitreal injection of antiangiogenic agents. Retina. 2009. 29:601–605.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download