Abstract
Purpose
To evaluate factors that can influence the prevalence of amblyopia in children with anisometropia.
Methods
We retrospectively reviewed the records of 63 children 2 to 13 years of age who had anisometropic amblyopia with a difference in the refractive errors between the eyes of at least two diopters (D). The type of anisometropia (myopia, hyperopia, and astigmatism), degree of anisometropia (<2-3 D, <3-4 D, or >4 D), best corrected visual acuity (BCVA) of the amblyopic eye at the time of initial examination, BCVA differences between sound and amblyopic eyes, whether or not occlusion therapy was performed, compliance with occlusion therapy, and the patient's age when eyeglasses were first worn were investigated.
Results
There was an increase in the risk of amblyopia with increased magnitude of anisometropia (p=0.021). The prevalence of amblyopia was higher in the BCVA <20/40 group and in patients with BCVA differences >4 lines between sound and amblyopic eyes (p=0.008 and p=0.045, respectively). There was no statistical relationship between the prevalence of amblyopia and the type of anisometropia or the age when eyeglasses were first worn. Poor compliance with occlusion therapy was less likely to achieve successful outcome (p=0.015).
Amblyopia is a disorder of the visual system that is characterized by a decrease in the best corrected visual acuity (BCVA) in an eye with no organic pathology [1]. Anisometropia is a well-known cause of amblyopia [2]. Unequal refractive error between the two eyes produces abnormal binocular interaction and/or visual deprivation. Patients with anisometropic amblyopia usually have no identifiable ocular defects and the visual acuity of the sound eye is normal, which makes it difficult to diagnose the symptoms, and thus early treatment is often delayed. Because improvement in visual acuity with amblyopia treatment depends on the age at which treatment begins, earlier detection of children with anisometropic amblyopia is desired [3-6].
According to Weakley [7,8], there is an increased risk of amblyopia with myopic anisometropia >2 diopters (D), hyperopic anisometropia >1 D, and astigmatic anisometropia >1.5 D. Hussein et al. [9], in a study of amblyopic children older than six years of age, found that the risk factors for anisometropic amblyopia treatment failure were age >6 years at the onset of treatment, the presence of astigmatism of >1.5 D in the amblyopic eye, poor compliance with treatment, and initial visual acuity in the amblyopic eye of ≤20/200.
The aim of this study was to determine and analyze factors early in the course of treatment that influence the prevalence of amblyopia in children with anisometropia.
Between January 2000 and December 2007, we retrospectively reviewed the records of 63 children 2 to 13 years of age who had anisometropia with a difference in the refractive power between the eyes of at least 2 D. Patients with at least six months of follow-up were included in the study. Visual acuity was measured at a 4 m distance using an international standard vision chart (Jin's vision chart), and amblyopia was defined as a BCVA difference between the sound and amblyopic eyes of more than two lines on the vision chart. Any patient with structural ocular abnormalities, including strabismus, history of spectacle correction, occlusion or penalization therapy, previous ocular surgery, ocular trauma, or neurologic disorders which could influence visual acuity, or with BCVA of the sound eye <20/40 was excluded from the research. Each patient's age at diagnosis, uncorrected visual acuity and BCVA, and examination of the external eye and fundus were studied. Cycloplegic refraction was performed after application of 1% cyclopentolate eye drops. Eyeglasses were prescribed based on the results of cycloplegic refraction.
The prevalence of amblyopia at the final visit was analyzed by studying the type of anisometropia (myopia, hypermetropia, and astigmatism), magnitude of anisometropia, BCVA at the start of treatment (≥20/40 or <20/40), BCVA differences between the sound and amblyopic eyes (≥4 lines or <4 lines), and the age at which eyeglasses were first worn (<5 years of age or ≥5 years of age). Anisometropia was divided into the following two groups: spherical anisometropia, in which the difference in the spherical equivalent between the eye was >2 D, while the cylinder power difference was <2 D, and cylindrical anisometropia, which had a >2 D cylindrical power difference. The magnitude of anisometropia was graded into an arbitrary three-category classification (Group 1, 2 to <3 D; Group 2, 3 to <4 D; Group 3, ≥4 D).
Full spherical and astigmatic refractive errors were corrected in each patient, and, depending on the visual improvement at the second visit (≥2 lines difference between sound and amblyopic eyes persisted), the patient was required to patch the sound eye for 4 to 6 hours per day. The compliance with patching treatment was divided into the following two groups based on the parents' estimate: children with good compliance who followed the treatment guideline an estimated ≥75% of the time, and poor compliance (<75% of the time).
A chi-square test and t-test were conducted for statistical analysis using SPSS ver. 15.0 (SPSS Inc., Chicago, IL, USA), and a p<0.05 was considered to be statistically significant.
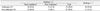
The mean age at the start of treatment was 5.9±3.9 years. Thirty-three patients (52.3%) were male and 30 patients (47.7%) were female. The follow-up period averaged 57.2±38.0 months, with a maximum of 147 months. Forty-one patients were diagnosed with spherical anisometropia, 18 were diagnosed with myopic spherical anisometropia, and 13 (72.2%) patients had amblyopia. Twelve of 23 (52.1%) patients with hypermetropic spherical anisometropia also had amblyopia, and eight of 22 (36.4%) astigmatic anisometropia patients had amblyopia. There were no frequency differences according to the type of anisometropia (myopic spherical anisometropia, hyperopic spherical anisometropia, and astigmatic anisometropia; p=0.770) (Table 1).
Nine (39.1%) of 23 patients in Group 1 (≥2 D, <3 D), 12 (52.1%) of 23 patients in Group 2 (≥3 D, <4 D), and 12 (70.6%) of 17 patients in Group 3 (≥4 D) had amblyopia. In general, children with higher magnitudes of anisometropia had a higher prevalence of amblyopia (p=0.021) (Table 2).
Twenty-seven patients had an initial BCVA of <20/40, 17 (63.0%) of which had amblyopia. Sixteen of 36 (44.4%) patients with BCVA ≥20/40 had amblyopia. There were differences among the statistical frequencies of amblyopia between the two groups (p=0.008), and an initial BCVA <20/40 in the amblyopic eye was a risk factor for the development of amblyopia. Among 18 patients <5 years of age at the initial visit, 12 had an initial BCVA of <20/40, and seven (58.3%) of these 12 patients had amblyopia. Of the six patients whose initial BCVA ≥20/40, one (16.7%) had amblyopia. Forty-five patients were ≥5 years of age at initial presentation. Fifteen patients had an initial BCVA of <20/40 and ten (66.7%) of these patients had amblyopia. Fifteen of 30 (50.0%) patients whose initial BCVA ≥20/40 had amblyopia. Given an initial BCVA <20/40, the risk of amblyopia at the final visit was not significantly different between the initial presentation groups with respect to age (p=0.656).
Eighteen patients were <5 years of age at the time of the initial spectacle correction and nine (50.0%) had amblyopia, while 24 (53.3%) of 45 patients ≥5 years of age had amblyopia. There was no statistical significance regarding the prevalence of amblyopia between patients <5 and ≥5 years of age at the time of initial spectacle correction (p=0.811).
Forty-six patients underwent patching therapy, and the mean duration of patching therapy was 22.2±17.9 months. Twenty-three (50.0%) of 46 patients who were treated with patching therapy had amblyopia, and ten (58.8%) of 17 patients without patching treatment had amblyopia. Good compliance with patching occurred in 25 patients, ten (40.0%) of whom had amblyopia. Of the 21 patients with poor compliance, 13 (61.9%) had amblyopia. Poor compliance with patching was a risk factor for amblyopia (p=0.027), while no differences existed in patients who were or were not treated with patching therapy (p=0.534) (Table 3).
Among the patients with good compliance to patching therapy, 11 had <4 lines of difference in the BCVA between the sound and amblyopic eyes at the initial presentation, and two (18.2%) patients had amblyopia at the final visit. Eight (57.1%) of 14 patients who had ≥4 lines of difference in the BCVA between the eyes at the initial visit presented with amblyopia at the final visit. A difference in the BCVA between the sound and amblyopic eyes ≥4 lines was a risk factor for the development of amblyopia in patients with good compliance to patching therapy (p=0.045) (Table 4).
Amblyopia is one of the leading causes of acquired monocular visual impairment [10], with an estimated prevalence in the pediatric population ranging from 4.7% to 7.5% [11]. Children with anisometropic amblyopia typically are diagnosed later than are children having other types of amblyopia, likely reflecting the lack of noticeable physical abnormalities in these children, in contrast to children with strabismus, who usually have an obvious condition that is easily recognized [3-5]. With respect to the magnitudes of anisometropia, Leon et al. [12] demonstrated that children with higher magnitudes of anisometropia had a higher prevalence and greater depths of amblyopia. However, Hussein et al. [9] concluded that the type, amount of refractive error, and the difference in refractive power between the eyes were significant risk factors for treatment failure. In the current study, children with higher magnitudes of anisometropia had a higher prevalence of amblyopia.
It is known that amblyopia is more severe and more frequent in hypermetropic anisometropia than it is myopic anisometropia [13]. In a study by Weakley [8], there was a tendency for the development of amblyopia at lower levels of hyperopic anisometropia (spherical hypermetropic anisometropia >1-2 D) compared to that with myopic anisometropia (spherical myopic anisometropia >-2 to -3 D). However, in patients with equal levels of spherical myopic anisometropia and spherical hypermetropic anisometropia >2 D, both the incidence and severity of amblyopia were remarkably similar. Kim et al. [14] reported that there is no significant difference in the frequencies of amblyopia between spherical and cylindrical anisometropia patients; however, in spherical anisometropia, hyperopic anisometropia patients have a higher risk for developing amblyopia. However, in this study, there were no differences in the frequency of amblyopia development among patients having myopic spherical anisometropia, hypermetropic spherical anisometropia, or astigmatic anisometropia. The lack of statistical significance for this comparison was probably due to the relatively higher magnitude of anisometropia in the myopia anisometropia group than in the other groups, and the small numbers in each group of this study.
Several studies have suggested that that the factors influencing outcomes of amblyopia are the initial age of treatment and the BCVA of the weaker eye at the time of the initial treatment. According to Kim et al. [15], in a study involving 66 amblyopic children, the duration of treatment was longer in children with an initially poorer BCVA and in younger children compared to that in older children with better BCVAs at the time of diagnosis. Chen et al. [16] reported that, of 60 anisometropic amblyopic children with spectacle correction alone, the resolution of amblyopia was related to better initial visual acuity and lesser degrees of anisometropia. Hussein et al. [9] found that an initial visual acuity in the amblyopic eye of 20/200 or worse was a risk factor of treatment failure, and patients with very poor vision in the amblyopic eye can have significant improvement in vision, but may not achieve a final vision of 20/40 or better. In the current study, the frequency of amblyopia development was higher in children with an initial visual acuity <20/40 than it was in children with an initial visual acuity of ≥20/40. This result suggests that, under conditions of high dependence on the sound eye, abnormal binocular interaction and/or visual deprivation resulted.
Older children with amblyopia generally respond less favorably to treatment [1]. Hussein et al. [9] demonstrated that age greater than six years at the onset of treatment was a risk factor for failure to achieve functional success. According to Leon et al. [12], children age three and older had an increased risk of amblyopia compared with that of younger children for moderate (≥4, <6 line difference) levels of anisometropia. However, Woodruff et al. [4] could not find a correlation between unfavorable amblyopia treatment outcome and age at initiation of treatment. Rho et al. [17] also could not document a statistical significance between age at initial treatment and treatment outcome. In the current study, there was no statistical significance of amblyopia prevalence in patients <5 year of age at the time of initial spectacle correction. We also found that there was no significant difference of amblyopia risk between the <5 year of age group and ≥5 year of age group among patients with an initial BCVA <20/40. Such a discrepancy between studies indicates the need for more research to determine whether age at initial treatment affects treatment outcome.
Previous studies have demonstrated that poor patching compliance was associated with a poor outcome. Hussein et al. [9] demonstrated inadequate compliance with treatment according to parental report at the first follow-up examination was a key predictive factor for failure risk. Choi and Kim [18] have demonstrated a relationship between anisometropic amblyopia and occlusion therapy when the treatment age was younger and the compliance rate was higher in the success group compared with those of the failure group. In the current study, patching therapy and the amblyopia prevalence had no significant relationship; however, poor compliance with patching was a risk factor for the prevalence of amblyopia.
A difference in the BCVA between the eyes is related to treatment outcome in amblyopia. Lee et al. [19], in a study of 80 patients with strabismic amblyopia and anisometropic amblyopia, demonstrated that patients with ≤4 lines of difference in the BCVA between the sound and amblyopic eyes at the initial visit had a high success rate with patching therapy. Although strabismic amblyopia was excluded from our study, we also found that BCVA differences between sound and amblyopic eyes of ≥4 lines was a risk factor for the development of amblyopia in patients having undergone patching therapy.
Regarding the limitations of the current study, there was a relatively small number of patients and lacks of standardization in the age groups and treatment method. A large prospective study is thus required to establish more statistically powerful results.
In conclusion, eyes with an initial visual acuity of <20/40, a high magnitude of anisometropia, and a ≥4 line difference in BCVA between the sound and amblyopic eyes were less likely to achieve successful outcomes. Therefore, such children must receive careful treatment. In addition, parents and guardians must be fully aware of the risk through sufficient explanation, regular observation, and amblyopia treatment.
Figures and Tables
Notes
References
1. von Noorden GK, Campos EC, editors. Binocular vision and ocular motility: theory and management of strabismus. 2001. 6th ed. St. Louis: Mosby;246–247.
2. Sjostrand J, Abrahamsson M. Risk factors in amblyopia. Eye (Lond). 1990. 4:787–793.
3. Shaw DE, Fielder AR, Minshull C, Rosenthal AR. Amblyopia: factors influencing age of presentation. Lancet. 1988. 2:207–209.
4. Woodruff G, Hiscox F, Thompson JR, Smith LK. The presentation of children with amblyopia. Eye (Lond). 1994. 8:623–626.
5. Chua BE, Johnson K, Martin F. A retrospective review of the associations between amblyopia type, patient age, treatment compliance and referral patterns. Clin Experiment Ophthalmol. 2004. 32:175–179.
6. Scheiman MM, Hertle RW, Beck RW, et al. Randomized trial of treatment of amblyopia in children aged 7 to 17 years. Arch Ophthalmol. 2005. 123:437–447.
7. Weakley DR. The association between anisometropia, amblyopia, and binocularity in the absence of strabismus. Trans Am Ophthalmol Soc. 1999. 97:987–1021.
8. Weakley DR Jr. The association between nonstrabismic anisometropia, amblyopia, and subnormal binocularity. Ophthalmology. 2001. 108:163–171.
9. Hussein MA, Coats DK, Muthialu A, et al. Risk factors for treatment failure of anisometropic amblyopia. J AAPOS. 2004. 8:429–434.
10. Attebo K, Mitchell P, Cumming R, et al. Prevalence and causes of amblyopia in an adult population. Ophthalmology. 1998. 105:154–159.
11. de Vries J. Anisometropia in children: analysis of a hospital population. Br J Ophthalmol. 1985. 69:504–507.
12. Leon A, Donahue SP, Morrison DG, et al. The age-dependent effect of anisometropia magnitude on anisometropic amblyopia severity. J AAPOS. 2008. 12:150–156.
13. McMullen WH. Some points in anisometropia in discussion on problem in refraction. Trans Ophthalmol Soc UK. 1939. 59:119.
14. Kim JB, Moon CS, Chang YH, et al. The amblyopia and strabismus accompanied with anisometropia. J Korean Ophthalmol Soc. 2007. 48:411–417.
15. Kim EK, Choi MY, Kim YH. Clinical analysis of successfully treated amblyopia with anisometropia, strabismis, and combined cause. J Korean Ophthalmol Soc. 2008. 49:303–308.
16. Chen P, Chen J, Tai M, et al. Anisometropic amblyopia treated with spectacle correction alone: possible factors predicting success and time to start patching. Am J Opthalmol. 2007. 143:54–60.
17. Rho SS, Yang HS, Chang YH, et al. The effect on outcome of amblyopia treatment in children with anisometropic amblyopia. J Korean Ophthalmol Soc. 2007. 48:535–540.
18. Choi MY, Kim YH. Clinical analysis of anisometropic amblyopia with monocular vision 0.1 or worse. J Korean Ophthalmol Soc. 2008. 49:973–978.
19. Lee CS, Shin MK, Paik HJ. Evaluation of factors affecting the outcome of occlusion treatment for amblyopia. J Korean Ophthalmol Soc. 2001. 42:1740–1746.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download