Abstract
Purpose
To evaluate the long-term efficacy and rotational stability of the AcrySof toric intraocular lens (IOL) in correcting preoperative astigmatism in cataract patients.
Methods
This prospective observational study included 30 eyes from 24 consecutive patients who underwent implantation of an AcrySof toric IOL with micro-coaxial cataract surgery between May 2008 and September 2008. Outcomes of visual acuity, refractive and keratometric astigmatism, and IOL rotation after 1 day, 1 month, 3 months, and long-term (mean, 13.3±5.0 months) follow-up were evaluated.
Results
At final follow-up, 73.3% of eyes showed an uncorrected visual acuity of 20/25 or better. The postoperative keratometric value was not different from the preoperative value; mean refractive astigmatism was reduced to -0.28±0.38 diopter (D) from -1.28±0.48 D. The mean rotation of the toric IOL was 3.45±3.39 degrees at final follow-up. One eye (3.3%) exhibited IOL rotation of 10.3 degrees, the remaining eyes (96.7%) had IOL rotation of less than 10 degrees.
Given that cataract surgery has become a refractive procedure, emmetropia is now the expected outcome of both the surgeon and most patients. Approximately 20% of patients having routine cataract surgery have visually significant corneal astigmatism [1]. To achieve emmetropia, these patients may have combined corneal refractive surgery and spherical intraocular lens (IOL) implantation or toric IOL implantation alone.
The toric IOL was devised by Shimizu et al. [2] in 1994 and has been used clinically since then. Several studies have analyzed the results of implantation of many models of toric IOLs and have found this method to be effective in correcting astigmatism [3-10].
The AcrySof toric series of IOLs (Alcon Laboratories, Fort Worth, TX, USA) is made of hydrophobic acrylate and shares the same biconvex single-piece design as the AcrySof SA60AT monofocal IOL (Alcon Laboratories). The toric IOL differs in that there is a toric component located on the posterior surface of the lens optic. The optic is marked with 3 peripheral dots that indicate the cylindrical axis of the lens and thus enable its correct alignment with the steepest axis of corneal astigmatism during surgery. The AcrySof toric IOL is available in 3 types: SA60T3, SA60T4, and SA60T5 with cylinder powers at the IOL plane (corneal plane) of 1.50 diopter (D) (1.03 D), 2.25 D (1.55 D), and 3.00 D (2.06 D), respectively.
The success of a toric IOL can be judged not only by its ability to reduce refractive astigmatism immediately postoperatively, but also by its ability to maintain a stable position in the capsular bag over the long-term. However, many surgeons have stopped using toric IOLs because of reported positional instability [11]. The most frequent cause of IOL rotation following uncomplicated cataract surgery is capsular bag shrinkage due to fibrosis [12]. The majority of this occurs within the first three months after implantation [13]. Even a small rotational deviation of the toric IOL from its intended axis can result in a large reduction of the astigmatic correction [14]. For example, a deviation of 10 degrees minimizes the potential correction by 35%.
Previous studies have examined the visual outcomes over a short period (3 to 6 months); however, to our knowledge no long-term studies regarding this type of IOL are available. The aim of this study was to assess the astigmatic reduction and rotational stability in the early postoperative period and at long-term follow-up of the AcrySof toric IOL in a series of cataract surgery patients with corneal astigmatism greater than 1.0 D.
This prospective observational study included 30 eyes from 24 consecutive patients with cataracts and preexisting regular corneal astigmatism of greater than 1.0 D who underwent implantation of an AcrySof toric IOL from May 2008 to September 2008. Preoperatively, patients had a complete ophthalmologic examination including measurement of uncorrected visual acuity (UCVA) and best spectacle-corrected visual acuity (BCVA), manifest refraction, autorefractometry (ARK-30; Nidek Co. Ltd., Gamagori, Japan), slitlamp examination, fundoscopy, keratometry, and topography (Orbscan II; Bausch & Lomb, TX, USA and Pentacam; Oculus, Wetzlar, Germany). Exclusion criteria included a history of glaucoma or retinal detachment, corneal disease, previous corneal or intraocular surgery, abnormal iris, pupil deformation, macular degeneration or retinopathy, and evidence of previous uveitis.
Biometry was performed with optical coherence biometry (IOL master; Carl Zeiss Meditec, Jena, Germany) using the SRK-T formula for the IOL power calculation and the A-constant of 118.7 for the toric IOL. Data for IOL calculation were taken from direct use of the IOL master. The target postoperative spherical equivalent was emmetropia. Intraocular lens cylinder power and alignment axis were calculated using a program available from the IOL manufacturer (www.acrysoftoriccalculator.com), taking into account the IOL master keratometry readings as well as mandatory data input on the position of the incision and the estimate of surgically induced astigmatism from the temporal incision (0.3 D for ESC, 0.5 D for TYC).
Preoperatively, with the patient sitting upright the toric reference corneal marker (AE-2793S; ASICO, Westmont, IL, USA) was used to place 3 limbal reference marks at the 3, 6, and 9 o'clock positions to correct for recumbent cyclotorsion. Intraoperatively, the actual implantation axis was marked using a Mendez ring and a toric axis marker (AE-2740; ASICO). Cataract surgery was performed by one of 2 experienced surgeons (ESC and TYC) under topical anesthesia. Each patient underwent microincision cataract surgery using the Infinity Vision System® and OzilTM Torsional Handpiece (Alcon Laboratories) with a 2.2 mm temporal clear corneal incision. The toric IOL was implanted into the capsular bag with a Monarch injector and a D-Cartridge (Alcon Laboratories). The IOL was rotated to its final position by exactly aligning the toric reference marks with the limbal implantation axis marks. Postoperatively, prednisolone eyedrops and levofloxaxcin eyedrops were used 4 times a day for 1 week and then tapered over 3 weeks or as clinically indicated.
Follow-up examinations were performed postoperatively at 1 day, 1 month, 3 months, and every 6 months thereafter. On each occasion, all patients underwent UCVA, BCVA, manual refraction, autorefractometry, and slit lamp examination. As part of the regular postoperative follow-up, digital retroilluminated slitlamp photographs were taken of each eye at every visit. Before slit lamp photography, eyes were dilated to a pupil diameter of at least 6.5 mm with a drop of 0.5% tropicamide and 0.5% phenylephrine mixed eye drops. Rotation was assessed by digital image analysis using the software program ImageJ (available at: http://rsb.info.nih.gov/ij/) distributed by the National Institutes of Health.
Statistical analysis was performed using Stata ver. 10 (StataCorp LP, College Station, TX, USA). The t-test was used for comparative statistics. Differences were considered statistically significant when the p-value was less than 0.05.
Thirty eyes from 24 consecutive patients were enrolled in this study. Table 1 shows the patients' demographics. The mean age was 55.8±16.2 years and the mean follow-up period was 13.3±5.0 months. The mean preoperative sphere and preoperative cylinder measured by autorefractometry was -1.88±3.58 D and -1.28±0.48 D, respectively. The mean keratometric cylinder was -1.57±0.51 D by manual keratometer. The keratometric cylinder measured by optical coherence biometry and corneal topography was -1.63±0.43 D and -1.67±0.60 D, respectively. There was no statistical difference of keratometric cylinder among the 3 methods.
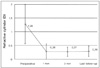
Fig. 1 shows the mean visual results at the early and final follow-up visits. At the last visit, the mean logarithm of the minimum angle of resolution (logMAR) UCVA was 0.33±0.18. The BCVA improved slightly to 0.10±0.05 logMAR.
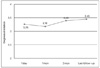
There was significant reduction in refractive astigmatism after toric IOL implantation (p<0.05) (Fig. 2). The mean reduction was 1.01±0.40 D. At final follow-up, the mean refractive cylinder was -0.28±0.38 D. All eyes had less than 1.0 D of cylinder and 86.7% were within 0.5 D after 1 year (Fig. 3). The mean change in keratometric astigmatism was 0.18±0.39 D and the corneal astigmatism did not significantly change following surgery (p=0.360).
The mean absolute toric IOL axis rotation was 3.45±3.39 degrees (range, 0 to 10.3 degrees) at final follow-up at 13.3±5.0 months. One eye (3.3%) had IOL rotation of 10.3 degrees, the remaining eyes (96.7%) had rotations of less than 10 degrees. Twelve (40%) IOLs rotated clockwise with a maximum rotation of 10.3 degrees, 10 (33.3%) IOLs rotated counterclockwise with a maximum rotation of 8.9 degrees, and 8 (26.7%) IOLs did not rotate (Fig. 4). The mean absolute rotation of the toric IOL was 3.26±3.54 degrees at 1 day postoperatively, 3.18±3.28 degrees at 1 month postoperatively, and 3.40±3.05 degrees at 3 months postoperatively (Fig. 5). Between day 1 and 3 months, the overall mean absolute rotation of all 30 implanted IOLs was 0.71±0.84 (range, 0 to 2.1) degrees. Between 3 months postoperatively and final follow-up (of 13.3±5.0 months) the mean absolute rotation was 3.46±3.39 degrees. There was no statistically significant rotation between early follow-up (1 month and 3 months) and final follow-up (p=0.215, p=0.492, respectively).
No complications were encountered during the intra- and postoperative courses. None of the lenses required secondary alignment.
Corneal astigmatism can be surgically managed using corneal, relaxing, or limbal incisions and excimer laser keratectomy. All these methods have limitations, including the degree of astigmatism that can be treated and long-term mechanical instability [15]. In addition, postoperative outcomes are subject to many other variables such as age, magnitude, and incision number, depth, and length. The use of toric IOLs to correct corneal astigmatism is one surgical option, and implantation of a toric IOL is one way to manage astigmatism in patients with cataract and corneal astigmatism.
It is important to obtain accurate corneal astigmatism measurements to determine the actual amount of cylinder requiring correction and the appropriate spherical power for the IOL. In the AcrySof clinical trial [16], manual keratometry was mandatory to measure corneal astigmatism. In our study, we used 3 different methods: manual keratometry, optical coherence biometry, and corneal topography; all 3 methods yielded comparable results. In addition, the IOL cylinder power and alignment axis calculated with the keratometric cylinder value from the three methods were not different. The p-values were 0.375 (manual keratometry and optical coherence biometry), 0.236 (manual keratometry and topography), and 0.485 (optical coherence biometry and topography). The difference in the alignment axis was 5.14±5.03 degrees, this was calculated by manual keratometry and optical coherence biometry. The difference between manual keratometry and corneal topography was 9.42±11.76 degrees. The result from optical coherence biometry and corneal topography yielded 10.24±13.33 degrees of difference. Although we primarily used data from the IOL master to calculate the IOL power, we believe that any method could be appropriate for measuring the amount and axis of astigmatism depending on the clinical settings.
The major requirement for toric IOLs is rotational stability. The magnitude of cylinder corrected is inversely proportional to the degree of axis misalignment between 0 degrees and 30 degrees. It has been estimated that approximately 1 degree of off-axis IOL rotation results in a loss of up to 3.3% of IOL cylinder power. Complete loss of cylinder power occurs when the IOL is misaligned by more than 30 degrees [17]. Earlier models of toric IOLs were restricted by considerable amounts of postoperative rotation and the need for additional surgical procedures to realign the IOL; IOL design has been shown to play a significant role in rotational stability [5,10,18]. Weinand et al. [19] found excellent rotational stability for the single-piece AcrySof SA60AT IOL, which utilizes a design similar to the toric IOL we used. The mean postoperative rotation was 0.7 degrees (range, 0.1 to 1.8 degrees) in 17 patients. Since then few studies have actually used the AcrySof toric IOL. Zuberbuhler et al. [20] reported in a series of 44 AcrySof toric IOLs that the postoperative rotation was within 5 degrees in 95% of cases and within 2 degrees in 68% of eyes after 3 months postoperatively. In 30 eyes, Mendicute et al. [21] demonstrated a mean toric IOL axis rotation of 3.63±3.11 degrees, with rotation less than 10 degrees in 96.7% of eyes using the AcrySof toric IOL. In our study, the mean axis rotation was 3.40±3.05 degrees at 3 months postoperatively. Our early follow-up results are in accordance with the previous literature, implying that the AcrySof toric IOL has good rotational stability during the early follow-up period. In addition, after longer follow-up of more than 1 year, the mean rotation of the IOL was 3.45±3.39 degrees and was not significantly different from early follow-up results. The largest rotation was 10.3 degrees and was seen in only one eye. No specific cause was identified for this large deviation and the patient did not require secondary repositioning of the lens because of visual satisfaction.
The mean rotation of the toric IOLs was 3.26±3.54 degrees at 1 day postoperatively, 3.40±3.05 degrees at 3 months postoperatively, and 3.45±3.39 degrees at final follow-up. Most IOL rotation happened in the early postoperative period. Once the anterior and posterior capsules fuse, IOL rotation was less frequent at long-term follow-up (mean, 13.3±5.0 months). Possible factors influencing the capsule fusion and resultant IOL stability include capsulorhexis size and IOL design and material. Ruhswurm et al. [5] found IOL rotation to be associated with increasing capsular bag diameter as well as with axial length. The initial IOL position could affect how gravity influences early rotation. To evaluate multiple possible factors on IOL rotation, further prospective comparative study is warranted.
In our study, 93.3% of eyes showed 20/40 or better UCVA and 73.3% of eyes showed 20/25 or better UCVA at final follow-up at a mean of 13.3 months. This compares favorably with results in the initial FDA clinical trial in which approximately 66% of patients with unilateral implantation of the toric IOL achieved a UCVA of 20/25 or better and 41% of the unilateral control subjects achieved a UCVA of 20/25 or better in 6-month data [11]. The FDA trial was originally designed to follow for 1 year, but only 6 months of data are available. In another study of the AcrySof toric IOL without a control group by Mendicute et al. [21], 66.6% of eyes achieved 20/25 or better and 93.3% of eyes achieved 20/40 or better UCVA at 3 months postoperatively. Some studies [20-22] demonstrated good short-term results, but as far as we know ours is the first study which showed the long-term efficacy of the AcrySof toric IOL past 1 year.
Eyes in our study had an 85.6% reduction in astigmatism after AcrySof toric IOL implantation. All eyes were within 1.0 D and 86.7% were within 0.5 D. Mendicute et al. [21] reported a reduction in astigmatism of 70% after AcrySof toric IOL implantation. A study by Sun et al. [6] showed a reduction in astigmatism of approximately 54% after Staar TF IOL implantation. Till et al. [8] found a higher percentage of reduction (81%) after Staar TF or TL IOL implantation. De Silva et al. [10] reported a reduction in astigmatism of 65% after MicroSil 6116TU (HumanOptics, Erlangen, Germany) toric IOL implantation. Differences between IOL models and preoperative astigmatism values are responsible for the variability in the percentage of astigmatism reduction and visual acuity outcomes between toric IOLs.
Selection of the appropriate toric IOL is made using a manufacturer IOL program that works on the basis of preoperative corneal astigmatism for the power and axis parameters. Keratometric corneal cylinder, measured by the IOL master in this study, is used to calculate the required IOL cylinder. Therefore, toric IOL implantation should be performed through small incisions to achieve expected outcomes based on keratometric values. In previous studies of the AcrySof toric IOL, the incision size for cataract surgery has ranged from 2.75 to 3.0 mm. In our study, microincision cataract surgery with a 2.2 mm clear corneal incision was performed. The outcome was favorable as in other studies and no complications related to the microincision cataract surgery were observed. Thus, surgeons may consider a combination of microincision cataract surgery and toric IOL implantation to correct astigmatism in cataract patients.
In conclusion, the results from our study show that microincision cataract surgery with implantation of the AcrySof toric IOL is a safe, predictable, and effective surgical option for correcting preexisting astigmatism during cataract surgery. The AcrySof toric IOL demonstrated no significant rotation during the long-term follow-up period of over a year. The toric IOL will play an increasingly important role in the future. Decreasing spectacle dependence improves patient quality of life and should be pursued. Thus, prospective comparative study with larger samples should continue to evaluate the efficacy of allowing spectacle independence.
Figures and Tables
 | Fig. 1Visual outcomes. Both postoperative uncorrected visual acuity (UCVA) and best spectacle-corrected visual acuity (BCVA) were significantly improved when compared with preoperative values (p<0.05) (mean final follow-up, 13.3±5.0 months). LogMAR=logarithm of the minimum angle of resolution. |
 | Fig. 2Refractive outcome. Mean refractive cylinder significantly improved compared to preoperative values during all follow-up periods (mean final follow-up, 13.3±5.0 months). D=diopter. |
References
1. Hoffer KJ. Biometry of 7,500 cataractous eyes. Am J Ophthalmol. 1980. 90:360–368.
2. Shimizu K, Misawa A, Suzuki Y. Toric intraocular lenses: correcting astigmatism while controlling axis shift. J Cataract Refract Surg. 1994. 20:523–526.
3. Grabow HB. Early results of 500 cases of no-stitch cataract surgery. J Cataract Refract Surg. 1991. 17:Suppl. 726–730.
4. Werblin TP. Do three-piece PMMA IOLs rotate after implantation in the capsular bag? J Refract Surg. 1995. 11:468–471.
5. Ruhswurm I, Scholz U, Zehetmayer M, et al. Astigmatism correction with a foldable toric intraocular lens in cataract patients. J Cataract Refract Surg. 2000. 26:1022–1027.
6. Sun XY, Vicary D, Montgomery P, Griffiths M. Toric intraocular lenses for correcting astigmatism in 130 eyes. Ophthalmology. 2000. 107:1776–1781.
7. Leyland M, Zinicola E, Bloom P, Lee N. Prospective evaluation of a plate haptic toric intraocular lens. Eye (Lond). 2001. 15:202–205.
8. Till JS, Yoder PR Jr, Wilcox TK, Spielman JL. Toric intraocular lens implantation: 100 consecutive cases. J Cataract Refract Surg. 2002. 28:295–301.
9. Chang DF. Early rotational stability of the longer Staar toric intraocular lens: fifty consecutive cases. J Cataract Refract Surg. 2003. 29:935–940.
10. De Silva DJ, Ramkissoon YD, Bloom PA. Evaluation of a toric intraocular lens with a Z-haptic. J Cataract Refract Surg. 2006. 32:1492–1498.
11. Horn JD. Status of toric intraocular lenses. Curr Opin Ophthalmol. 2007. 18:58–61.
12. Ohmi S. Decentration associated with asymmetric capsular shrinkage and intraocular lens size. J Cataract Refract Surg. 1993. 19:640–643.
13. Strenn K, Menapace R, Vass C. Capsular bag shrinkage after implantation of an open-loop silicone lens and a poly (methyl methacrylate) capsule tension ring. J Cataract Refract Surg. 1997. 23:1543–1547.
14. Sanders DR, Grabow HB, Shepherd J. Grills JP, Martin RG, Sanders DR, editors. The toric IOL. Sutureless cataract surgery: an evolution toward minimally invasive technique. 1992. Thorofare: Slack, Inc.;183–197.
15. Husain SE, Kohnen T, Maturi R, et al. Computerized videokeratography and keratometry in determining intraocular lens calculations. J Cataract Refract Surg. 1996. 22:362–366.
16. Grabow HB. Kershner RM, editor. Intraocular correction of refractive errors. Refractive keratectomy for cataract surgery and the correction of astigmatism. 1994. Thorofare: Slack, Inc.;79–115.
17. Novis C. Astigmatism and toric intraocular lenses. Curr Opin Ophthalmol. 2000. 11:47–50.
18. Patel CK, Ormonde S, Rosen PH, Bron AJ. Postoperative intraocular lens rotation: a randomized comparison of plate and loop haptic implants. Ophthalmology. 1999. 106:2190–2195.
19. Weinand F, Jung A, Stein A, et al. Rotational stability of a single-piece hydrophobic acrylic intraocular lens: new method for high-precision rotation control. J Cataract Refract Surg. 2007. 33:800–803.
20. Zuberbuhler B, Signer T, Gale R, Haefliger E. Rotational stability of the AcrySof SA60TT toric intraocular lenses: a cohort study. BMC Ophthalmol. 2008. 8:8.
21. Mendicute J, Irigoyen C, Aramberri J, et al. Foldable toric intraocular lens for astigmatism correction in cataract patients. J Cataract Refract Surg. 2008. 34:601–607.
22. Na JH, Lee HS, Joo CK. The clinical result of acrySof toric intraocular lens implantation. J Korean Ophthalmol Soc. 2009. 50:831–838.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download