Abstract
Purpose
To investigate the effects of brimonidine, an α-2-adrenergic agonist, on barrier function in ARPE-19 cells by measuring transepithelial resistance (TER).
Methods
ARPE-19 cells were cultured into a confluent monolayer on a microporous filter. Brimonidine was added to the apical medium, and the barrier function of the cells was evaluated by measuring TER. A subset of cells was treated under hypoxic conditions, and the TER changes observed upon administration of brimonidine were compared to those observed in cells in normoxic conditions.
Results
The ARPE cell membrane reached a peak resistance of 29.1±7.97 Ωcm2 after four weeks of culture. The TER of the cells treated under normoxic conditions increased with brimonidine treatment; however, the TER of the cells treated under hypoxic conditions did not change following the administration of brimonidine.
The retinal pigment epithelium (RPE) plays an essential role in maintaining the viability and functionality of the neural retina and, among other functions, prevents the neurosensory retina from accumulating extracellular fluid in the subretinal space [1].
The human RPE cell line (ARPE-19) has structural and functional properties characteristic of RPE cells in vivo and therefore makes this cell line valuable for in vitro studies of retinal pigment epithelium physiology. These cells were first described as developing into highly differentiated, polarized monolayers and exhibiting features of a polarized and differentiated epithelium [2,3]. The measurement of transepithelial resistance (TER) in cultured ARPE cells has been used to evaluate the barrier function of RPE cells [4,5].
Adrenergic α and β receptors have been identified in cultured human RPE cells; they participate in membrane permeability and membrane potential in ARPE cells [6]. Also, it has been reported that α-2-receptors are expressed in RPE-choriocapillaries, though the exact function of this α receptor has not yet been elucidated [7].
Brimonidine is a selective α-2-adrenergic agonist that has recently been approved for the long-term treatment of elevated intraocular pressure due to open angle glaucoma or ocular hypertension. In addition, it reaches significant concentrations with clinical dosing and exhibits a neuroprotective effect in animal models [8].
In the present study, we measured the TER in cultured ARPE cells in order to investigate the role of adrenergic α-2-agonists with respect to barrier function in the RPE.
The human RPE cell line, ARPE-19 cells were purchased from the American Type Culture Collection (Rockville, MD, USA). The cells were passaged and propagated using a slight modification of the technique described by Dunn et al [2]. In brief, the cells were cultured in medium (DMEM/F12; Gibco BRL, Grand Island, NY, USA) containing 10% fetal bovine serum (FBS; ThermoTrace, Melbourne, Australia) in a humidified incubator at 37℃ in 5% CO2. Media were changed twice a week.
The ARPE cells were seeded at a density of 1.66×105 cells/cm2 in DMEM/F-12 culture medium and supplemented with 100 U/mL penicillin-streptomycin, 2 mM L-glutamine, and 1% FBS on a microporous filter (Transwell; Costar Corning, Corning, NY, USA) until the cells cultured to confluence.
For the hypoxic cell group, the ARPE-19 cells were transferred to a hypoxic chamber containing 5% CO2, 94% N2 and 1% O2 24 hours prior to TER measurement.
The TER was measured using an epithelial volt-ohmmeter (EVOM; World Precision Instruments, Sarasota, FL, USA). The TER of the filter alone was measured as background and was subtracted from the TER obtained with the filters and ARPE-19 cells. Net TER measurements were calculated by subtracting the value of a blank, laminin-coated filter without cells from the experimental value. Final resistance-area products (Ω×cm2) were obtained by multiplication with the effective growth area.
The ARPE cells were cultured and the TER was measured every week for up to six weeks in order to determine the optimal incubation time for yielding the highest TER. The viability of the cells was assessed using trypan blue dye.
Brimonidine was purchased from Sigma Chemicals (St Louis, MO, USA) and was dissolved in dimethyl sulfoxide (DMSO) to a concentration of 50 mM and diluted to 0.01, 0.1, or 1 uM in DMEM/F12 medium containing 1% FBS just prior to use. The baseline TER was measured before administration of brimonidine. Immediately following this, 50 uL brimonidine solution was added to the apical chamber, and 50 uL culture media was taken out of the apical chamber simultaneously so that the concentration of brimonidine in the apical chamber reached 1, 10, or 100 nM (depending on the initial concentration) and so that the fluid volume of the apical chamber was not altered. To determine the optimal concentration of brimonidine, changes in TER were measured every 10 seconds for the first minute following exposure to each concentration of brimonidine and at 2, 3, and 5 minutes thereafter. Measurements were repeated at least three times for each well and for five wells of each concentration.
Changes in TER following administration of brimonidine to both the normoxic and hypoxic cell cultures were measured at every 10 seconds for the first minute following exposure and at 2, 3, 5, 10, 20, 30, and 120 minutes thereafter. Measurements were repeated at least three times for each well, and each experiment was repeated in 11 different wells.
The results were expressed as mean value±SD. Comparison of the TERs between the normoxic and hypoxic group was performed using the Mann-Whitney U-test. Changes in the TER from the baseline value following treatment with brimonidine were analyzed using the Wilcoxon signed rank test. Statistical significance was accepted at the p<0.05 level. Statistical analyses were performed using SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA).
The monolayer of cells developed a resistance of approximately 20.9±5.40 Ωcm2(n=5) after two weeks of culture and reached a peak resistance of 29.1±7.97 Ωcm2 (n=5) after four weeks of culture. The TER had decreased to 25.1±7.21 Ωcm2 (n=5) after six weeks of culture (Fig. 1). The viability of the ARPE cells was greater than 97% at all measuring points.
When the ARPE monolayer was treated with various concentrations of brimonidine at four weeks of culture, the 10 nM concentration of brimonidine induced the greatest change in TER, although it was not statistically significant.
The normoxic ARPE monolayer was treated with a 10 nM concentration of brimonidine at four weeks of culture; this was believed to be the optimal concentration and culture period for TER measurement. Treatment with brimonidine resulted in an increase in TER (Fig. 2). Pretreatment values of TER (mean 29.1±7.97 Ωcm2) increased to 31.5±6.0 Ωcm2 1 minute after treatment (p=0.05, n=11, Wilcoxon signed rank test) and maintained this level 30 minutes (32.3±9.16 Ωcm2, p=0.038) after exposure. Thereafter, the TER decreased until it returned to its baseline level two hours following brimonidine treatment.
This study indicates that the TER of an ARPE-19 monolayer can be increased by treatment with a nanomolar amount of apical brimonidine. However, this effect was not reproduced in the ARPE monolayer treated under hypoxic conditions. These results suggest that α-2 receptors play a role in maintaining barrier function in the RPE.
The RPE passively and actively transports fluid in the subretinal to choroidal direction; this RPE fluid "pump" function is thought to play a major role in reabsorption of subretinal fluid and in promoting and maintaining retinal attachment [9]. Therefore, the RPE membrane is a potential target for small therapeutic molecules that bind membrane receptors and activate fluid absorption from the subretinal space.
Several studies have reported that α-2-adrenergic receptors are present in the human ciliary body, retinal pigmented epithelium-choriocapillaris, iris, and neurosensory retina [10,11]. Quinn and associates reported that adrenergic agonists, including isoproterenol and epinephrine, activate ion transport at the apical membrane of the human fetal RPE [6]. We hypothesize that the presence of α-2-receptors in the RPE could change the barrier function of the RPE membrane.
Brimonidine, an α-2-adrenergic receptor agonist, has been employed in the clinical setting of glaucoma because of its therapeutic potential for reducing intraocular pressure (IOP) by aqueous suppression and enhanced uveoscleral outflow. In addition to these IOP-lowering effects, several recent investigations in animal models suggest that brimonidine may exert a neuroprotective effect on retinal ganglion cells by preventing cell death secondary to ischemic injury [8,12]. A recent clinical pilot study suggests a trend toward slower progression of retinal dystrophy when treated with topical brimonidine [13]. Furthermore, topically applied brimonidine can reach the back of the eye at nanomolar concentrations sufficient to activate α-2 adrenergic receptors. This yields obvious advantages for the treatment of various retinal diseases in clinical settings [14].
Following exposure to brimonidine, there was no increase in the TER of the ARPE membrane culture subjected to hypoxic conditions. This result suggests that hypoxia can induce dysfunction of active ion transport at the apical membrane of the ARPE.
Some studies have reported that DMSO at concentrations of 1% or 10% can induce TER changes in various cell membranes [15,16]. In contrast, Cui et al. [5] showed that 0.05% DMSO did not alter TER in cultured ARPE. In this study, the final concentration of DMSO was 1/250 of that used in the former study, and its effect on TER was therefore insignificant
One limitation of this study is that we could not elucidate the mechanisms of TER change in the ARPE membrane. An analysis of ion transfer and permeability testing could have possibly supported the TER changes observed in this study.
Although the exact mechanism remains unclear, brimonidine enhanced the barrier function in ARPE-19 cells in the present study. The specific effects of brimonidine on the action of ion pumps require further investigation.
Figures and Tables
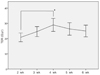 | Fig. 1Changes of transepithelial resistance (TER) according to the culture periods. The TER was highest at 4 weeks of culture and decreased thereafter. |
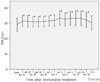 | Fig. 2The effects of brimonidine on transepithelial resistance in polarized ARPE-19 monolayers cultured in normoxic condition. ARPE-19 cells were treated with 10 nM brimonidine and transepithelial resistance (TER) was measured at indicated time points. Data are mean±2SD (n=14). The TER values showed significant increase compared to the pre-treatment values immediately after the exposure to brimonidine and up to 30 minutes. Thereafter, the TER decreased until it returned to its baseline level two hours following brimonidine treatment. |
 | Fig. 3The effects of brimonidine on transepithelial resistance (TER) in polarized ARPE-19 monolayers cultured in hypoxic condition. The TER of the hypoxic ARPE monolayer did not change in the two hours following exposure to brimonidine. |
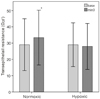 | Fig. 4The effects of brimonidine on tranepithelail resistance (TER) in polarized ARPE-19 monolayers cultured in normoxic and hypoxic conditions. The ARPE-19 monolayers treated in the hypoxic chamber showed no increment of TER after the treatment of brimonidine (p=0.038 compared to the baseline value). |
Acknowledgements
This study was supported by the National Research Foundation of Korea grant funded by the Ministry of Education, Science and Technology, Republic of Korea (No.2009-0084597).
References
1. Marmor MF. Control of subretinal fluid: experimental and clinical studies. Eye. 1990. 4:340–344.
2. Dunn KC, Aotaki-Keen AE, Putkey FR, Hjelmeland LM. ARPE-19, a human retinal pigment epithelial cell line with differentiated properties. Exp Eye Res. 1996. 62:155–169.
3. Tian J, Ishibashi K, Handa JT. The expression of native and cultured RPE grown on different matrices. Physiol Genomics. 2004. 17:170–182.
4. Geisen P, McColm JR, King BM, Hartnett ME. Characterization of barrier properties and inducible VEGF expression of several types of retinal pigment epithelium in medium-term culture. Curr Eye Res. 2006. 31:739–748.
5. Cui HS, Hayasaka S, Zhang XY, et al. Effect of berberine on barrier function in a human retinal pigment epithelial cell line. Jpn J Ophthalmol. 2007. 51:64–67.
6. QuinnRH , Quong JN, Miller SS. Adrenergic receptor activated ion transport in human fetal retinal pigment epithelium. Invest Ophthalmol Vis Sci. 2001. 42:255–264.
7. Matsuo T, Cynader MS. Localization of alpha-2 adrenergic receptors in the human eye. Ophthalmic Res. 1992. 24:213–219.
8. Danylkova NO, Alcala SR, Pomeranz HD, McLoon LK. Neuroprotective effects of brimonidine treatment in a rodent model of ischemic optic neuropathy. Exp Eye Res. 2007. 84:293–301.
9. Pederson JE. Ryan SJ, editor. Fluid physiology of the subretinal space. Retina. 2006. 4th ed. Philadelphia: Elsevier/Mosby;1909–1920.
10. Bylund DB, Chcko DM. Characterization of alpha2 adrenergic receptor subtypes in human ocular tissue homogenates. Invest Ophthalmol Vis Sci. 1999. 40:2299–2306.
11. Diebold Y, Enriquez de Salamanca A, Calonge M, et al. Alpha2-adrenergic receptors are present in normal human conjunctiva. Curr Eye Res. 2005. 30:1121–1129.
12. Ma K, Xu L, Zhang H, et al. Effect of brimonidine on retinal ganglion cell survival in an optic nerve crush model. Am J Ophthalmol. 2009. 147:326–331.
13. Merin S, Obolensky A, Farber MD, Chowers I. A pilot study of topical treatment with an alpha2-agonist in patients with retinal dystrophies. J Ocul Pharmacol Ther. 2008. 24:80–86.
14. Acheampong AA, Shackleton M, John B, et al. Distribution of brimonidine into anterior and posterior tissues of monkey, rabbit, and rat eyes. Drug Metab Dispos. 2002. 30:421–429.
15. Kosik-Bogacka D, Mlodzik-Danielewicz N, Banach B, Tyrakowski T. Effect of amiloride and bumetanide on transepithelial ion transport in isolated rabbit cecal and colonic wall. Postepy Hig Med Dosw. 2005. 59:229–235.
16. Taub ME, Kristensen L, Frokjaer S. Optimized conditions for MDCK permeability and turbidimetric solubility studies using compounds representative of BCS classes I-IV. Eur J Pharm Sci. 2002. 15:331–340.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download