Abstract
Purpose
To evaluate corneal biomechanical properties in eyes that had previously undergone penetrating keratoplasty (PK) using the ocular response analyzer (ORA).
Methods
We recruited 26 patients who had received unilateral PK. Corneal hysteresis (CH), corneal resistance factor (CRF), Goldmann-correlated intraocular pressure (IOPg), and cornea-compensated intraocular pressure (IOPcc) were measured with the ORA and were compared to the measurements from the contralateral eyes that did not undergo PK.
Results
The CH was 8.95±2.59 mmHg in eyes that underwent PK and 9.78±1.45 mmHg in the contralateral eyes that did not undergo PK (p=0.077). The CRF was 10.26±2.64 mmHg in post-PK eyes and 9.75±1.45 mmHg in the contralateral eyes (p=0.509), and the CH-CRF was significantly smaller in post-PK eyes (-1.31±2.32 mmHg in post-PK eyes vs. 0.03±0.88 mmHg in fellow eyes, p=0.016). The IOPg and IOPcc were significantly higher in the PK group than they were in the control group. The IOPcc's were 20.81±7.81 mmHg and 16.27±2.49 mmHg in post-PK and control eyes, respectively (p=0.011); and the IOPg's were 19.22±7.34 mmHg and 15.07±3.03 mmHg in post-PK and control eyes, respectively (p=0.019). The IOPcc-g's were 1.59±2.81 mmHg and 1.21±1.30 mmHg in post-PK and control eyes, respectively (p=0.412), and the central corneal thickness (CCT)'s were 489.11±90.60 µm and 556.24±42.84 µm in post-PK and control eyes, respectively (p=0.068).
The ocular response analyzer (ORA, Reichert Ophthalmic Instruments, Depew, NY, USA) can measure corneal biomechanical properties such as corneal hysteresis (CH) and corneal resistance factor (CRF) [1]. In addition, noncontact intraocular pressures such as the Goldmann-correlated intraocular pressure (IOPg) and corneal-compensated intraocular pressure (IOPcc) can be measured by the ORA. The ORA detects the pressure at which the cornea is flattened as it is indented with an air puff and the pressure at which it is flattened as it returns to its original shape. Corneal hysteresis is defined as the difference between these two pressures and is thought to represent the viscosity of the cornea. The mean of these two pressures is the IOPg. The IOPcc is a pressure measurement that utilizes the CH measurement to determine an intraocular pressure (IOP) value that is less affected by corneal properties such as central corneal thickness (CCT). Moreover, many previous studies have reported that the IOPcc is unrelated to CCT [1-5]. CRF is an empirically determined parameter that is thought to represent the overall resistance of the cornea [6]. ORA measurement of these parameters has previously been reported to demonstrate good reproducibility and clinical reliability [7].
Although the significance of these ORA parameters is not fully understood, several studies have reported changes in these parameters in various diseases, as well as following certain procedures. CH has been shown to be significantly lower in eyes with keratoconus [1,8,9], Fuchs' dystrophy [1,10], high myopia [11], glaucoma [1,5], and inpost-laser in situ keratomileusis (LASIK) eyes [2,12]. Following clear corneal incision cataract surgery, CH and CRF were found to be decreased at one day postoperatively; this change was maintained for one week, after which the pressure increased back to baseline by one month postoperatively [13].
Penetrating keratoplasty (PK) is frequently performed for various corneal pathologies. However, there have previously been no studies using the ORA to measure the biomechanical properties of post-PK eyes. As such, we measured the corneal biomechanical properties of patients that had previously undergone unilateral PK using the ORA and compared the measurements with those of the normal contralateral eyes.
This study was approved by the Institutional Review Board of the Clinical Research Institute of Seoul National University Hospital.
Twenty-six eyes that had previously undergone PK for unilateral corneal disease at Seoul National University Hospital were included in this study. Slit lamp biomicroscopic examination was performed at the time of recruitment in order to exclude any patients with noticeable pathology in the contralateral eye and to identify evidence of rejection or recurrence in the post-PK eye. Further studies were performed on an as-needed basis. Patients with no evidence of rejection, infection, or recurrence of disease in the post-PK eye and with no evidence of disease in the contralateral eye were included.
The ORA (Reichert Ophthalmic Instruments) was used to measure CH, CRF, IOPg, and IOPcc in both the post-PK and contralateral normal eyes. One examiner performed all of the measurements with three consecutive readings in each eye, including only good-quality measurements with two distinct peaks. The mean of the three measurements was used for statistical analysis. CCT was measured with the ORA-attached handheld ultrasonic pachymeter.
All statistical analyses were performed with SPSS ver. 15.0 (SPSS Inc., Chicago, IL, USA). The Wilcoxon signed rank test was used to analyze the difference in each ORA parameter between the post-PK and contralateral eyes. Correlation between parameters was evaluated with Spearman's rho correlation. A p-value less than 0.05 was considered statistically significant.
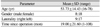
The mean patient age was 53.73±14.43 years, and eight of the patients were male. The mean duration since undergoing PK was 19 months. Demographic data of the patients is summarized in Table 1. The causative diseases requiring PK are shown in Table 2.
All eyes underwent PK using the conventional 16 interrupted suture technique performed by two surgeons (KMK and OJY).
The ORA parameters in the post-PK eyes and the contralateral normal eyes are shown in Table 3. CH was decreased in the post-PK eyes, but this difference was not statistically significant (8.95±2.59 mmHg in the post-PK eyes vs. 9.78±1.45 mmHg in the contralateral normal eyes; p=0.077). CRF was higher in the post-PK eyes than in the fellow eyes, but without statistical significance (10.26±2.64 mmHg in the post-PK eyes vs. 9.75±1.45 mmHg in the fellow eyes; p=0.509). The IOPcc and IOPg were significantly higher in the post-PK group than in the control group (IOPcc, 20.81±7.81 mmHg in the post-PK eyes and 16.27±2.49 mmHg in the contralateral eyes, p=0.011; IOPg, 19.22±7.34 mmHg in the post-PK eyes and 15.07±3.03 mmHg in the fellow eyes, p=0.019). In addition, the CCTs were 489.11±90.60 µm and 556.24±42.84 µm in the post-PK and fellow eyes, respectively (p=0.068).
In addition to the four basic parameters measured by the ORA, the difference between CH and CRF and the difference between IOPcc and IOPg (IOPcc-g) were calculated and analyzed between the groups. CH-CRF was significantly smaller in post-PK eyes than in contralateral eyes (-1.31±2.32 mmHg in post-PK eyes vs. 0.03±0.88 mmHg in fellow eyes, p=0.016). CH-CRF was negatively correlated with IOPcc (correlation coefficient, -0.966; p<0.001) and IOPg (correlation coefficient, -0.987; p<0.001) (Fig. 1). IOPcc-g was not significantly different between post-PK eyes and contralateral eyes (1.59±2.81 mmHg in post-PK eyes vs. 1.21±1.30 mmHg in fellow eyes; p=0.412). IOPcc-g demonstrated a negative correlation with both CH (correlation coefficient, -0.832; p<0.001) and CRF (correlation coefficient, -0.806; p<0.001) (Fig. 2).
CH is known to represent the viscosity of the cornea, reflecting the collagen structure and hydration state of the cornea. CH is believed to have little association with CCT or IOP, although the degree of association varies among reports [14]. It has been reported that CH is decreased in keratoconus, Fuchs' dystrophy, high myopia, and glaucoma, as well as in post-LASIK corneas and in the immediate postoperative period following cataract surgery using a clear corneal incision. In this study, we found that CH tended to decrease in post-PK eyes.
CRF is thought to represent the elasticity of the cornea, with stronger correlations with IOP and CCT compared to those of CH. CRF has also been reported to be decreased in keratoconus, Fuchs' dystrophy, and in post-LASIK eyes. Our study demonstrated that there was no significant difference in CRF between post-PK eyes and normal fellow eyes; only a slight increase was observed in post-PK eyes.
Regarding the difference between CH and CRF, previous reports have demonstrated that CH-CRF is negative in both normal and glaucoma subjects and positive in keratoconus and post-LASIK subjects [14]. Also, CH-CRF has been reported to be increased in eyes with high myopia and elevated IOPg and IOPcc [11]. As for the mechanism of this change in glaucomatous eyes, previous investigators have theorized that "corneal remodeling" results in decreased CH as a response to glaucomatous damage and that a high CRF represents a stiffened cornea resulting from high IOP [14]. We found that CH-CRF was significantly lower in post-PK eyes compared to those of fellow eyes. This might be attributed to the fact that the IOPg and IOPcc were both significantly higher in post-PK eyes in this study. It remains uncertain whether the duration of increased IOP was sufficient in these patients to induce "corneal remodeling;" however, significant decreases in CH and CH-CRF in the post-PK eyes might be associated with higher IOPs. The strong negative correlations of CH-CRF with IOPcc and IOPg further support this hypothesis.
Additionally, although both IOPcc and IOPg were higher in post-PK eyes, IOPcc-g was not significantly different in the post-PK eyes. Given that IOPcc-g is thought to reflect the degree of cornea-induced IOP measurement error [4]; these findings suggest that cornea-induced IOP measurement error was not significantly higher in post-PK eyes than it was in normal eyes.
In contrast to the irregular applanation signal previously reported for a transplanted cornea [1], the applanation curves acquired in all the patients in our study were similar to the curves acquired from normal subjects, with no noticeable irregularities.
This study has several limitations in terms of the small number of eyes studied and the heterogeneities of the underlying conditions requiring PK. In addition, this study is a cross-sectional study. A prospective, controlled study with a large number of patients is needed to further characterize corneal biomechanical changes following PK procedures.
In conclusion, our study revealed that CH tended to decrease and CRF tended to increase following PK, resulting in a significant decrease in CH-CRF. These changes may have been influenced by an increase in IOP and a decrease in CCT in the post-PK eyes.
Figures and Tables
 | Fig. 1Correlations of corneal hysteresis (CH) and corneal resistance factor (CRF) with cornea-compensated intraocular pressure (IOPcc) and Goldmann-correlated intraocular pressure (IOPg). |
 | Fig. 2Correlations of cornea-compensated intraocular pressure and Goldmann-correlated intraocular pressure (IOPcc-g) with corneal hysteresis (CH) and corneal resistance factor (CRF). |
References
1. Luce DA. Determining in vivo biomechanical properties of the cornea with an ocular response analyzer. J Cataract Refract Surg. 2005. 31:156–162.
2. Ortiz D, Pinero D, Shabayek MH, et al. Corneal biomechanical properties in normal, post-laser in situ keratomileusis, and keratoconic eyes. J Cataract Refract Surg. 2007. 33:1371–1375.
3. Pepose JS, Feigenbaum SK, Qazi MA, et al. Changes in corneal biomechanics and intraocular pressure following LASIK using static, dynamic, and noncontact tonometry. Am J Ophthalmol. 2007. 143:39–47.
4. Medeiros FA, Weinreb RN. Evaluation of the influence of corneal biomechanical properties on intraocular pressure measurements using the ocular response analyzer. J Glaucoma. 2006. 15:364–370.
5. Lam A, Chen D, Chiu R, Chui WS. Comparison of IOP measurements between ORA and GAT in normal Chinese. Optom Vis Sci. 2007. 84:909–914.
6. Sullivan-Mee M, Billingsley SC, Patel AD, et al. Ocular Response Analyzer in subjects with and without glaucoma. Optom Vis Sci. 2008. 85:463–470.
7. Moreno-Montanes J, Maldonado MJ, Garcia N, et al. Reproducibility and clinical relevance of the ocular response analyzer in nonoperated eyes: corneal biomechanical and tonometric implications. Invest Ophthalmol Vis Sci. 2008. 49:968–974.
8. Kirwan C, O'Malley D, O'Keefe M. Corneal hysteresis and corneal resistance factor in keratoectasia: findings using the Reichert ocular response analyzer. Ophthalmologica. 2008. 222:334–337.
9. Shah S, Laiquzzaman M, Bhojwani R, et al. Assessment of the biomechanical properties of the cornea with the ocular response analyzer in normal and keratoconic eyes. Invest Ophthalmol Vis Sci. 2007. 48:3026–3031.
10. del Buey MA, Cristobal JA, Ascaso FJ, et al. Biomechanical properties of the cornea in Fuchs' corneal dystrophy. Invest Ophthalmol Vis Sci. 2009. 50:3199–3202.
11. Shen M, Fan F, Xue A, et al. Biomechanical properties of the cornea in high myopia. Vision Res. 2008. 48:2167–2171.
12. Gatinel D, Chaabouni S, Adam PA, et al. Corneal hysteresis, resistance factor, topography, and pachymetry after corneal lamellar flap. J Refract Surg. 2007. 23:76–84.
13. Kucumen RB, Yenerel NM, Gorgun E, et al. Corneal biomechanical properties and intraocular pressure changes after phacoemulsification and intraocular lens implantation. J Cataract Refract Surg. 2008. 34:2096–2098.
14. Touboul D, Roberts C, Kerautret J, et al. Correlations between corneal hysteresis, intraocular pressure, and corneal central pachymetry. J Cataract Refract Surg. 2008. 34:616–622.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download