Abstract
The purpose of this case report is to evaluate the visual outcome of an intravitreal triamcinolone acetonide injection (IVTA) as a treatment for a patient with acute nonarteritic anterior ischemic optic neuropathy (NAION). A 65-year-old male patient with severe visual loss due to acute NAION was treated with 4 mg/0.1mL IVTA. Fundus examination and measurements of the patient's best-corrected visual acuity and visual field were performed before and after the injection at 2 weeks, 1 month, 3 months, and 6 months. The best-corrected visual acuity changed from 0.05 before the injection to 0.16 at 2 weeks, 0.3 at 1 month, and 0.4 at 3 months and at the final visit. Optic disc swelling had markedly decreased at 1 week postoperatively and disappeared at 2 weeks after the injection. The clinical course of this patient suggests that an IVTA may be effective in increasing visual acuity following an acute NAION. A large randomized controlled trial is needed to assess the efficacy of IVTA as a treatment for NAION.
Nonarteritic anterior ischemic optic neuropathy (NAION) is characterized by a sudden, painless, monocular visual loss in patients after the fourth or fifth decade of life.1,2 The known risk factors are a small optic nerve head, systemic hypertension, and hyperlipidemia.3,4 However, there is no proven effective treatment for NAION patients.2,5
Intravitreal triamcinolone acetonide injection (IVTA) may help to resolve optic disc edema and stop a vicious cycle of ischemia and edema which can lead to further tissue infarction.6 Recently, Jonas et al.7 reported that IVTA was not effective treatment for NAION; however, Kaderli et al.6 reported rapid visual recovery following IVTA in NAION patients.
The purpose of this study is to report the visual outcome of a single patient who received 4 mg IVTA as treatment for acute NAION.
A 65-year-old male presented with sudden visual loss of his right eye of 4 days duration. The patient noted his visual loss upon awakening from sleep. There was no associated ocular pain or headache. His initial best-corrected visual acuity was 0.05 and a relative afferent pupillary defect (1.8 log unit) was present. Fundus examination of his affected eye demonstrated optic disc edema and a flame-shaped peripapillary hemorrhage (Fig. 1). The optic disc edema involved the whole disc, with the exception of the superior zone. The early phase of an intravenous fluorescein angiogram showed a segmental perfusion delay of the optic disc (Fig. 2). A diffuse cecocentral scotoma was present in the right eye (Fig. 3). The patient reported a history of systemic hypertension of at least 10 years. The erythrocyte sedimentation rate, C-reactive protein levels, and protein C concentration were all normal. The patient did not show any characteristics of arteritic anterior ischemic optic neuropathy and was diagnosed with acute NAION. The patient was informed of the natural history of NAION and the fact that there is no proven effective treatment for NAION. After full explanation of the expected effects and possible complications of IVTA, the patient provided informed consent.
An intravitreal injection of 4 mg/0.1mL triamcinolone acetonide (TA) was performed in the affected eye. The IVTA injection was performed in a surgical room under sterile conditions with topical anesthesia (Alcaine®, Alcon, USA). The injection was administered with a 30 gauge needle, 4.0 mm from the inferotemporal limbus. To prevent infection and ocular hypertension due to the IVTA, the patient received topical antibiotics (Vigamox®, Alcon, USA) following the injection and his intraocular pressure was measured 24 hours after the IVTA injection and at each follow-up visit. Measurements of the patient's best-corrected visual acuity by Snellen acuity, Goldmann perimetry, applanation tonometry, slit lamp biomicroscopy, and fundus examination of the affected eye were performed at 2 weeks, 1 month, 3 months, and 6 months following the IVTA.
The patient's best-corrected visual acuity changed from 0.05 before the injection to 0.16 at 2 weeks, 0.3 at 1 month, and 0.4 at 3 months postoperatively and at the final visit. The optic disc edema had markedly decreased at 1 week and disappeared at 2 weeks following the injection. At 3 months after the IVTA injection, we observed a segmental pale neuroretinal rim (5 o'clock-11 o'clock) during the fundus exam (Fig. 4). The area of the pale neuroretinal rim corresponded with the previous segmental perfusion delay seen with the fluorescein angiogram. The patient did not develop intraocular pressure exceeding 21 mmHg, progression of cataract, or endophthalmitis during follow-up.
The patient presented here showed a relatively good recovery of visual acuity and a rapid resolution of optic disc edema. The patient's best-corrected visual acuity improved by five Snellen lines following the IVTA injection. There was also a marked decrease in optic disc edema during the first week after the injection and resolution of the optic disc edema by the second week.
The natural course of optic disc edema in NAION has been reported to spontaneously resolve within 6-8 weeks.2,8 We suggest that rapid resolution of the optic disc edema in this patient may be the major cause of visual acuity recovery. It has been inferred that rapid reduction of optic disc edema by IVTA could prevent further tissue damage by stopping a vicious cycle of ischemia, edema, and compartment syndrome occurring in NAION.2,6 Another possibility may be that IVTA could serve to decrease macrophage presence in the affected areas of infarcted brain and optic nerve;9 however, we do not have any histological proof of this hypothesis.
The result of the present study corresponds with Karderli et al.6 who reported that IVTA led to recovery of visual acuity in 4 NAION patients. However, our finding is different from those of Jonas et al.,7 who reported that IVTA was not effective in visual acuity recovery for 3 NAION patients. The reason for this difference is the dosage of TA used. Twenty mg of TA is 5 times greater than the 4 mg used in our study and by Karderli et al.6; a higher dose of TA remains in the eye longer. One of the patients in the study by Jonas et al.7 developed ocular hypertension following IVTA injection. A high intraocular pressure might interfere with vascular circulation and axoplasmic transport in the affected eye. In addition, they did not mention the duration of optic disc edema following the IVTA injection.
This is the first case report that demonstrates visual acuity recovery in acute NAION following IVTA injection in a Korean patient. Considering that there is no proven effective treatment for NAION, IVTA injection could be an alternative and effective treatment option for acute NAION without any systemic complications. However, large randomized controlled trials may be necessary to establish the efficacy and safety of IVTA injections as the treatment of choice for acute NAION.
Figures and Tables
 | Fig. 1A fundus photograph at the time of diagnosis demonstrates optic disc swelling with a flame-shaped hemorrhage. The optic disc swelling involved the whole disc, with the exception of the superior zone. |
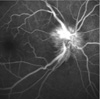 | Fig. 2Intravenous fluorescein angiogram. The early phase of an intravenous fluorescein angiogram showed a segmental perfusion delay in the optic disc. |
References
1. Repka MX, Savino PJ, Schatz NJ, Sergott RC. Clinical profile and long-term implications of anterior ischemic neuropathy. Am J Ophthalmol. 1983. 96:478–483.
2. Martin TJ, Corbett JJ. Neuro-ophthalmology: The requisites in ophthalmology. 2000. 1st ed. St Louis: Mosby;62–67.
3. Beck RW, Savino PJ, Repka MX, et al. Optic disc structure in anterior ischemic optic neuropathy. Ophthalmology. 1984. 91:1334–1337.
4. Kim DH, Hwang JM. Risk factors for Korean patients with anterior ischemic optic neuropathy. J Korean Ophthalmol Soc. 2007. 48:1527–1531.
5. Beck RW, Hayreh SS, Podhajsky PA, et al. Aspirin therapy in nonarteritic anterior ischemic optic neuropathy. Am J Ophthalmol. 1997. 123:212–217.
6. Kaderli B, Avci R, Yucel A, et al. Intravitreal triamcinolone improves recovery of visual acuity in nonarteritic anterior ischemic optic neuropathy. J Neuroophthalmol. 2007. 27:164–168.
7. Jonas JB, Spandau UH, Harder B, Sauder G. Intravitreal triamcinolone acetonide for treatment of acute nonarteritic anterior ischemic optic neuropathy. Graefes Arch Clin Exp Ophthalmol. 2007. 245:749–750.
8. Hayreh SS, Zimmerman MB. Nonarteritic anterior ischemic optic neuropathy: Natural history of visual outcome. Ophthalmology. 2008. 115:298–305.
9. Knox DL, Kerrison JB, Green WR. Histopathologic studies of ischemic optic neuropathy. Trans Am Ophthalmol Soc. 2000. 98:203–220.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download