Abstract
We report a very rare case of trichilemmal carcinoma (TLC) involving the upper eyelid. To the best of our knowledge, this is the first report of trichilemmal carcinoma of the upper eyelid in Korea. A 51-year-old man presented to our hospital complaining of a bloody discharge from his left upper eyelid. He had a soft and lobulated mass on the palpebral conjunctiva. An incisional biopsy revealed trabecular growth of tumor cells with clear cytoplasm, prominent nucleoli, frequent mitoses, and foci of trichilemmal keratinization. Immunohistochemically, the lesion was positive for p53 and negative for CD 34. A diagnosis of TLC was made, and total excision of the mass and reconstruction of the eyelid were performed. Trichilemmal carcinoma is a rare malignant tumor, though it appears to be an indolent neoplasm with no metastatic potential. The treatment of choice for trichilemmal carcinoma of the eyelid is complete excision with tumor-free margins due to the locally invasive nature of the lesion.
Trichilemmal carcinoma (TLC) is an uncommon malignant adnexal tumor that originates from the external hair sheath.1 Trichilemmal carcinoma has a benign clinical course, but exhibits a malignant and invasive histological appearance.2 Eyelid involvement of TLC has been only rarely reported. Here, we report the first Korean case of TLC involving the upper eyelid.
A 51-year-old man presented with bloody discharge from his left upper eyelid that had begun 2 to 3 days prior to presentation. One month prior to visiting our hospital, he had noticed the presence of a nontender, palpable, movable nodule that had not changed in size since discovery (Fig. 1). Swelling of the left upper lid was apparent.
Slit-lamp examination revealed a 0.5×0.5 cm-sized protruding lesion of the left upper palpebral conjunctiva. The mass was slightly yellow and was composed of multiple lobules (Fig. 2). An incisional biopsy was performed.
On incisional biopsy, a yellowish solid mass was observed. The mass demonstrated a trabecular growth pattern of tumor cell nests characterized by clear cytoplasm, prominent nucleoli, frequent mitoses, few atypical tripolar mitoses, and focal necrosis. There were also foci of trichilemmal keratinization (Fig. 3). On immunohistochemical staining, the tumor cells were diffusely distributed and were strongly positive for p53, but were negative for CD 34 (Fig. 4). Given the histological and immunohistochemical findings, the lesion was determined to be a TLC.
The mass was completely excised with a pentagonal wedge resection of the upper lid, including a 5-mm safety margin, and the eyelid was reconstructed. The mass lesion was first outlined in a pentagonal shape and then excised; the excision included the surrounding palpebral conjunctiva. Tumor-free margins were ensured by frozen section analysis (Fig. 5A). The posterior lamella was reconstructed with a sliding tarsoconjunctival flap, and the anterior lamella was repaired with a myocutaneous advancement flap (Fig. 5B-5D). After completion of the procedure, a reverse Frost suture was inserted into the center of the upper eyelid to prevent corneal exposure.
At the six month follow-up, there was no evidence of local recurrence or metastasis.
Trichilemmal carcinoma was first described in 1976 as "a histologically invasive, cytologically atypical, clear cell neoplasm of adnexal keratinocytes which is in continuity with the epidermis and/or follicular epithelium."3 In most patients, the tumor typically occurs on sun-exposed areas of the face and scalp,1,2,4,5 but is rare on the eyelid.5 Trichilemmal carcinoma on the eyelid was first described in 1993 in a 95-year-old woman.5,6
Trichilemmal carcinoma typically affects individuals aged 40 years and older.7,8 Trichilemmal carcinoma can have a grossly papular, nodular, or exophytic appearance.2,8,9 All TLCs reported to date have been less than 2 cm in diameter.2,3 Lai and colleagues10 reported an induration of the eyelid with a small area of ulceration and keratosis, but a normal conjunctiva. In previous reports,5,10,11 there were no significant changes of the conjunctiva; in the current case however, the upper lid mass completely penetrated into the inner side of the upper lid and was seen on the conjunctival side on slit-lamp examination.
Histopathologically, TLC demonstrates a lobular proliferation centered on pilosebaceous structures and is composed of clear cells that are characterized by clear cytoplasm and prominent nucleoli. Trichilemmal carcinoma exhibits trichilemmal keratinization with an abrupt or pagetoid interface and dermal invasion.8-10
Malignant proliferating trichilemmal tumors (PTTs) are often confused with TLC. However, PTT is not synonymous with TLC.3,6,9 Proliferating trichilemmal tumors usually arise in a pre-existing trichilemmal cyst and are frequently confined to the scalp. Proliferating trichilemmal tumors are larger than TLCs (with a diameter of up to 25 cm). Proliferating trichilemmal tumors demonstrate sharply circumscribed convoluted lobules with pushing margins, deep dermal extensions, extensive areas of tumor cell necrosis, abrupt keratinization, minimal pleomorphism, low mitotic activity, and foci indistinguishable from a trichilemmal cyst.3,6 Proliferating trichilemmal tumors are apt to recur and to metastasize, as distinct from the behavior of TLCs.6,9
Trichilemmal carcinoma must be differentiated from other skin cancers. It is easy to confuse TLC with clear cell basal cell carcinoma (BCC), but zones of clear cells are not sufficient to diagnosis conventional BCC.9,10 Squamous cell carcinoma demonstrates cellular atypia and cells with clear cytoplasm, similar to TLC, but differs from TLC in the absence of trichilemmal keratinization or lobular proliferation.7,10 Also, TLC resembles trichilemmoma in the presence of a plate-like endophytic nodule extending into the dermis, but differs with respect to the occurrence of frequent mitosis or cellular atypia.1
p53 tumor suppressor gene mutations are often found in patients with nonmelanoma skin cancer. Complete loss of p53 on immunohistochemical staining represents the malignant transformation of PTT.11 Also, focal staining for the presence of CD 34 is a marker of differentiation from the outer hair sheath. However, the tumor of the current patient was negative for CD 34, indicating an undifferentiated tumor cell type.12,13
Trichilemmal carcinoma is locally invasive and, histologically, appears to have high-grade mitotic potential. However, TLC generally has a benign clinical course, and there is no evidence of recurrence after complete excision.2,7,9,10
Masayuki et al.11 reported a case of TLC of the upper eyelid that was treated with full dose irradiation. However, the tumor recurred and invaded the orbit. The tumor was resected in a procedure involving the eyelid and orbital contents. At the 29 month follow-up, there was no evidence of local recurrence or metastasis.
Consequently, upon presentation of an indurated nodule or an ulcerated mass on the eyelid, it is necessary to consider the possibility of a cancerous lesion.2,6,8 Trichilemmal carcinoma should be considered in the differential diagnosis of an eyelid mass. Trichilemmal carcinoma is a malignant tumor that usually does not metastasize, despite local regional recurrence.1,5,14 It is important to perform a total excision of the tumor mass, with tumor-free margins, and to offer careful follow-up to all patients.1,10,12
Figures and Tables
Fig. 1
The patient had a swelling of the upper eyelid and a palpable, nontender, movable mass on the left eyelid.

Fig. 2
A yellowish, soft, multi-lobulated mass is shown. The mass protrudes through the lateral end of the left upper palpebral conjunctiva. (A) Gross view. (B) Slit-lamp view.
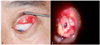
Fig. 3
Histology of the mass. (A) The section revealed a trabecular growth pattern of tumor cell nests (H&E, ×40). (B, C) The cells were characterized by clear cytoplasm, prominent nucleoli, frequent mitoses, few atypical tripolar mitoses, and focal necrosis. There were also foci of trichilemmal keratinization (black arrow) (B: H&E, ×100; C: H&E, ×400).

Fig. 4
Immunohistochemical staining of the mass. (A) Negative staining for CD 34. (B) Strongly positive staining for p53.

Fig. 5
Mass excision and reconstruction of the defect. (A) Complete mass excision using a pentagonal shape. Tumor-free margins were confirmed by frozen section biopsy. (B) Reconstruction of the posterior lamella with a tarsoconjunctival sling. (C) Reconstruction of the anterior lamella with a myocutaneous advancement flap. (D) Complete closure of the defect.

References
1. Billingsley EM, Davidowski TA, Maloney ME. Trichilemmal carcinoma. J Am Acad Dermatol. 1997. 36:107–109.
2. Reis JP, Tellechea O, Cunha MF, Baptista AP. Trichilemmal carcinoma: review of 8 cases. J Cutan Pathol. 1993. 20:44–49.
3. Headington JT. Tumour of the hair follicle: a review. Am J Pathol. 1976. 85:479–514.
4. Song MG, Min HG, Jung SY, et al. Trichilemmal carcinoma with a cutaneous horn. Br J Dermatol. 2000. 143:646–647.
5. Dailey JR, Helm KF, Goldberg SH. Tricholemmal carcinoma of the eyelid. Am J Ophthalmol. 1993. 115:118–119.
6. Lee SJ, Choi KH, Han JH, et al. Malignant proliferating trichilemmal tumor of the lower eyelid. Ophthal Plast Reconstr Surg. 2005. 21:349–352.
7. Boscaino A, Terrancciano LM, Donofrio V, et al. Trichilemmal carcinoma: a study of seven cases. J Cutan Pathol. 1992. 19:94–96.
8. Swanson PE, Marrogi AJ, Williams DJ, et al. Tricholemmal carcinoma: a clinicopathologic study of 10 cases. J Cutan Pathol. 1992. 19:100–109.
9. Chan KO, Lim IJ, Baladas HG, et al. Multiple tumour presentation of trichilemmal carcinoma. Br J Plast Surg. 1999. 52:665–667.
10. Lai TF, Huilgol SC, James CL, et al. Trichilemmal carcinoma of the upper eyelid. Acta Ophthalmol Scand. 2003. 81:536–538.
11. Masayuki T, Hideo N, Yurihisa I, et al. Surgical treatment of recurrent trichilemmal carcinoma of the upper eyelid. Otolaryngol Head Neck Surg (Tokyo). 2004. 76:709–713.
12. Takata M, Rehman I, Rees JL. A trichilemmal carcinoma arising from a proliferating trichilemmal cyst: the loss of the wild-type p53 is a critical event in malignant transformation. Human Pathology. 1998. 29:193–195.
13. Poblet E, Jimenez-Acosta F, Rocamora A. QBEND/10 (anti-CD34 antibody) in external root sheath cells and follicular tumours. J Cutan Pathol. 1994. 21:224–228.
14. Herrero J, Monteagudo C, Ruiz A, Llombart-Bosch A. Malignant proliferating trichilemmal tumours: an histopathological and immunohistochemical study of three cases with DNA ploidy and morphometric evaluation. Histopathology. 1998. 33:542–546.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download