Laser iridotomy is performed primarily for the treatment of acute angle-closure glaucoma (AACG) caused by relative pupillary block. Laser iridotomy offers the same efficacy as surgical iridectomy with fewer complications and can be easily and quickly performed in outpatient departments.1-6 Iridotomy helps to prevent AACG by flattening the convex surface of the iris and widening the angle in patients with relative pupillary block. Success rates of laser iridotomy have been reported to be from 65-76%,7,8 and are relatively low in patients of east Asian descent.9
Identifying factors associated with successful laser iridotomy for patients with AACG would be quite helpful in designing a proper treatment plan for each patient after laser iridotomy.
The present research examined a sample of Korean patients with AACG with corneal edema and with IOP above 40 mmHg as there is a lower response to pilocarpine caused by the ischemia of the iris above this level of intraocular pressure (IOP).10 Therefore, it may be more difficult to perform successful laser iridotomy in these eyes and achieve appropriate IOP. Maximum tolerable medical therapy was administered to all subjects and the response to therapy and relevant clinical factors that may affect IOP control after laser iridotomy were collected and analyzed.
Materials and Methods
The subjects were selected from patients who visited CHEIL Eye Hospital during the period from June 2004 to June 2008 and presented with AACG with initial IOP above 40 mmHg at the time of visiting the hospital. Based on medical records, a retrospective review was carried out using 77 eyes of 77 patients. None of the patients included in the study had a pathological condition affecting the visual field except transient changes after acute glaucoma such as nonspecific constriction. Patients who had previously been treated for any glaucoma were excluded. Also, secondary angle-closure glaucoma such as neovascular glaucoma, lens-induced glaucoma and uveitic glaucoma were specifically excluded.
AACG was diagnosed when the eye showed an IOP more than 40 mmHg and closed angle by gonioscopy with accompanying acute symptoms including ocular pain, redness and blurred vision according to Kim and Jung's classification system.11 At the time of first visit, all patients immediately received β-blocker drops and 2% pilocarpine in the eyes, along with oral administration of a carbonic anhydrase inhibitor. Intravenous hyperosmotic agent (15% Mannitol®; Choongwae Pharmaceutical Co., Seoul, Korea) was given if the patient did not have a significant systemic disease, such as acute intra-cranial hematoma or severe congestive heart failure. Laser iridotomy was performed immediately after the resolution of corneal edema and the widening of the angle.
Laser iridotomy was performed with an argon laser (Integre-S; Ellex Medical Pty. Ltd., Adelaide, Australia) and Nd:YAG laser (YC-1800; NIDEK, Gamagori, Japan) by a single operator on all patients, in order to minimize interobserver error. 0.5% proparacaine HCl and 1% apraclonidine were dropped into the eye prior to surgery, and then an Abraham iridotomy lens was inserted into the eye to excise the superotemporal or superonasal area of the iris. The spot size of the argon laser was 50 µm, while the time, strength and frequency of the irradiation were 0.05-0.1 second, 900-1000 mW and 10-70 times, respectively. When part of the pigmented epithelium was seen or when the iris stroma was sufficiently removed for the pigmented epithelium to be exposed, Nd:YAG laser irradiation was applied 3-25 times at 2.3-3.4 mJ. The laser pointer of the argon laser was used to make sure the size of the excision area was at least 150-200 µm. After surgery, 1% apraclonidine was dropped into the eye and then 0.1% fluorometholone was administered four times a day for a week. As unaffected eyes have an approximately 50% acute angle-closure attack probability within five years,2 prophylactic laser iridotomy was performed for the other eye during the follow-up observation period.
IOP was measured by Goldmann applanation tonometer at the time of the initial hospital visit, 1-2 hours after medical therapy and one hour, one day, three days, one week, two weeks, one month and every three months after initial laser iridotomy. The success of laser iridotomy was assessed in terms of IOP, reduction rate of IOP and the necessity of additional treatment. For the purpose of analysis, an increase in IOP on follow-up was defined as an increase greater than 21 mmHg requiring medical or surgical treatment. The time intervals to increases in IOP after laser iridotomy were recorded.
We analyzed the data to detect whether there were predictive factors for development of IOP increase, such as age, sex of the patient, duration of symptoms, initial levels of IOP and pupil status. A dilated, fixed, miotic-resistant pupil was defined as a pupil greater than 7 mm in diameter and not responding to miotics and light even after IOP normalized following treatment as previously described.
Multivariate odds ratio analyses between each risk factors and the risk of subsequent increases of IOP after laser iridotomy was carried out. The confidence interval was 95% for the odds ratio and statistical significance was assumed at p<0.05.
Results
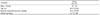
From June 2004 to June 2008, 77 eyes of 77 patients were included in this study. The mean follow-up period was 12.7 months (range, 1 to 48 months). Of the 77 patients who received laser iridotomy, 18 patients were male and 59 were female with a mean age of 66.0 years (range, 30 to 84 years). The mean duration of symptoms was 6.4 days (range, 1 to 30 days) and the mean initial IOP was 52.6 mmHg (range, 40 to 80 mmHg) (Table 1).
All patients underwent sequential argon laser and Nd: YAG laser peripheral iridotomy after maximal tolerable medical therapy and all 77 eyes achieved a patent iridotomy of sufficient size. Temporary IOP spikes were noted in three eyes after laser iridotomy (range, 22 to 32) and all cases resolved spontaneously without further treatment within a day. There were no severe complications accompanying the laser iridotomy such as retinal burn, corneal injury, hyphema and intractable inflammations.
The time interval for the subsequent increase in IOP is shown in Table 2. Forty-six of 77 eyes (59.7%) had normalized IOP on follow-up after laser iridotomy alone. Thirty-one of 77 eyes developed an increase in IOP during follow-up and most of them (30/31 eyes) presented an increased IOP within six months after laser iridotomy. In this group, 20 of 31 eyes developed an early increase in IOP within one month after laser iridotomy.
The mean IOP was 32.1±26.9 mmHg (range, 22 to 60 mmHg) in 31 eyes showing IOP increases after laser iridotomy and two eyes eventually underwent trabeculectomy in order to achieve IOP control.
We evaluated successful laser iridotomy according to the response of the maximal tolerable medical therapy given immediately upon hospital visit. The IOP of 42 of 77 eyes was reduced to more than 30% of the initial IOP, of which 39 of 42 eyes had not developed an increase in IOP during follow-up. However, in the 35 eyes presenting with less than 30% IOP reduction after maximal tolerable medical therapy, only seven of 35 eyes had not developed an increase in IOP (p=0.000) (Table 3). Forty-nine of 77 eyes were administered intravenous hyperosmotic agent treatment during maximal tolerable medical therapy and there was no IOP increase in 24 of the 49 eyes (p=0.012) on follow-up (Table 3).
We evaluated five possible predictive factors for the development of a subsequent increase in IOP requiring further treatment: age, sex of the patient, duration of symptoms, level of initial IOP and pupil status. Successful laser iridotomy was more often achieved in patients who presented within seven days (Odds ratio, 4.51; 95% confidence interval, 1.38 to 14.75). Patients who were female, older than 60 years, and had initial IOP above than 50 mmHg were found to have a greater chance of developing an increase in IOP although not statistically significant. Dilated fixed pupils were observed only in eyes presenting with an increase in IOP after laser iridotomy (p=0.000) (Table 4).
Discussion
The success rate of laser iridotomy is influenced by the length of follow-up period.12-14 Re-opening the closed angle is the major goal in the treatment of AACG. Reduction of IOP also helps to prevent further glaucomatous damage. There are several methods used to achieve re-opening including medical therapy, corneal indentation, laser iridoplasty or pupilloplasty, and laser iridotomy. If there is no response to these treatments, surgical iridectomy or trabeculectomy is indicated. Primary treatment usually starts with IOP-reducing drugs followed by laser iridotomy performed promptly once the attack has been resolved by medical therapy. In most cases, laser iridotomy relieves the AACG attack. We analyzed the predictive values of several factors for successful laser iridotomy to provide better pre-iridotomy patient assessment in the future.
The present study showed that there were no differences in the success rates of laser iridotomy according to sex, age and initial IOP which agrees with the results of research conducted by Chung et al.12 and Aung et el.13 Forty-six of 110 eyes (41.8%) in Aung et al.13, 32 of 45 eyes (71.1%) in Chung et al.12 and 46 of 77 eyes (59.7%) in the present study were treated with laser peripheral iridotomy alone with no subsequent increase in IOP at follow-up. Laser iridotomy alone is, however, not sufficient to prevent a clinically significant increase in IOP after AACG in the majority of patients of east Asian descent.13 In addition, IOP after laser iridotomy usually increases within six months in Asian eyes treated with AACG.12,13 These findings are unique in Asians.13 Several reasons have been suggested for this marked ethnic difference in IOP increases with AACG. Oh et al.15 emphasized geographical variation in the chamber angle - the iris joins the scleral wall more anteriorly in east Asians and more posteriorly in individuals of European descent. Kim and Jung11 also mentioned that creeping angle closure is not uncommon, and that anterior lens positioning without significant lens enlargement is responsible for angle-closure glaucoma in Asians. Aung et al.13 reported that Asian eyes may be prone to develop more severe attacks of acute primary angle-closure compared to Europeans, and that this may be related to the longer duration of symptoms and the difficulty of breaking the acute attack. In addition, more laser energy is needed to penetrate the iris for iridotomy performed on the thicker dark-brown irides common in Asians.13,16 The trabecular meshwork's damage and diminished outflow caused by inflammation and pigment release during laser iridotomy with higher laser energy level may ultimately cause increased IOP on follow-up.13 Therefore, it is necessary to monitor IOP closely in the first few months after AACG in order to manage subsequent increases in IOP.
The success rates were analyzed in terms of response to maximal tolerable medical therapy given immediately upon the initial hospital visit. Out of 42 eyes with more than 30% IOP reduction, the IOP of 39 patients (92.9%) were normalized with laser iridotomy alone. Of the 35 patients with lower than 30% IOP reduction, only seven eyes were satisfactorily controlled. Higher rates of successful laser iriodotomy were achieved in eyes with more than 30% reduced IOP upon maximal tolerable medical therapy (p<0.001). We considered those who showed a significant IOP reduction effect with medical therapy alone to have no significant anatomical and functional abnormalities of aqueous outflow, therefore maintaining appropriate IOP after laser iridotomy. In addition, of those patients who received intravenous Mannitol® (systemic mannitolization) as a part of medical therapy, 24 of 33 eyes (72.7%) with more than 30% reduced IOP had not developed an increase in IOP, while only five of 16 patients with less than 30% reduced IOP did not experience an increase (p=0.012). Systemic mannitolization causes a reduction in vitreous volume, thereby aiding the reduction of IOP through the angle-closure alleviation effect and pupillary block alleviation effect. We believe that this is why those patients with more than 30% IOP reduction upon systemic mannitolization showed a significantly higher success rate, since IOP was maintained appropriately after the laser iridotomy.
An increase in IOP was observed more frequently in eyes treated more than seven days after the development of symptoms. A longer duration of symptoms may cause more damages to aqueous outflow and lead to the formation of peripheral anterior synechiae (PAS).17 AACG and chronic angle-closure glaucoma are most likely to have a greater extent of PAS than patients in the angle closure hypertension or ACG suspect subtypes. In addition, synechial closure of the angle may play an important role in IOP increases in later disease stages. Such a difference is thought to increase the risk of PAS occurrence as the angle-closure glaucoma period gets longer and to cause the functional loss of aqueous humor outflow. A dilated and fixed pupil was already mentioned as a possible factor related to laser iridotomy failure due to accelerated PAS formation18 and dilated, fixed pupils were only observed in eyes presenting an increase in IOP in this study.
In conclusion, the present research demonstrates that the success rate of laser iridotomy is not related to age, sex or initial IOP. Successful laser iridotomy was achieved in eyes treated within seven days of acute symptom onset, and cases with more than 30% reduced IOP upon maximal tolerable medical therapy including systemic mannitolization had a significantly higher success rate compared to laser iridotomy alone. We believe that this result is helpful in developing treatment modalities for AACG patients.
A limitation of the present research is that it was a hospital-based retrospective study. Analyses of additional features such as the degree of distribution of the PAS and the size of the pupil at the time of attack would be helpful in future studies. Further research with long-term follow-up observation of eyes after successful laser iridotomy and with appropriate IOP control with respect to the recurrence and progression of acute angle-closure glaucoma is warranted.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download