Abstract
Purpose
To evaluate the efficacy of excision of avascular bleb and advancement of adjacent conjunctiva (EBAC) for treatment of hypotony after trabeculectomy with mitomycin C (MMC).
Methods
Fifteen patients (17 eyes) who received EBAC for correction of hypotony between September 1996 and October 2008 were reviewed retrospectively. The main outcomes were intraocular pressure (IOP) and postoperative complications.
Results
Hypotony (IOP <6 mmHg) of eight eyes (47.1%, seven patients) was caused by bleb perforation. Of these, two eyes (two patients) had a history of trauma. Hypotony appeared at 33.9±30.8 months, and EBAC was performed at 48.2±35.3 months after trabeculectomy with MMC. The mean follow-up period was 38.3±29.8 months. The qualified success rate of EBAC was 100% at 51 months after EBAC, and the complete success rate of EBAC was 76.5% at six months and 70.6% at 51 months, as determined by Kaplan-Meier analysis. Post-EBAC complications included blepharoptosis in four eyes (23.5%) and bleb perforation in one (5.9%). The blepharoptosis resolved within one month after EBAC in two patients. However, in the other patients, mild blepharoptosis remained at 17 and 22 months postoperatively.
The goal of trabeculectomy is to reduce intraocular pressure (IOP) to a level that will prevent further optic nerve damage, while avoiding complications from ocular hypotony. The adjunct use of mitomycin C (MMC) with trabeculectomy increases the likelihood of maintaining a low IOP.1 However, it also increases the incidence of complications such as shallow anterior chamber, progression of cataract, ciliochoroidal effusion, and bleb leaks.2-4 Trabeculectomy with adjunct use of MMC may have an even higher rate of late bleb leaks than those with adjunct use of 5-fluorouracil (5-FU),5,6 since trabeculectomy with MMC can produce extremely thin, avascular blebs.6
Conservative treatments associated with bleb leaks and overfiltration are usually attempted first, including aqueous suppressants, antibiotics, oversized contact lenses,7 cyanoacrylate glue,8,9 pressure patching, and autologous blood intrableb injection.10-13 However, these procedures have a limited success rate.14,15 Effective treatment of hypotony often requires surgical management,16 usually by advancement of conjunctiva from the adjacent conjunctiva and/or Tenon layers17-25 or by free conjunctival autografts.26,27 The goal of surgery is to seal bleb leaks and overfiltration while preserving a functioning filtering bleb, and several studies have reported that surgical management has a 83-96% success rate, although success was defined differently in each study.28,29
We previously reported a method of bleb revision for hypotony caused by leaking or overfiltrating blebs, in which bleb excision and advancement of the fornical conjunctiva was performed to correct hypotony in five patients. Intraocular pressure increased and visual acuity (VA) improved after operation.30 The purpose of this study was to evaluate the effects of excision of avascular bleb and advancement of adjacent conjunctiva (EBAC) for treatment of hypotony after trabeculectomy with MMC.
A retrospective review was conducted of 17 eyes (15 patients) that underwent EBAC for correction of hypotony after trabeculectomy with MMC at Chungbuk National University Hospital between September 1996 and October 2008. All patients had minimum of six months of follow-up after EBAC.
We investigated the patient medical records and noted demographic and clinical characteristics including IOP, VA, type of glaucoma, gender, age at the time of EBAC, and history of trauma and bleb perforation. Duration of trabeculectomy with MMC and hypotony and duration of trabeculectomy with MMC and EBAC were investigated. Operative and postoperative courses were noted, especially duration of follow-up, IOP, VA, bleb appearance and complications.
EBAC was performed under Nadbath's akinesia, with a sub-Tenon injection of 2% lidocaine. Anterior chamber paracentesis was placed at either the 3 or 9 o'clock position. The thinned avascular conjunctival bleb was excised. The healthy conjunctiva and Tenon capsule between the superior border of the excised bleb and the superior fornix were used to reconstruct the new bleb. One or two horizontal relaxing incisions in the fornix were made that were long enough to permit coverage of the filtration site without tension. The conjunctiva and Tenon capsule anterior to the relaxing incision were undermined, and the Tenon flap was carefully advanced to the limbus, avoiding formation of a button hole, and sutured to the limbus. Following this, the limbal margin of the conjunctival flap was sutured separately with 10-0 Nylon.
Hypotony was defined as an IOP below 6 mmHg lasting for one month or longer. EBAC was considered a complete success (CS) when the complication was resolved while maintaining an IOP ≥6 mmHg and ≤18 mmHg without the use of glaucoma medication. Qualified success (QS) was achievement of the above with glaucoma medications but with no need for reoperation for glaucoma. The date of failure was considered the first visit in which recurrence or persistence of the complication (hypotony, leaks) or IOP >18 mmHg was noted.
Statistical analysis was carried out using SPSS ver. 13.0 (SPSS Inc., Chicago, IL, USA), and a p-value less than 0.05 was considered statistically significant.
The mean age of the patients (14 men and one woman) was 41.9±14.2 years (range, 15 to 66 years). The mean time interval between trabeculectomy with MMC and occurrence of hypotony was 33.9±30.8 months with a range of 1 day to 89 months. The mean time interval between trabeculectomy with MMC and EBAC was 48.3±35.3 months (range, 0 to 89 months). Hypotony of eight eyes (47.1%) of seven patients was caused by bleb perforation; of these, two eyes in two patients had a history of trauma. Mean follow-up after EBAC was 38.3±29.8 months (range, 9 to 104 months) (Table 1). Primary open-angle glaucoma was the most common glaucoma type (nine eyes, 52.9%), followed by neovascular glaucoma (four eyes, 23.6%), pigmentary glaucoma (one eye, 5.9%), uveitic glaucoma (one eye, 5.9%), Posner-Schlossman syndrome (one eye, 5.9%), and glaucoma following ocular surgery (one eye, 5.9%) (Table 2).
The mean preoperative IOP was 2.8±2.1 mmHg, and the mean IOP at last follow-up was 12.2±3.2 mmHg (p<0.001, t-test) (Fig. 1). The mean preoperative VA (logMAR) was 1.02±1.04, and the mean VA (logMAR) at the final follow-up was 0.54±0.97 (p=0.174, t-test) (Fig. 2).
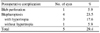
Kaplan-Meier survival analysis was used to measure the QS and CS rates of EBAC. Qualified success was obtained for all 17 eyes at 51 months follow-up, although five patients required glaucoma medication for IOP control. EBAC gave a CS rate of 76.5% at six months and 70.6% at 51 months follow-up (Fig. 3). At the final follow-up after EBAC, 12 (70.6%) of 17 eyes had thick walled blebs; and one had a partially translucent bleb. Diffuse and partially translucent blebs were maintained in three eyes (17.6%), a bleb was not maintained in one eye (5.9%) and a diffuse avascular bleb in one eye (5.9%) showed bleb perforation at 89 months after EBAC.
Complications from EBAC included blepharoptosis in four eyes (23.5%), one of which had hypertropia. Blepharoptosis of two patients without hypertropia was resolved in one month with no management. In one patient without hypertropia, mild blepharoptosis remained at the 22-month follow-up after EBAC. In one patient with hypertropia, mild blepharoptosis and hypertropia remained at 17 months after EBAC. Hypertropia was small (<10 prism diopter) and conservative management was performed. Bleb perforation was seen in one eye (5.9%) at 89 months after EBAC, and the patient underwent reoperation (Table 3). No other postoperative complications such as endophthalmitis, suprachoroidal hemorrhage, choroidal effusions, or shallow anterior chamber occurred.
Trabeculectomy is commonly conducted when medical therapy fails to control IOP. The introduction of adjunctive 5-fluorouracil (5-FU) and MMC has resulted in improvement of IOP control for eyes that had lower rates of operative accomplishment and for uncomplicated glaucoma.1,31 However, adjunctive use of MMC may cause a higher incidence of postoperative hypotony and hypotonic maculopathy.3,4
Trabeculectomy conducted with MMC may have a higher rate of bleb leaks than trabeculectomy conducted with 5-FU.6 Histopathological examination of blebs after trabeculectomy with MMC revealed irregularities in the conjunctival epithelium, breaks in the basement membrane, and conjunctival and subconjunctival hypocellularity, each of which may be a predisposing factor for bleb leaks and overfiltration.32
With managing hypotony, observation is appropriate in the absence of complications. Seah et al.33 reported that hypotony is common after trabeculectomy but usually persists for less than two weeks. Only patients with prolonged hypotony had a VA decline, suggesting that if the IOP remains below the physiological tolerance for over two months, treatment of hypotony should be attempted. Complications that increase the urgency of treatment for bleb leaks and hypotony include decline of VA with macular folds, present or previous blebitis, a shallow anterior chamber, and profound hypotony. In our study, the mean time between hypotony and EBAC was 13.6±25.0 month (range, 0 to 99 months). Seven eyes had bleb leaks, one had a decreased VA only, one had a decreased VA with a macular fold, and the others had hypotony for over two months.
Management of bleb leaks and overfiltrating blebs overlaps because both indicate excessive filtration of aqueous humor. The first treatments are usually conservative,6,10 but these have a limited success rate.14,15 When conservative management fails, surgical management is required. Dunnington and Regan17 described a series of 15 patients with either inadvertent or intentional filtering blebs who underwent conjunctival advancement for bleb leaks. Geijin et al.25 described a success rate of 86.1% for 36 patients who underwent excision of conjunctiva and advancement of conjunctiva and Tenon capsule for bleb leaks or overfiltrating bleb. The IOP increased from 4.3 mmHg to 13.5 mmHg after operation. Burnstein et al.34 compared conjunctival advancement and nonincisional treatment for filtering bleb leaks. Conjunctival advancement was more likely to control IOP effectively and was less likely to have serious complications like endophthalmitis, than was management with nonincisional treatment. We conducted EBAC in 17 eyes that had hypotony after trabeculectomy with MMC. Intraocular pressure increased from 2.8 mmHg to 12.2 mmHg at the final follow-up (p<0.001). VA (logMAR) decreased from 1.02 to 0.54 at the final follow-up, but these differences were not significant.
Budenz et al.35 compared the safety and efficacy of preserved human amniotic membrane transplants with conjunctival advancement for repair of late-onset bleb leaks. The cumulative survival for amniotic membrane transplant was 81% at six months, 74% at one year, and 46% at two years, and the cumulative survival for conjunctival advancement was 100% throughout the follow-up period. Tannenbaum et al.29 described the effect of bleb excision and conjunctival advancement for leaking or hypotonous eyes after trabeculectomy or combined operation and found that bleb excision and conjunctival advancement successfully managed leaks and hypotony. Complete success was obtained for 40% of patients and QS was obtained for 83% of patients. In our study, EBAC eliminated bleb leaks and hypotony effectively. Qualified success was 100% throughout the follow-up, and CS was 76.5% at six months and 70.6% at 51 months.
Replacement of the abnormal conjunctiva with a normal healthy conjunctiva restores the normal epithelial barrier and appears to be the most successful physiological therapy for reversing hypotony. It is relatively safe because manipulation is extraocular, and additional manipulation of the scleral flap is not needed.
Scleral patch graft or amniotic membrane transplantation could be performed for treatment of hypotony, but donor sclera or amniotic membrane may be virally contaminated, so special preservation and care are needed.36 Also, adequate donor tissue or amniotic membrane is not always available. EBAC does not require donor tissue or amniotic membrane.
Complications of EBAC are an immediate postoperative IOP spike, recurrent bleb leaks, bleb dysesthesia, bleb failure, hypertropia and blepharoptosis.24,28-30,34 We found that surgery can cause adverse events, but they were uncommon. We experienced four cases of blepharoptosis and one case of bleb perforation. One case of blepharoptosis was combined with small hypertropia. Two cases of blepharoptosis resolved in 2 months after EBAC. In the other cases, blepharoptosis improved, although mild blepharoptosis remained. Blepharoptosis and hypertropia were probably due to tension from an insufficient relaxing incision in the fornix.
Some studies report that initial VA is often not restored in some hypotony patients, despite treatment. Prolonged hypotony is thought to cause irreversible chorioretinal folds from fibrosis within the retina, choroids, or sclera.4 In our study, three eyes from two patients had no restoration of preoperative VA. Neovascular glaucoma due to proliferative diabetic retinopathy was present in one patient and Eales' disease in the other.
Generally, hypotony has numerous complications, and prevention is the best treatment. We were able to obtain proper control of IOP and maintenance of initial VA without serious complications. In conclusion, EBAC was an effective and safe procedure for treatment of hypotony after trabeculectomy with MMC.
Figures and Tables
Fig. 1
Scatter plot of preoperative intraocular pressure (IOP) and IOP at final follow-up. Mean preoperative IOP was 2.8±2.1 mmHg and mean IOP at final follow-up was 12.2±3.2 mmHg. IOP was significantly higher at final follow-up (p<0.001, t-test).
EBAC=excision of avascular bleb and advancement of adjacent conjunctiva.

Fig. 2
Scatter plot of preoperative visual acuity (VA) and VA at final follow-up. Mean preoperative VA (logMAR) was 1.02±1.04 and mean VA (logMAR) at final follow-up was 0.54±0.97. Differences were not significant (p=0.243, t-test).
EBAC=excision of avascular bleb and advancement of adjacent conjunctiva.

Fig. 3
Kaplan-Meier analysis of success rate of excision of avascular bleb and advancement of adjacent conjunctiva. Criteria for complete success were intraocular pressure (IOP) ≥6 mmHg and ≤18 mmHg with the use of no glaucoma medications. Criteria for qualified success were the same as that for complete success but with use of glaucoma medication to control IOP.
Notes
References
1. Robin AL, Ramakrishnan R, Krishnadas R, et al. A long-term dose-response study of mitomycin in glaucoma filtering surgery. Arch Ophthalmol. 1997. 115:969–974.
2. Kitizawa Y, Kawase K, Matsushita H, Monobe M. Trabeculectomy with mitomycin: a comparative study with fluorouracil. Arch Ophthalmol. 1991. 109:1693–1698.
3. Whiteside-Michel J, Liebmann JM, Ritch R. Initial 5-fluorouracil trabeculectomy in young patients. Ophthalmology. 1992. 99:7–13.
4. Stamper RL, Mcmeneny MG, Lieberman MF. Hypotonous maculopathy after trabeculectomy with subconjunctival 5-fluorouracil. Am J Ophthalmol. 1992. 113:544–553.
5. Skuta GL, Beeson CC, Higginbotham EJ. Intraoperative mitomycin versus postoperative 5-fluorouracil in high risk glaucoma filtering surgery. Ophthalmology. 1992. 99:438–444.
6. Greenfield DS, Liebmann JM, Jee J, Ritch R. Late-onset bleb leaks after glaucoma filtering surgery. Arch Ophthalmol. 1998. 116:443–447.
7. Blok MD, Kok JH, van Mil C, et al. Use of the Megasoft Bandage Lens for treatment of complications after trabeculectomy. Am J Ophthalmol. 1990. 110:264–268.
8. Awan KJ, Spaeth PG. Use of isobutyl-2-cyanoacrylate tissue adhesive in the repair of conjunctival fistula in filtering procedures for glaucoma. Ann Ophthalmol. 1974. 6:851–853.
9. Zalta AH, Wieder RH. Closure of leaking filtering blebs with cyanoacrylate tissue adhesive. Br J Ophthalmol. 1991. 75:170–173.
10. Azuara-Blanco A, Katz LJ. Dysfunctional filtering blebs. Surv Ophthalmol. 1998. 43:93–126.
11. Leen MM, Moster MR, Katz LJ, et al. Management of overfiltering and leaking blebs with autologous blood injection. Arch Ophthalmol. 1995. 113:1050–1055.
12. Wise JB. Treatment of chronic postfiltration hypotony by intrableb injection of autologous blood. Arch Ophthalmol. 1993. 111:827–830.
13. Choundri SA, Herndon LW, Damji KF, et al. Efficacy of autologous blood injection for treating overfiltering or leaking blebs after glaucoma surgery. Am J Ophthalmol. 1997. 123:554–555.
14. Matsuo H, Tomidokoro A, Tomita G, Araie M. Topical application of autologous serum for the treatment of late-onset aqueous oozing or point-leaking through filtering bleb. Eye. 2005. 19:23–28.
15. Burnstein A, WuDunn D, Ishii Y, Jonescu-Cuypers C, Cantor LB. Autologous blood injection for late-onset filtering bleb leaks. Am J Ophthalmol. 2001. 132:36–40.
16. Ritch R, Schuman JS, Belcher CD III. Cases in controversy: management of the leaking filtration bleb. J Glaucoma. 1993. 2:114–118.
17. Dunnington JH, Regan EF. Late fistulization of operative wounds. Arch Ophthalmol. 1950. 43:407–418.
18. Sugar HS. Complications, repair and reoperation of antiglaucoma filtering blebs. Am J Ophthalmol. 1967. 63:825–833.
19. McCulloch C. Surgery of filtering blebs. Int Ophthalmol Clin. 1967. 7:125–134.
20. Cohen JS, Shaffer RN, Hetherington J, Hoskins D. Revision of filtration surgery. Arch Ophthalmol. 1977. 95:1612–1615.
21. Galin MA, Hung PT. Surgical repair of leaking blebs. Am J Ophthalmol. 1977. 83:328–333.
22. Wilensky JT. Management of late bleb leaks following glaucoma filtering surgery. Trans Am Ophthalmol Soc. 1992. 90:161–168.
23. O'Connor DJ, Tressler CS, Caprioli J. A surgical method to repair leaking filtering blebs. Ophthalmic Surg. 1992. 23:336–338.
24. Budenz DL, Chen PP, Weaver YK. Conjunctival advancement for late-onset filtering bleb leaks: indications and outcomes. Arch Ophthalmol. 1999. 117:1014–1019.
25. van de Geijin EJ, Lemij HG, de Vries J, de Waard PW. Surgical revision of filtration blebs: a follow-up study. J Glaucoma. 2002. 11:300–305.
26. Buxton JN, Lavery KT, Liebmann JM, et al. Reconstruction of filtering blebs with free conjunctival autografts. Ophthalmology. 1994. 101:635–639.
27. Wilson MR, Kotas-Neumann R. Free conjunctival patch for repair of persistent late bleb leak. Am J Ophthalmol. 1994. 117:569–574.
28. Wadhwani RA, Bellows AR, Hutchinson BT. Surgical repair of leaking filtering blebs. Ophthalmology. 2000. 107:1681–1687.
29. Tannenbaum DP, Hoffman D, Greaney MJ, Caprioli J. Outcome of bleb excision and conjunctival advancement for leaking or hypotonous eyes after glaucoma filtering surgery. Br J Ophthalmol. 2004. 88:99–103.
30. Hyung SM, Ahn DG. Midterm follow-up of necrotic bleb excision and advancement of the fornical conjunctiva. Korean J Ophthalmol. 1999. 13:85–91.
31. Katz GJ, Higginbotham EJ, Litcher PR, et al. Mitomycin C versus 5-fluorouracil in high-risk glaucoma filtering surgery: extended follow-up. Ophthalmology. 1995. 102:1263–1269.
32. Shields MB, Scroggs MW, Sloop MW, Simmons RB. Clinical and histopathological observations concerning hypotony after trabeculectomy with adjunctive mitomycin-C. Am J Ophthalmol. 1993. 116:673–683.
33. Seah SKL, Prata JA Jr, Minckler DS, et al. Hypotony following trabeculectomy. J Glaucoma. 1995. 4:73–79.
34. Burnstein AL, Wudunn D, Knotts SL, et al. Conjunctival advancement versus nonincisonal treatment for late-onset glaucoma filtering bleb leaks. Ophthalmology. 2002. 109:71–75.
35. Budenz DL, Barton K, Tseng SC. Amniotic membrane transplantation for repair of leaking glaucoma filtering blebs. Am J Ophthalmol. 2000. 130:580–588.
36. Mehta JS, Franks WA. The sclera, the prion, and the ophthalmologist. Br J Ophthalmol. 2002. 86:587–592.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download