Abstract
Purpose
To compare the success rates and stabilities of postoperative alignment between adjustable and the non-adjustable surgeries in the treatment of sensory exotropia.
Methods
A retrospective analysis was performed on all patients with sensory exotropia who had undergone unilateral lateral rectus recession and medial rectus resection (R&R) between January 1998 and August 2005. Thirty-four patients underwent conventional R&R, and 20 patients underwent R&R with adjustable suture of the lateral rectus. The surgical results between the two groups were analyzed with regard to the preoperative and post-operative deviation angles and the postoperative drift. The postoperative deviation angle was measured on postoperative day 1 as well as at two weeks, three months, six months and the final visit after surgery.
Results
There were no statistically significant differences in the mean preoperative and postoperative deviation angles between the two groups. In 30 (88%) patients in the non-adjustable group and 15 (75%) patients in the adjustable group, postoperative deviation was less than 15 prism diopters (PD) at the three month follow-up. There was no significant difference in the mean postoperative drift between the two groups.
Conclusions
Strabismus surgery with adjustable sutures did not show a significantly better result than surgery without adjustable sutures in the treatment of sensory exotropia. Considering the amount of postoperative exodrift in both groups, we postulate that the immediate ocular alignment after surgery for sensory exotropia should be orthophoric or 5-6 PD of esodeviation.
The adjustable suture surgical technique was introduced to afford the surgeon the opportunity to place the eye in a desired position within a few hours of surgery.1-4 In 1975, Jampolsky described a two-stage adjustable technique with surgery under general anesthesia and later adjustment of the ocular position under local anesthesia. This was easy to perform and its usage has been increasing.4-8 The adjustable suture technique can reduce immediate over-or undercorrection after surgery and is recommended in cases for which unpredictable surgical results are expected.5 It is a two-stage procedure, however, which prolongs the surgical time and can be uncomfortable and even painful for patients.6,7,9 In addition, it does not guarantee long-term alignment after the surgery.6,7 Therefore, we proposed that surgeons should only choose the adjustable-suture technique when there is conclusive evidence of advantage to the patient in treatment of their strabismus.
The purpose of this study was to compare the success rates and the long-term stabilities in postoperative alignment between adjustable and the non-adjustable surgeries in the treatment of sensory exotropia.
Medical records were reviewed from 178 patients with sensory exotropia who had undergone strabismus surgery between January 1998 and August 2005. All of the patients included in the study had constant exodeviation and had been diagnosed with sensory exotropia. Patients with cranial nerve palsies, thyroid eye disease, previous strabismus surgery, restrictive strabismus or co-existing vertical strabismus were excluded.
Overall, 54 patients met the criteria for inclusion in this study. The differences between the conventional and adjustable surgeries were explained to each patient, and they were free to choose their preferred method. Thirty-four patients elected to undergo non-adjustable unilateral lateral rectus recession and medial rectus resection (group 1), and twenty patients underwent unilateral medial rectus muscle resection and adjustable lateral rectus muscle recession with the Jampolsky method (group 2).
Data collected from the medical records included patient's age, gender, visual acuity, preoperative and postoperative deviation angles, the amount of postoperative drift, and the amount of resection and recession. The deviation angles were measured in the primary position at 33 cm using the modified Krimsky method before surgery and at postoperative day 1 as well as at two weeks, three months, six months and at the final follow-up visit after surgery.
All surgeries were performed by one author (JYK). In the adjustable group (group 2), the surgical procedure consisted of a conventional medial rectus muscle resection followed by a lateral rectus muscle recession using an adjustable hang-back suture; the adjustment procedure was then performed several hours after surgery in a surgical room. The goal of adjustment was to achieve orthophoria at the near point. The target angle for conventional R&R was also orthophoria at the near point. The amounts of resection and recession for a given deviation were derived from standard strabismus tables.10
All patients underwent a minimum of three months of follow-up and 69% of patients underwent six or more months of follow-up. We defined postoperative drift as the difference between the deviation angle at the final visit and the deviation angle on postoperative day 1. A successful outcome was defined as having an alignment within 15 PD of orthophoria at the near point.
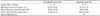
Table 1 shows descriptive data for the 54 patients in this study. The mean ages of the patients were 23 years (range, 6 to 59 years) in group 1 and 24 years (range, 12 to 42 years) in group 2. The mean preoperative deviation angles were 39.9 PD (range, 20 to 60 PD) in group 1 and 38.8 PD (range, 20 to 50 PD) in group 2. There was no difference in preoperative deviation angle between the two groups (t-test, p>0.05). Eight (40%) patients in group 2 required postoperative adjustment. Six patients underwent postoperative adjustments for overcorrection and two patients underwent adjustments for undercorrection. The average durations of postoperative follow-up were 16.1 months (range, 6 months to 5 years) in group 1 and 20.9 months (range, 6 months to 10 years) in group 2.
Fig. 1 illustrates the course of the mean postoperative deviation angle during follow-up. In group 1, the mean deviation angle changed from 1.6 PD of esodeviation at postoperative day 1 to 3.9 PD of exodeviation at the final follow- up. In group 2, the mean deviation angle changed from 2.9 PD of exodeviation to 8.1 PD of exodeviation. There were no statistically significant differences in mean postoperative deviation angles during follow-up between the two groups (p>0.05).
In group 1, the mean postoperative drift values were 5.1±8.6 PD (median value, 5 PD; 95% confidence interval [CI], 1.9 to 8.3) in group 1 and 5.3±8.8 PD (median value, 5 PD; 95% CI, 0.2 to 10.3) in group 2. The success rates after strabismus surgery were 88% in group 1 and 75% in group 2. There was no statistically significant difference in success rate between the two groups (Fisher's exact test, p=0.47).
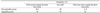
Table 2 demonstrates the final drift patterns and probabilities based on measurements at the final follow-up examinations. In group 1, 13 (38.2%) patients showed exo-drift (postoperative drift toward the original deviation), 17 (50%) patients showed zero-drift (postoperative drift within 5 PD of postoperative alignment) and four (11.8%) patients showed eso-drift (postoperative drift away from the original deviation). In group 2, nine (45%) patients showed exo-drift, nine (45%) patients showed zero-drift and two (10%) patients showed eso-drift.
Although we attempted to study the influence of other clinical factors on surgical outcome, final postoperative deviation was not found to be significantly influenced by patient's age, gender, preoperative deviation angle or selection of the adjustable procedure (Table 3).
In this study, the success rates and stabilities of postoperative alignment between the adjustable and non-adjustable surgeries in the treatment of sensory exotropia were compared. Our data suggests that, when compared to surgery without adjustable sutures, strabismus surgery with adjustable sutures is not associated with either a statistically significant higher success rate or less postoperative drift in the treatment of sensory exotropia.
There are relatively few studies directly comparing the results of the adjustable suture technique to those of traditional non-adjustable surgery.7,11 Our results correspond with an earlier study by Bishop and Doran7 which reported the success rates of adjustable and non-adjustable surgeries to be 81% and 88%, respectively. In horizontal strabismus, Mohan et al.11 have shown no significant difference in success rates between the two methods. The subjects of these studies,7,11 however, represented various subtypes of strabismus including esotropia, cranial nerve palsies and patients with a history of strabismus surgery on both horizontal and vertical muscles. In order to reduce the heterogeneity of our patients, our study focused only on patients with sensory exotropia without previous strabismus surgery. In this study, the success rates for the adjustable and non-adjustable groups were 75% and 88%, respectively. There was no significant difference in the success rates between the two groups.
These findings are in contrast to the results of Tripathi et al.8 which reported that strabismus surgery with adjustable sutures had significant better final results than surgery without adjustable sutures. They reported the re-operation rates for adjustable and non-adjustable surgeries to be 8.5% and 27.2%, respectively. However, they did not mention preoperative and postoperative deviation angles or postoperative drift. Therefore, we question whether a simple direct comparison of re-operation rates can be used as an indicator of successful outcome.
Eight (40%) patients in the adjustable group underwent postoperative adjustment. According to other published data, the rate of adjustment is usually between 39 and 50%.4,7,12-14 Although measurements of deviation angles are less accurate for patients with sensory exotropia, the surgical outcomes in our study were predictable considering that our rate of adjustment was at the lower end of the range. The postoperative drifts in our study were similar to those published by others.4,7,12,15 Bishop and Doran7 reported a 9.6 PD drift after adjustable surgery and an 8.8 PD drift after nonadjustable surgery at the three-month follow-up. Weston et al.4 have reported a 4.8 PD drift after the first operation and a 4.1 PD drift after the second adjustable surgery for exotopia. Park et al.15 reported average postoperative drifts of 4.26 PD in exotropic patients and 7.5 PD in exotropic patients after adjustable surgery. In our study, the postoperative drifts in the adjustable and non-adjustable group were 5.3 PD and 5.1 PD, respectively, at an 18-month follow-up. There was no significant difference in postoperative drift between the two groups.
We were interested in the unexpected equivalent means and median postoperative drifts when comparing the two groups. Based on these similar drift patterns, we recommend a 5 PD esotropic position as the postoperative target for sensory exotropic patients in order to obtain optimal long-term alignment regardless of surgical technique.
We were unable to demonstrate either a greater success rate or less postoperative drift with adjustable strabismus surgery in our study. In fact, our success rate with adjustable surgery was even lower than that of non-adjustable surgery. However, these results can only be generalized to patients with uncomplicated sensory exotropia. Furthermore, a much larger prospective study would be required to detect a statistically significant difference in results.
References
1. Rosenbaum AL. The use of adjustable suture procedures in strabismus surgery. Am Orthopt J. 1978. 28:88–94.
2. Wisnicki HJ, Repka MX, Guyton DL. Reoperation rate in adjustable strabismus surgery. J Pediatr Ophthalmol Strabismus. 1988. 25:112–114.
3. Lennerstrand G. Adjustable sutures in strabismus surgery: a follow-up study. Acta Ophthalmol. 1982. 60:717–728.
4. Weston B, Enzenauer RW, Kraft SP, Gayowsky GR. Stability of the postoperative alignment in adjustable-suture strabismus surgery. J Pediatr Ophthalmol Strabismus. 1991. 28:206–211.
5. Jampolsky A. Current techniques of adjustable strabismus surgery. J Pediatr Ophthalmol Strabismus. 1979. 88:406–418.
6. Hertle RW. Clinical characteristics of surgically treated adult strabismus. J Pediatr Ophthalmol Strabismus. 1998. 35:138–145.
7. Bishop F, Doran RM. Adjustable and non-adjustable strabismus surgery: a retrospective case-matched study. Strabismus. 2004. 12:3–11.
8. Tripathi A, Haslett R, Marsh IB. Strabismus surgery: adjustable sutures-good for all? Eye. 2003. 17:739–742.
9. Walters G, Stewart OG. Bradbury JA. The use of subtenon ropivacaine in managing strabismus with adjustable sutures. J AAPOS. 2001. 5:95–97.
10. Parks MM, Mitchell P. Duane TD, Jaeger EA, Tasman W, editors. Concomitant exodeviations. Clinical Ophthalmology. 1988. v. 1:revised ed. Philadelphia: Harper & Row;chap. 13.
11. Mohan K, Ram J, Sharma A. Comparison between adjustable and non-adjustable hang-back muscle recession for concomitant exotropia. Indian J Ophthalmol. 1998. 46:21–24.
12. Keech RV, Scott WE, Christensen LE. Adjustable suture strabismus surgery. J Pediatr Ophthalmol Strabismus. 1987. 24:97–102.
13. Eino D, Kraft SP. Postoperative drifts after adjustable surgery. Can J Ophthalmol. 1997. 32:163–169.
14. Pratt-Johnson JA. Adjustable suture strabismus surgery: a review of 255 consecutive cases. Can J Ophthalmol. 1985. 20:105–109.
15. Park HY, Jung SK, Nam KR. Surgical results of adjustable strabismus surgery in horizontal rectus muscles. J Korean Ophthalmol Soc. 1996. 37:1335–1341.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download