Abstract
Purpose
To evaluate the effectiveness of tramadol for the reduction of pain in panretinal photocoagulation (PRP).
Methods
A double-masked randomized controlled study was performed. Fifty-eight eyes in 29 patients with proliferative diabetic retinopathy were enrolled. The eyes of the patients were randomized into two groups. Group A received an empty capsule. Group B received an oral intake of 100 mg tramadol. The capsule used in Group A had the same appearance as that used in Group B. Pain during PRP was assessed using a visual analog scale. Vital signs, including blood pressure and heart rate, were measured.
Results
The mean pain scores for groups A and B were 4.80±2.10 and 3.83±1.82 (p=0.09). There were no significant differences in the mean pain scores between the two groups. More patients in group A complained of greater pain than moderate intensity (visual analogue scale=4). Systemic blood pressure increased significantly in group A after laser treatment. However, there were no significant differences in the diastolic blood pressure changes between the two groups. We found no statistical correlation in the heart rate changes.
Diabetic retinopathy remains the most common cause of blindness in the working age population in the developed world. Findings from the Diabetic Retinopathy Study (DRS) established that panretinal photocoagulation (PRP) is an effective treatment for reducing severe visual loss in patients with proliferative diabetic retinopathy.1 However, most patients experience pain during PRP.2-4 Intolerance to laser treatment can be increased because of pain.2 Therefore, steps are needed to reduce pain during PRP.
Retrobulbar anesthesia is an effective way to block pain sensation. However, it is invasive, has potential complications, and is difficult to apply in an outpatient room.5 Intramuscular administration of anesthetic agents can be effective, but some patients have a phobia for injections. Oral analgesia is widely used in other areas of pain control. Analgesia can reduce pain by the sustained excitation of dorsal horn neurons. Pain may be eliminated or reduced if the afferent barrage is prevented or reduced from reaching the CNS by either a pre-injury neuronal block with local anesthetics or the use of other analgesics prior to a nociceptive input.6,7
Tramadol is an atypical opioid that is used to treat moderate and severe pain. The mechanism of action of tramadol is not yet fully understood, but it is believed to work through the modulation of the GABAergic, noradrenergic, and serotonergic systems. In addition, tramadol is a mild µ-opioid receptor agonist. As with many opioids, tramadol has the ability to create dependence, but this risk is lower than with traditional opioids.
The effects of tramadol on pain reduction during PRP have not yet been studied. In this study, we evaluated the analgesic effects of tramadol for pain relief during PRP in patients with proliferative diabetic retinopathy.
A prospective, double masked, randomized, case-controlled study was conducted in the department of ophthalmology of Hanyang University Guri Hospital. Data from the patients was collected between April 2007 and December 2007. Informed consent was obtained from all patients prior to their participation. The Ethical Committee of the Hanyang University Guri Hospital approved all methodologies. Patients with proliferative diabetic retinopathy and no previous history of PRP were included. Patients were excluded from the study if they had a history of hypersensitivity or contraindication to tramadol, a significant psychiatric disorder, a history of previous PRP, or the current use of any analgesic medications (for example, rheumatoid arthritis or malignancy). Demographic data, diabetes mellitus (DM) status, duration of DM, and the presence of hypertension were also recorded.
One eye from each patient was randomized to a treatment group. A control group was created using the fellow eye of same patient. Group A received an empty capsule. This capsule had the same appearance as that used in group B. Group B received an oral intake of low dose (100 mg) tramadol (Tridol®; Yuhan corporation, Seoul, Korea). The medication was administered one hour prior to the panretinal photocoagulation procedure.
The pupils were dilated using 1% tropicamide (1% Mydiacyl®; Alcon Laboratories, Hunenberg, Switzerland). One hour later, a drop of proparacaine hydrochloride 0.5% (Alcaine®; Alcon Laboratories) was applied to each eye for corneal anesthesia prior to application of the fundus contact lens (Transequator®; Volk Optical, Mentor, OH, USA). Laser treatment using an argon green laser (Novus Omni® ; Coherent, Palo Alto, CA, USA) was performed by the second researcher. The treatment guidelines were standardized, as recommended by the Early Treatment Diabetic Retinopathy Study.8 The study involved a total of 800-1600 burns. The parameters for the burns consisted of a 400 µm spot size and 0.15 second pulse duration, attempting a moderately white burn avoiding the horizontal midlines. The areas were treated in the following order: inferior, nasal, superior, and temporal.
Visual acuity and intraocular pressure were measured prior to the laser treatment. Blood pressure and heart rate were recorded with a digital monitor just before, during, and immediately after the laser treatment.
A visual analog scale (VAS), consisting of a 10 cm scale labeled with numbers from 0 to 10, was used to determine the intensity of the pain. The blinded examiner instructed patients that 0 represents experiencing no pain and 10 represents experiencing the maximum pain they could imagine. The general analgesic effects of tramadol during laser photocoagulation were studied in each of the three groups. Changes in vital signs were monitored and recorded, and the severities of the pain among the areas where the laser was applied were recorded.
Statistical computations were performed using SPSS ver. 11.0 (SPSS Inc., Chicago, IL, USA). A p-value of less than 0.05 was considered statistically significant.
Twenty-six eyes from 13 patients with proliferative diabetic retinopathy were studied, with a total of 32 cases in group A and 24 in group B. The mean age of the patients was 52.90±8.08 years, with a range of 34 to 72 years. All of the patients had type II diabetes. The duration of diabetes history ranged from 1 to 20 years, with a mean of 11.19±6.16 years. Thirteen patients had a history of hypertension and were taking oral systemic anti-hypertension drugs. Histories of other ocular diseases were not reported, except for refractive errors.
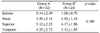
There were no significant differences in the mean pain scores between the two treatment groups. The mean pain scores for group A and B were 4.80±2.20 and 3.83±1.82 (p=0.09) (Table 1). In group A, 22 of 32 (68.7%) patients felt more severe pain (VAS>4), as compared to the placebo group. In group B, 9 of 24 (37.5%) patients felt more severe pain, as compared to the placebo group (Table 2). Pain score results for the retinal areas where the laser was applied are summarized on Table 3.
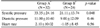
Systolic and diastolic blood pressures increased after laser treatment in all of the groups (Table 4). The increases in these pressures in the placebo group were 33.35±24.16 mmHg and 11.00±10.60 mmHg, respectively. An increase of 21.11±13.74 in the systolic pressure, and 9.00±12.09 in the diastolic pressure, was noted in group B. A significant difference in the change of systolic blood pressure between the two groups (p=0.048) was noted.
We found a decrease in the heart rate for patients in group B. The mean changes in the heart rate for patients in group A and B were 2.10±10.02 and -1.05±8.45, respectively. There was no statistical correlation in the heart rate changes between the two groups.
Pain experienced during laser therapy varies, but can be a serious complication for some patients. In this study, 31 of 56 patients reported more severe pain (VAS>4), indicating that PRP is a painful ophthalmic procedure. These findings are similar to those in other studies.2,4,9
This study evaluated the analgesic effects of tramadol during PRP. Tramadol is an analgesic widely used to relieve moderate to moderately severe pain. Tramadol is more effective than acetaminophen and other non-steroidal anti-inflammatory drugs (NSAIDs) for pain relief but is considered less effective than opioids. The mechanism of action for tramadol involves inhibiting the reuptake of serotonin and norepinephrine, as well as exhibiting a weak µ-agonist activity.10 The advantages of tramadol include a relative lack of respiratory depression, low risk of major organ toxicity, little depression of gastrointestinal motility, and a low potential for abuse.11-13 Common side effects (overall incidence of 1.6% to 6.1%) include dizziness, drowsiness, sweating, nausea, vomiting, dry mouth, and headache. No differences in pain relief between the placebo and tramadol groups during PRP were found in this study. However, there were fewer patients in the tramadol group who felt more severe pain (VAS>4). and tramadol was effective in mitigating the rise in systolic blood pressure.
Controversy over the most effective method of pain control during PRP persists. NSAIDs can relieve pain by inhibiting cyclooxygenase enzyme activity and, thus, block the formation of endogenous prostaglandins. Ocular administration of 0.5% ketorolac tromethamie ophthalmic solution is a useful analgesic drug which reduces prostaglandin E2 levels in the aqueous humor.14 NSAIDs can be used to treat pain after other ocular surgeries, such as photorefractive keratectomy,15 radial keratotomy,16 and posterior segment surgery.17 Sodium diclofenac 0.1% is effective in reducing pain during PRP, as compared with a placebo.4 However, Esgin and Samut.5 reported that the analgesic effects of topical ketorolac 0.5% were not different than an artificial tear drop during posterior segment laser photocoagulation.
Paracetamol is a widely used and effective analgesic. However, pre-emptive analgesia with paracetamol did not significantly reduce the pain associated with panretinal photocoagulation.18 Wu et al.9 evaluated the analgesic effects of acetaminophen and found that acetaminophen is not effective for pain control.
Retrobulbar and peribulbar anesthesia, on the other hand, have been known to be effective for pain relief,9 although both are invasive and can result in vision-threatening complications, including perforation and infection. Subtenon anesthesia is another method that has fewer risks, as compared to retrobulbar and peribulbar anesthesia. Unfortunately, subtenon anesthesia is also dangerous to patients, although no-needle, one-quadrant subtenon anesthesia during PRP is possible.3 Stevens argued that this method can provide effective anesthesia during panretinal photocoagulation and avoids the risks of using a sharp needle.
Entonox gas, a mixture of 50% nitrous oxide and 50% oxygen, can also be used to reduce pain during PRP.2 Ho wever, in practice, Entonox gas is difficult to use, requirin g a large amount of equipment and space.
There were some limitations to this study. First, the sample size was small, and the number of patients in each group was not the same. Second, the blinded examiner who evaluated the visual analog scales from the patients was not one person. This could be a source of bias. Third, although most of the laser parameters were the same, the number of laser treatments was different for each patient.
PRP is a painful procedure for most patients and can cause changes in vital signs, including blood pressure and heart rate. In this study no evidence that tramadol is effective for pain relief during PRP was found. However, this study showed that tramadol is more effective than a placebo for relieving more severe pain and is also effective in stabilizing vital signs, such as systolic blood pressure. Further studies are needed to evaluate pain control during PRP.
Figures and Tables
References
1. The Diabetic Retinopathy Study Research Group. Photocoagulation treatment of proliferative diabetic retinopathy: clinical application of Diabetic Retinopathy Study. DRS report number 8. Ophthalmology. 1981. 88:583–600.
2. Cook HL, Newsom RS, Mensah E, et al. Entonox as an analgesic agent during panretinal photocoagulation. Br J Ophthalmol. 2002. 86:1107–1108.
3. Stevens JD, Foss AJ, Hamilton AM. No-needle one-quadrant stubtenon anasethesia for panretinal photocoagulation. Eye. 1993. 7:768–771.
4. Weinberger D, Ron Y, Lichter H, et al. Analgesic effect of topical sodium, diclofenac 0.1% drops during retinal laser photocoagulation. Br J Ophthalmol. 2000. 84:135–137.
5. Esgin H, Samut HS. Topical ketorolac 0.5% for ocular pain relief during scatter laser photocoagulation with 532nm green laser. J Ocul Pharmacol Ther. 2006. 22:460–464.
6. Wall PD. The prevention of postoperative pain. Pain. 1988. 33:289–290.
7. Dahl JB, Kehlet H. The value of pre-emptive analgesia in the treatment of post-operative pain. Br J Anaesth. 1993. 70:434–439.
8. Early Treatment Diabetic Retinopathy Study Research Group. Early photocoagulation for diabetic retinopathy: ETDRS report number 9. Ophthalmology. 1991. 98:766–785.
9. Wu WC, Hsu KH, Chen TL, et al. Interventions for relieving pain associated with panretinal photocoagulation: a prospective randomized trial. Eye. 2006. 20:712–719.
10. Miller RD, editor. Miller's Anesthesia. 2005. 6th ed. Philadelphia: Elsevier/Churchill Livingstone;2736–2737.
11. Scott LJ, Perry CM. Tramadol: a review of its use in perioperative pain. Drugs. 2000. 60:139–176.
12. Budd K, Langford R. Tramadol revisited. Br J Anaesth. 1999. 82:493–495.
13. Wilder-Smith CH, Hill L, Wilkins J, et al. Effects of morphine and tramadol on somatic and visceral sensory function and gastrointestinal motility after abdominal surgery. Anesthesiology. 1999. 91:639–647.
14. Nichols J, Snyder RW. Topical nonsteroidal anti-inflammatory agents in ophthalmology. Curr Opin Ophthalmol. 1998. 9:40–44.
15. Rajpal RK, Cooperman BB. Analgesic efficacy and safety of ketorolac after photorefractive keratectomy: Ketorolac Study Group. J Refract Surg. 1999. 15:661–667.
16. McDonald MB, Brint SF, Caplan DI, et al. Comparison of ketorolac tromethamine, diclofenac sodium, and moist drops for ocular pain after radial keratotomy. J Cataract Refract Surg. 1999. 25:1097–1108.
17. Lesnoni G, Coppe AM, Manni G, et al. Analgesic effect of topical diclofenac versus betamethasone after posterior segment surgery. Retina. 1995. 15:34–36.
18. Vaideanu D, Taylor P, McAndrew P, et al. Double masked randomized controlled trial to assess the effectiveness of paracetamol in reducing pain in panretinal photocoagulation. Br J Ophthalmol. 2006. 90:713–717.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download