Abstract
Purpose
To investigate the degree of reunion in rabbit eyes of the superior oblique tendon after several surgical weakening procedures.
Methods
A total of 32 rabbits (64 eyes) were used in this study. The rabbits were randomly assigned to four groups, eight rabbits (16 eyes) in the tenotomy group, eight rabbits (16 eyes) in the tenectomy group, eight rabbits (16 eyes) in the disinsertion group and eight rabbits (16 eyes) in the recession group. The degree of reunion or reattachment of the superior oblique tendon on the globe were examined on four eyes in each group at postoperative weeks two, four, six and eight.
Results
At eight weeks, the newly created insertion site remained at the same site in all eyes in the recession group, and the distal end of the superior oblique tendon was reattached at the medial border of the superior rectus muscle in all four eyes in the tenotomy and disinsertion groups, and in three of four eyes in the tenectomy group.
Conclusions
From this experimental study, it was speculated that superior oblique recession is more effective than other superior oblique weakening procedures. This result could be helpful in the prediction of time of recurrence for superior oblique overaction after superior oblique weakening procedures.
Various kinds of superior oblique (SO) weakening procedures such as tenotomy, tenectomy and recession are performed for surgical correction of superior oblique overaction.1-7
In performing superior oblique tenotomy or tenectomy, there is no risk of complication such as scleral perforation; however, recurrence of superior overaction can be seen during follow-up due to reconnection of the cut tendon ends after surgery.3,6,8,9
Recession of the SO muscle is a more controlled and reliable procedure due to graded recession according to superior oblique overaction. However, a major disadvantage of this procedure is the changing of the SO muscle function of depression into one of elevation after creation of a new insertion point located along the equator rather than the anterior portion of the globe.10-15
Recently, a procedure for weakening the SO muscle by lengthening of the tendon with a silicone band has been developed.16-18 The authors performed four methods for weakening the SO muscle of rabbits and analyzed the degrees of reunion of the SO muscle according to each surgical method.
A total of 32 white, New Zealand rabbits (64 eyes) were used in this study.
The subjects were randomly assigned to four groups depending on the type of SO weakening procedure used: eight rabbits (16 eyes) in the tenotomy group, eight rabbits (16 eyes) in the tenectomy group, eight rabbits (16 eyes) in the disinsertion group and eight rabbits (16 eyes) in the recession group.
General anesthesia was attained with intramuscularly administered ketamine HCL (25 mg/kg) and xylazine HCL (10 mg/kg). During each operation, a conjunctival incision was made radial to the corneoscleral limbus along the medial side of the superior rectus (SR) insertion. Then, separation of the SR and SO was carefully performed, and the SO tendon was exposed near the nasal border of the SR by a muscle hook under direct visualization.
In the disinsertion group, disinsertion of the SO was performed, and careful dissection of the tendon capsule, and separation of the SR from the SO was done. In the tenotomy group, the SO tendon was exposed on a muscle hook under direct visualization near the nasal border of the SR. After assuring that the entire tendon was hooked, it was then transected at 2 mm nasal to the nasal border of the SR insertion. In the tenectomy group, the SO was transected at about 4 mm from the nasal side of the nasal border of the SR insertion. In the recession group, the SO tendon was disinserted, passed under the SR, and a 6-0 vicryl suture was secured in the tendon. The tendon was then sutured to the sclera at a point located 4 mm nasal to the nasal border of the SR insertion. The conjunctiva was closed using interrupted sutures.
The status of reunion or reattachment of the superior oblique tendon on the globe was examined in four eyes in each group at postoperative weeks two, four, six and eight.
On examination, reopening of the sutured conjunctiva and exploration of the SO was done. Careful dissection around the SR muscle and exposure of the new insertion of the SO were performed. The degree of reunion or anterior displacement was recorded.
In the recession group, there was no change in position of the recessed SO tendon, and all 16 eyes were well positioned through postoperative week eight (Fig. 1).
In the tenotomy group, there was no observable distal end of the tenotomized SO tendon at postoperative week two for all four eyes. At four weeks, the proximal end of the tenotomized SO tendon was repositioned anteriorly and partially reattached to the sclera and the nasal border of the SR in three eyes. At six weeks, the previously tenotomized end of SO tendon was newly inserted into the nasal border of the SR in three eyes and reattached into the sclera posterior to the previously tenotomized area in one eye. At eight weeks, there was reattachment of the tenotomized ends of the SO tendon into the nasal border of the SR in all four eyes (Fig. 2).
In the tenectomy group, there was no observable distal end of the tenectomized SO tendon at postoperative week two for all four eyes. At four weeks, the tenectomized end of the SO tendon was loosely reattached in a fan-shape to the nasal side of the SR with connective tissue in two 2 eyes. At six weeks, there was reattachment of the tenectomized SO tendon into the nasal border of the SR in two eyes. At eight weeks, there was reattachment of the tenectomized SO tendon with connective tissue along the nasal border of the SR in three eyes (Fig. 3).
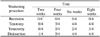
In the disinsertion group, there was no identifiable end of the disinserted SO tendon in three eyes; however, loose reattachment of the disinserted SO tendon insertion with connective tissue along with the nasal border of the SR was observed at postoperative week two in one eye. At four weeks, there was loose reattachment of the disinserted SO tendon to the SR 4 mm posterior to the nasal insertion of the SR in two eyes, loose reattachment of the disinserted SO tendon in the nasal insertion of the SR in one eye, and there was no observable end of the disinserted SO tendon in one eye. At six weeks, there was reattachment of the disinserted SO tendon into the nasal insertion of the SR in four eyes. At eight weeks, the previously disinserted SO tendons of all four eyes were reattached to the SR 2-4 mm posterior to the nasal insertion of the SR (Fig. 4)(Table 1).
Superior oblique tendon weakening procedures have been performed to treat SO overaction and Brown syndrome. In 1946, Berke19 performed SO tenotomy with variable results and several postoperative complications. Probably, this was due to blind hooking of the SO muscle through a superonasal, conjunctival incision. In 1970, Parks and Helveston20 began to perform SO weakening procedures under direct visualization of the SO insertion, and SO tendon recession was first introduced by Ciancia and Diaz.21 In 1974, Prieto-Diaz22 presented a modification of SO recession, which consisted of reinsertion of the tendon behind the equator of the globe in order to avoid frequent complications like a limitation of depression in abduction and an over-convergence in extreme downgazing.
Surgeries for SO overaction are relatively less common than are those for esotropia or exotropia. Superior oblique tendon weakening procedures are technically difficult due to the location of the superior oblique insertion quite posterior to the globe. Excessive tissue damage could occur in the attempt to expose and allow direct visualization of the SO, which frequently leads to postoperative adhesions, lid edema, temporary ptosis and severe hemorrhage.4,10,12,14 To prevent these possible complications, it is necessary to avoid blindly hooking the SO muscle and taking extreme caution in handling ocular tissue during direct visualization of the SO insertion.
At present, tenotomy, tenectomy and recession of the SO muscle are the most common procedures for diminishing the action of the SO muscle. Efforts to improve SO weakening surgery have led to the development of such procedures as Z-lengthening, split tendon lengthening, and disinsertion.1-7 However, these methods are not often used because their surgical results are no better than those of tenotomy or tenectomy.8,10-14,23
One major drawback of SO tenotomy and tenectomy is that they are "all or none" procedures.7 If a large separation occurs in the cut ends of the tendon, it can lead to SO paresis with incyclotorsion and hypotropia.11-13 It is reported that overcorrection of the SO tendon by tenotomy or tenectomy is up to 30-85%.24 There is also undercorrection of these procedures due to incomplete separation of the SO tendon during surgery or reunion of the cut ends of the tendon after surgery.3,6-9,23,25 In patients with bifoveal fusion, intractable cyclovertical diplopia can occur, and the treatment of this diplopia is very complicated.6-10,23,26
The reason for these complications may be that there is a lack of control over the amount of separation of the cut ends of the tendon according to the degree of SO overaction.7 In 1991, Wright16 introduced a new technique for SO weakening by elongating the tendon with a segment of a 240 retinal silicone band. He reported that the use of a silicone expander demonstrated better results due to the controlled elongation of SO tendon.
Recession of SO muscle is a theoretically superior procedure to tenotomy or tenectomy for its ability to adjust the amount of SO tendon weakening.5,11-13,27,28 Buckley and Flynn7 reported that there were similar surgical results and postoperative complications between SO recession and tenotomy. Similarly, Wertz et al29 reported that disinsertion or myectomy of the inferior oblique (IO) muscle in Rhesus monkeys demonstrated only half of the shortening effect shown by the recession of the IO muscle. In these experiments, the authors inferred that recession of the IO muscle was a better operation, as disinsertion and myectomy demonstrated a more uneven and wider variation in the new insertion site of the IO muscle. We cannot directly compare their report with our experiment because of the use of different animal models and muscles; however, SO and IO muscles are both oblique muscles which share similar anatomical and functional characteristics.
The purpose of this experiment was to compare the degree of reunion of SO tendons having experienced various weakening procedures. In the recession group, there was no reunion or anterior displacement of the new insertion site because of a scleral suture placed into the SO tendon. In the other three groups, there was anterior displacement of the new insertion or reunion to the nasal border of the SR muscle. The degree of reunion was most severe in the tenotomy and disinsertion groups and less severe in the tenectomy group. Therefore, recession of the SO muscle is thought to be a theoretically superior procedure to tenotomy, tenectomy or disinsertion.
Proper surgical technique is critical to the success of any SO weakening procedure. Good results are dependent on careful dissection with preservation of the nasal intermuscular septum, and tenotomy of the entire tendon. Verification of complete tenotomy should be done by performing an exaggerated forced duction test.30
In conclusion, there are still questions as to whether this result, obtained in rabbits, is directly applicable to humans, as rabbits have less ocular movement than humans. However, we recommend SO recession over the other SO weakening procedures due to its more predictable surgical results and lower degree of reunion.
Figures and Tables
Fig. 1
In the recession group, there was no change in the recessed SO tendon position in all 16 eyes through postoperative week eight.

Fig. 2
In the tenotomy group, there were no visible cut ends of the SO tendons at postoperative week two in all four eyes (left upper). At four weeks, the proximal end of the SO tendon was repositioned anteriorly and partially reattached to the sclera in three eyes (right upper). At six weeks, there was reattachment of the proximal end of the SO tendon into the nasal border of the SR in four eyes (left lower). At eight weeks, there was reattachment of the proximal end of the SO tendon into the nasal border of the SR in all four eyes (right lower).

Fig. 3
In the tenectomy group, there were no visible cut ends of the SO tendons at postoperative week two in all four eyes (left upper). At four weeks, the proximal end of the SO tendon was loosely reattached in a fan-shape to the nasal border of the SR in two eyes (right upper). At six weeks, there was reattachment of the SO tendon into the nasal border of the SR in two eyes (left lower). At eight weeks, there was reattachment of the SO tendon along the nasal border of the SR in three eyes (right lower).

Fig. 4
In the disinsertion group, there was loose reattachment of the disinserted SO tendon along the nasal border of the SR at postoperative week two in one eye (left upper). At four weeks, there was loose reattachment of the disinserted SO tendon 4 mm posterior to the nasal insertion of the SR in three eyes (right upper). A six weeks, there was reattachment of the disinserted SO tendon into the nasal insertion of the SR in four eyes (left lower). At eight weeks, the disinserted SO tendons were reattached to the SR 2-4 mm posterior to the nasal insertion of the SR in all four eyes (right lower).

References
1. Von Noorden GK, Campos EC. Binocular vision and ocular motility. 2002. 6th ed. St. Louis: Mosby;396–457.
2. Parks MM. Ocular motility and strabismus. 1975. Hargestown: Harpers & Row;100–108.
3. Wright KW, Spiegel PH. Pediatric Ophthalmology and strabismus. 2002. 2nd ed. New York: Springer;204–223.
4. Rosenbaum AL, Santiago AP. Clinical strabismus management: Principles and surgical technique. 1999. Philadelphia: W.B. Saunders;459–475.
5. Parks MM. Surgery for Brown syndrome. Symposium on Strabismus: Transection of the New Orleans Academy of Ophthalmology. 1978. St Louis: CV Mosby;157–177.
6. Prieto-Diaz J. Superior oblique overaction. Int Ophthalmol Clin. 1989. 29:43–50.
7. Buckley EG, Flynn JT. Superior oblique recession versus tenotomy: a comparison of surgical results. J Pediatr Ophthalmol Strabismus. 1983. 20:112–117.
8. Crawford JS. Surgical treatment of true Brown syndrome. Am J Ophthalmol. 1976. 81:289–295.
9. Parks MM. Management of overacting superior oblique Clinical course of accommodative esotropia. Optom Vis Sci. 1998. 75:97–102.
10. Scott WE, Jampolsky AJ, Redmond MR. Superior oblique teno tomy: Indications and complications. Int Ophthalmol Clin. 1976. 16:151–159.
11. McNeer KW. Untoward effects of superior oblique tenotomy. Ann Ophthalmol. 1972. 4:747–755.
12. Urist MJ. Complications following bilateral superior oblique weakening surgical procedures for A-pattern horizontal deviation. Am J Ophthalmol. 1970. 70:583–587.
13. Rubin SE, Nelson LB, Harley RD. A complication in weakening the superior oblique muscle in A-pattern exotropia. Ophthalmic Surg. 1984. 15:134–135.
14. Souza-Diaz C, Uesugui CF. Efficacy of different techniques of superior oblique weakening in the correction of the A anisotropia. J Pediatr Ophthalmol Strabismus. 1986. 23:82–86.
15. Romano P, Roholt P. Measured graduated recession of the superior oblique muscle. J Pediatr Ophthalmol Strabismus. 1983. 20:134–140.
16. Wright KW. Superior oblique silicone expander for Brown syndrome and superior oblique overaction. J Pediatr Ophthalmol Strabismus. 1991. 28:102–107.
17. Wright KW, Min BM, Park C. Comparison of superior oblique tendon expander to superior oblique tenotomy for the management of superior oblique overaction and Brown syndrome. J Pediatr Ophthalmol Strabismus. 1992. 29:92–97.
18. Yim HB, Park C. Effects of the superior oblique tendon silicone expander for superior oblique overaction. J Korean Ophthalmol Soc. 1992. 33:970–976.
19. Berke RN. Tenotomy of the superior oblique for hypertropia. Trans am Ophthalmol Soc. 1946. 44:304–338.
20. Parks MM, Helveston EM. Direct visualization of the superior oblique tendon. Arch Ophthalmol. 1970. 84:491–494.
21. Ciancia AO, Prieto-Diaz J. Retroceso del Oblicuo superior. Arch Ofthalmol B Aires. 1970. 45:193.
22. Prieto-Diaz J. Resultados y complicaciones del retroceso del oblicuo superior. Actas dell IV Congresso del CLADE. 1974. Mexico: 186.
23. Parks MM. Commentary on superior oblique tenotomy for A-pattern strabismus in patients with fusion. Binocular Viaion. 1988. 3:39.
24. Von Noorden GK, Olivier P. Superior oblique tenectomy in Brown syndrome. Ophthalmology. 1982. 89:303–309.
25. Rosenbaum AL, Santiago AP. Clinical strabismus management: Principles and surgical technique. 1999. Philadelphia: W.B. Saunders;219–229.
26. Reynolds JD, Wackerhagen M. Bilateral superior oblique tenotomy for A-pattern strabismus in patients with fusion. Binocular Vision. 1988. 3:33–38.
27. Romano P, Roholt P. Measured graduated recession of the superior oblique muscle. J Pediatr Ophthalmol Strabismus. 1983. 20:134–140.
28. Caldeira JAF. Graduated recession of the superior oblique muscle. Br J Ophthalmol. 1975. 59:553–559.
29. Wertz RD, Romano PE, Wright P. Inferior oblique myectomy, disinsertion and recession in Rhesus monkeys. Arch Ophthalmol. 1977. 95:857–860.
30. Guyton DL. Exaggerated traction test for the oblique muscles. Ophthalmology. 1981. 88:1035–1040.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download