This article has been
cited by other articles in ScienceCentral.
Abstract
Purpose
To compare high-sensitivity C-reactive protein (hsCRP) levels and lipid profiles between Korean normal tension glaucoma (NTG) patients and healthy controls.
Methods
This cross-sectional study included 38 Korean patients with NTG and 38 age- and sex-matched healthy control subjects. We excluded the patients with cardiovascular risk factors and other systemic diseases that might affect CRP levels and lipid profiles. Each patient underwent a Humphrey visual field examination and blood sampling for hsCRP and lipid profile analyses. Subsequently, the NTG patients were classified into two groups based on their untreated intraocular pressure (IOP) level: low NTG (LNTG) with IOP≤13 mmHg (13 subjects) and high NTG (HNTG) with relatively high IOP (>13 and ≤21 mmHg, 25 subjects). The hsCRP levels and lipid profiles were compared between NTG patients and healthy controls, and between LNTG, HNTG, and healthy controls.
Results
There were no significant differences in hsCRP and lipid profiles between either the NTG patients and healthy controls, or between the LNTG, HNTG, and controls (p>0.05) after exclusion of Korean patients with cardiovascular risk factors. There was no significant association between hsCRP and visual field indices (p>0.05).
Conclusions
High-sensitivity C-reactive protein-related vascular inflammatory conditions may not be directly associated with the development of NTG, regardless of the untreated IOP level.
Keywords: Atherosclerosis, C-reactive protein, Lipid profiles, Normal tension glaucoma
Normal tension glaucoma (NTG) is a clinical disease entity characterized by progressive thinning of the retinal nerve fiber layer and corresponding visual field loss in eyes with a normal range of intraocular pressure (IOP). Hypotheses associated with the development of NTG include vascular dysregulatory factors, such as systemic blood pressure changes, ocular blood flow abnormalities, or vasospasm.
1-
3 Many patients with glaucoma have an increased endothelin-1 plasma level.
4 In patients with primary open angle glaucoma (POAG), both systemic arteriosclerosis and sclerotic changes in the ocular vessels have been observed but also questioned.
5,
6 Theoretically, these sclerotic changes in ocular vasculature might result in the impairment of ocular perfusion, with thickening of the vascular endothelial wall.
C-reactive protein (CRP) is an early acute phase reactant of inflammation, increasing in response to active infections or acute inflammatory processes. Minor elevations of CRP are also present in chronic inflammatory situations, such as atherosclerosis.
7 High-sensitivity CRP (hsCRP) is the most reliable and accessible marker of inflammation associated with atherosclerosis.
8 It was also found to be correlated with impaired systemic endothelial vascular reactivity, and it was suggested that it may have a role in the pathogenesis of endothelial dysfunction and atherogenesis.
9,
10 Risk factors for atherosclerosis are also important fields of interest. Any cardiovascular risk factor which can damage the vascular endothelial wall could increase the incidence of atherosclerotic change in the vessels. Dyslipidemia is one of the most important risk factors for the development of atherosclerosis.
The vascular dysfunction observed in patients with NTG may be a consequence of systemic vascular endotheliopathy.
11 A population-based epidemiological survey in Japan revealed that 92% of POAG patients had a normal IOP range.
12 The prevalence of NTG in the Japanese population is higher than that of Western countries.
13,
14 Because of this, it could be speculated that there might be a different underlying mechanism of pathogenesis for NTG in Asians.
The roles of atherosclerosis and dyslipidemia in the development of NTG have not yet been well defined. Leibovitch et al. found that plasma hsCRP levels were significantly higher in the NTG cases than in the controls.
15 However, Su et al. found no significant differences in hsCRP levels and lipid profiles in NTG patients when compared with age- and sex-matched controls.
16,
17
We compared hsCRP and lipid profiles between patients with NTG and healthy controls in a homogenous Korean population, in which NTG is presumably the most common type of open-angle glaucoma. We also investigated whether or not there was any difference in hsCRP and lipid profiles between NTG patients with high levels of IOP and those with low IOP levels at the initial diagnosis of glaucoma.
Materials and Methods
We performed an age- and sex-matched case-control study with 38 newly diagnosed NTG patients and 38 healthy control subjects. All subjects were Korean. Each subject underwent a complete slit-lamp examination, including gonioscopy, IOP evaluation by Goldmann applanation tonometry, Humphrey visual field 24-2 full threshold or SITA standard examination (Humphrey Visual Field Analyzer II Model 745i, Carl Zeiss Meditec, Dublin, CA), and fasting blood sampling for hsCRP and lipid profiles including total cholesterol, low density lipoprotein (LDL) cholesterol, high density lipoprotein (HDL) cholesterol, and triglycerides.
Normal tension glaucoma eyes (n=38) were defined as having: (1) an untreated IOP not exceeding 22 mmHg at different times of the day, from 9 AM to 5 PM (2) open anterior chamber angles on gonioscopy (3) glaucomatous optic neuropathy with thinning or notching of the neuroretinal rim and (4) reliable glaucomatous visual field defects with Glaucoma Hemifield Test results (GHT) outside of 99% of the age-specific normal limits or a PSD outside of 95% of the normal limits.
Thirty-eight healthy volunteers were recruited from within the medical staff or clinic patients who had previously undergone cataract surgery. All subjects had a best-corrected visual acuity of 20/30 or better. The normal appearances of the optic nerve heads in both eyes were confirmed by a complete ophthalmic examination. The control eyes had intact neuroretinal rims; there was no evidence of disc hemorrhage, notching, excavation, or asymmetry of the vertical cup to disc ratio >0.2. No other pathologic ocular condition other than cataract was noted. No subject in the control group had a history of IOP elevation above 21 mmHg or ocular trauma. The visual fields of the control subjects were all normal. The GHT result was within normal limits, and the field did not meet any of the following criteria described above.
Subjects with systemic diseases that might be associated with an increased level of CRP (hypertension, hypercholesterolemia, diabetes mellitus, cerebral vascular accident, infection, chronic pulmonary obstructive disease or autoimmune diseases) were excluded from the study, thus none of our subjects were taking systemic medication that might affect CRP level, such as anti-hypertensives, cholesterol-lowering agents, or aspirin.
Normal subjects were selected to match NTG patients by age and sex. For both NTG and control subjects, if both eyes met the inclusion criteria for the study, one eye was selected at random. The affected eye was selected in unilaterally diseased NTG patients. NTG patients were initially classified into two groups based on their untreated IOP levels: one with low IOP (≤13 mmHg low normal tension glaucoma, LNTG n=13), and the other with relatively high IOP (>13 and ≤ 21 mmHg high normal tension glaucoma, HNTG n=25). Data are expressed as the mean±standard deviation. Continuous variables were compared between the NTG and control groups using the unpaired Student's t-test and were compared among the LNTG, HNTG, and controls with the Kruskal-Wallis test. Categorical variables between groups were compared with the Chi-square test. Differences with a value of p<0.05 were considered statistically significant. Subsequently, NTG patients were classified based on the IOP cutoff point of 16 mmHg for the comparison of hsCRP and lipid profiles (IOP ≤16 mmHg, n=23 >16 and ≤21 mmHg, n=15). All applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during this study.
Results
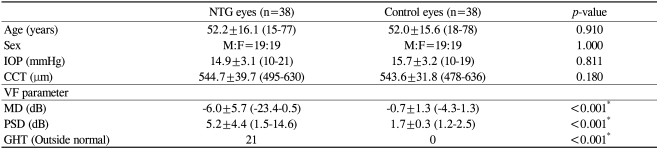
Table 1 presents descriptive statistics for the demographic and clinical characteristics of the study patients. All 38 NTG patients were Korean 19 (50.0%) were men and 19 (50.0%) were women. There were no significant differences in age, IOP, and central corneal thickness (CCT) between overall NTG subjects and normal controls (age,
p=0.910 IOP,
p=0.811; CCT,
p=0.180). Visual field parameters (mean deviation (MD), pattern standard deviation (PSD)) were worse in patients with NTG (MD,
p<0.001; PSD,
p<0.001) than in control patients.
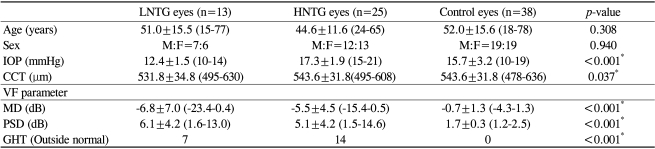
Table 2 presents descriptive statistics for the demographic and clinical characteristics of the LNTG, HNTG, and control patients. Seven (53.8%) LNTG patients were men and six (46.2%) were women, while 12 (48.0%) HNTG patients were men and 13 (52.0%) were women. There was no significant difference in age among the groups (
p=0.940) however, IOP, CCT, MD, and PSD were different among the groups (IOP,
p<0.001; CCT,
p=0.037; MD,
p<0.001; PSD,
p<0.001).
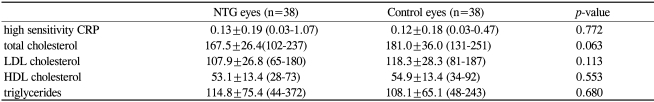
Table 3 shows descriptive statistics and comparisons of hsCRP and lipid profiles between NTG patients and control subjects. None of these biochemical parameters showed statistical significance between the NTG patients and the normal control subjects (hsCRP,
p=0.772; total cholesterol,
p=0.063; LDL cholesterol,
p=0.113; HDL cholesterol,
p=0.553; triglycerides,
p=0.680).
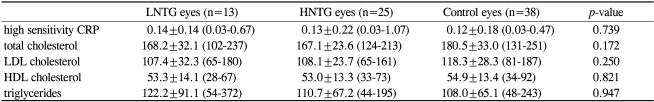
Table 4 shows descriptive statistics and comparisons of hsCRP and lipid profiles between the LNTG, HNTG, and the normal controls. There were no statistical significances in the differences in the parameters among the groups (hsCRP,
p=0.739; total cholesterol,
p=0.172; LDL cholesterol,
p=0.250; HDL cholesterol,
p=0.821; triglycerides,
p=0.947). When the data was analyzed with an IOP cutoff point of 16 mmHg, there also was no statistical significance in hsCRP and lipid profiles between LNTG and HNTG subjects (hsCRP,
p=0.131; total cholesterol,
p=0.143; LDL cholesterol,
p=0.191; HDL cholesterol,
p=0.606, triglycerides,
p=0.180).
Discussion
Our data showed that CRP level and lipid profiles were not different between NTG patients and normal controls. These results coincide with those of the article published by Su et al.
16,
17 However, our data is contrary to the prior report by Leibovitch et al.
15 which showed an increased level of hsCRP in NTG patients when compared with normal controls. In their study, they did not exclude patients with hypertension, DM, and other systemic diseases that can affect CRP level. As CRP and lipid profiles differ with age and race,
18 an age- and sex-matched case-control study in a homogenous population is most desirable for the comparison of the biochemical parameters. In our study of Korean patients, the subjects with systemic diseases such as hypertension, hypercholesterolemia, ischemic heart disease, and cerebrovascular incidents were all excluded. In our study design, we thought a higher accuracy would be achieved if we determined the association between NTG and CRP level after excluding those patients with systemic diseases to minimize the biasing effect of systemic morbidity.
In contrast, other studies might produce different results if the systemic morbidity of subjects is not taken into account. There is evidence suggesting that atherosclerosis affects the peripheral circulation of the blood flow in the end-organs, resulting in diseases such as ischemic heart disease and ischemic brain disease.
19,
20 There is also evidence which suggests that the development of NTG is affected by reduced or unstable ocular blood flow,
2 and that atherosclerosis is the most typical cause of compromised blood flow due to the resulting vascular stiffness with vascular endothelial wall thickening. This suggests that the lack of association between CRP and lipid profiles with NTG in our series of patients does not rule out the possibility of an association of atherosclerosis with NTG. A prospective, population-based study will be needed to answer this question.
The definition of "normal tension" in NTG was derived from an old epidemiological survey by Leydhecker et al. on the IOP distribution in patients with no visual field defects.
21 Lee et al. showed that, in NTG patients with low IOP ≤13 mmHg, IOP-related parameters were not associated with functional and structural glaucomatous damages, while there was an association in NTG patients with relatively high IOP >13 mmHg, suggesting that there might be different subgroups within NTG patients based on the untreated IOP levels [Lee CH, Lee J, Choi J, Kook MS. Prediction of glaucomatous damage using central corneal thickness and 24-hour IOP profiles. AAO annual meeting 2006 poster abstract]. In our study, there was no difference in CRP and lipid profiles when NTG subjects were classified by their untreated IOP levels, indicating that a direct linkage between the vascular inflammation associated with atherosclerosis and glaucoma is lacking in NTG eyes with differing IOP levels.
Iwase et al. reported the higher prevalence of NTG among Japanese subjects in an epidemiological study.
12 The prevalence of cases of POAG with IOP levels of 21 mmHg or less was 3.6%, whereas the prevalence for those with IOP levels of more than 21 mmHg was 0.3% in their study. The associations of the polymorphism of the endothelin receptor type A gene with NTG were reported only in Korean and Japanese populations.
22,
23 These findings, differing from Western studies, raised the need for an investigation of vascular risk factors other than IOP in Asian populations. For example, a recent report suggested that circadian fluctuations in mean ocular perfusion pressure were associated with functional and glaucomatous damages in Korean NTG subjects.
2 We hypothesized that systemic atherosclerosis could jeopardize the local perfusion status of the ocular vessels. C-reactive protein levels and lipid profiles in this study functioned as a proxy for general atherosclerosis in the vessels. We found that these biochemical parameters did not differ between NTG patients and the normal controls, nor did they differ between the NTG patients grouped according to their different IOP levels. Direct evidence that systemic endothelial dysfunction was associated with NTG was not obtained.
Our study has limitations due to the small groups sizes of NTG subjects and normal controls. Determining sample size is an important issue in a clinical study because samples that are too large may waste time, resources, and money, while samples that are too small may lead to inaccurate or non-applicable results. We did not calculate the sample size statistically in the present study as it was very difficult to assume the effect size of NTG on hsCRP and lipid profiles as there are a very limited number of articles, which themselves are very controversial.
15-
17 Thus, our study should be regarded only as a pilot study. Exclusion of the NTG subjects with systemic morbidity in our study could result in another type of selection bias, as it is known that there are heterogenous risk factors contributing to the development of NTG. C-reactive protein levels may also vary in patients in different stages of glaucoma. Further investigations are needed to reveal the association of CRP and lipid profiles with NTG patients according to the presence of systemic cardiovascular disease.
In conclusion, our negative findings suggest that the hsCRP-related vascular inflammatory component may not be a direct risk factor for the development of NTG in Korean subjects who do not have systemic cardiovascular disease.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download