Abstract
We report a case of ocular ischemic syndrome accompanied by neovascular glaucoma that was successfully treated with Bevacizumab. A 70-year-old male patient diagnosed with neovascular glaucoma of the left eye 3-4 years prior complained of continuous left eye pain and declining visual acuity despite receiving the latest treatment methods. At the time of admission the patient had no light perception in the left eye and his intraocular pressure was 30 mmHg. Anterior segment and fundus examinations revealed neovascularization of the iris and stenosis of the retinal vessel. Hypofluorescence of the choroid and retinal vessels was observed on fluorescence fundus angiography. Left internal carotid artery stenosis was observed on a brain MRI. Despite being treated with eye solution and oral medication, intraocular pressure was not controlled. After 7 days, we performed an intravitreal Bevacizumab 1.25 mg/0.05mL injection. One day after the intravitreal Bevacizumab injection, the neovascularization had nearly regressed and intraocular pressure was 30 mmHg. Intravitreal Bevacizumab injection produced regression of neovascularization and proved effective for treatment of neovascular glaucoma in this case of ocular ischemic syndrome.
Ocular ischemic syndrome occurs in about 5% of patients diagnosed with severe carotid artery occlusion (>90%), and may lead to neovascular glaucoma (NVG) due to the growth of blood vessels on the iris surface and anterior chamber angle. NVG develops in about 1/3 of cases of ocular ischemic syndrome. Vascular endothelial growth factor (VEGF) is the most thoroughly studied angiogenic peptide implicated in ischemic retinal disease and NVG.1 VEGF is mitogen specific for vascular endothelial cells, and recently, the intravenous use of an anti-VEGF antibody, bevacizumab (Avastin) has been applied to target vessel formation for treatment of colorectal cancer. Intravenous and intravitreal injection of bevacizumab has also been reported to have anatomical and functional success for treating choroidal neovascularization and macular edema.2 We report a successful case of intravitreal injection of bevacizumab for the treatment of iris and angle neovascularization in a patient with NVG secondary to ocular ischemic syndrome.
A 70-year-old patient with a 4-year history of neovascular glaucoma due to ischemic retinopathy in the left eye and vertigo visited our hospital after having received the maximal medical therapy for intraocular pressure (IOP) control and panretinal photocoagulation (PRP) at another facility. He had experienced a total lack of light perception in the left eye for 3 years and his IOP was 30 mmHg. Slit lamp examination demonstrated 6 clock hours of angle neovascularization with synechiae in left eye (Fig. 1). Indirect ophthalmoscopy revealed narrowing and ghost retinal vessels and a pale optic disc. Fluorescein angiography revealed hypofluoresceins in the choroid and retinal vessels (Fig. 2A). Magnetic resonance angiography indicated significant occlusion of the left carotid artery (Fig. 2B). We diagnosed the patient with ocular ischemic syndrome and treated him with the maximal tolerable medical therapy (timolol and brimonidine, oral acetazolamide and intravenous mannitol) for 7 days, but his IOP remained high (27-38 mmHg). The use of bevacizumab was discussed as an alternative after fully explaining its experimental status for ocular neovascular disease. The patient opted for intravitreal bevacizumab (Avastin) injection and signed a consent form out-lining the risk factors, possible side effects, and experimental status of the medication. We injected 1.25 mg/0.05mL of bevacizumab into the vitreous cavity of the patient's left eye. One day after intravitreous injection of bevacizumab, the neovascularization of the iris had almost completely resolved (Fig. 3), but the anterior synechiae remained. In addition, IOP was 33 mmHg and his visual acuity was unchanged. After 2 days, the patient underwent left carotid artery stent insertion for severe left carotid artery stenosis. He experienced onset of severe ocular pain and his IOP was 53 mmHg. He was treated with intravenous mannitol and oral acetazolamide, which resolved the ocular pain and reduced the patient's IOP to 22 mmHg. After 7 days of injection, we started treatment with PRP on the left eye. His IOP was unchanged and the regression of neovascularization of the iris persisted. At 10 days, the regression of neovascularization was still present and the IOP was unchanged at 33 mmHg. Since there was no longer any ocular pain and light perception had returned, no additional surgery was planned. After 8 months, the ocular pain had not returned.
Ocular ischemic syndrome occurs secondary to severe carotid artery obstruction and involves ocular signs and symptoms including corneal edema, rubeosis iridis, neovascular glaucoma, hypoperfusion retinopathy, and choroidal perfusion disturbance. Neovascular glaucoma is a devastating complication caused by ischemic retinopathy secondary to carotid artery occlusion. VEGF plays a central role in ocular pathologies characterized by neovascularization and increased vascular permeabillty.3 The standard treatment includes retinal photocoagulation and cyclodestructive or drainage procedures. In this case, panretinal photocoagulation (PRP) was completed to decrease the constant rate of VEGF secretion and stop the neovascular drive. However, in spite of PRP, the IOP remained high.
Bevacizumab is a recombination of humanized anti-VEGF IgG1 approved as an antiangiogenic agent for the treatment of metastatic colorectal cancer in combination with chemotherapy.4 It has the effect of reversing neovascularization by controlling VEGF. A recent studiy proposed using bevacizumab intravitreally for age-related macular degeneration.5 In the present case, 24 hours after treatment we saw a dramatic reduction of iris neovascularization, and no relapse was seen within a follow-up time of 10 days. IOP was still high (22-33 mmHg), however, probably due to chronic NVG with synechiae. Other case reports suggest that a single injection of bevacizumab was associated with medically controlled for at least 6 weeks.6 However, treatment with bevacizumab seems to have a fast, potent effect on neovascular pathologic correlates. In conclusion, bevacizumab may be a valuable adjunct in treating neovascular glaucoma, though further studies are needed to outline optimal time, doses, and patient selection.
Figures and Tables
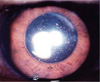
Fig. 1
Slit lamp examination demonstrated 6 clock hours of angle neovascularization with synechiae in the left eye.
References
1. Michels S, Rosenfeld PJ, Puliafito CA, et al. Systemic bevacizumab (Avastin) therapy for neovascular age-related macular degeneration: twelve-week result of an uncontrolled open-label clinical study. Ophthalmology. 2005. 112:1035–1047.
2. Reichel E. Intravitreal bevacizumab for choroidal neovascularization and cystoid macular edema: a cost-effective treatment. Ophthalmic Surg Laser Imaging. 2005. 36:270–271.
3. Ferrata N. Vascular endothelial growth factor: basic science and clinical progress. Endocr Rev. 2004. 25:581–611.
4. Howitz H, Fehrenbacher L, Novotny W, et al. Bevacizumab plus irnotecan, fluorouracil, and leucovorin for metastatic colorectal cancer. N Engl J Med. 2004. 350:2335–2342.
5. Rosenfeld PJ, Mosfeghi AA, Puliafito CA. Optical coherence tomography finding after an intravitreal injection of bevacizumab (Avastin) for neovascular age-related macular degeneration. Ophthalmic Surg Laser Imaging. 2005. 36:331–335.
6. Kahook MY, Schuman JS, Noecker RJ. intravitreal bevacizumab in a patient with neovascular glaucoma. Ophthalmic Surg Laser Imaging. 2006. 37:144–146.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download