Abstract
A 48-year-old man presented with visual dimness in the right eye that had developed 2 weeks previously. Dilated fundus examination showed few vitreous cells and numerous yellow, placoid lesions in both eyes. His right eye had more severe serous retinal detachment involving the macula. Fluorescein angiography demonstrated early irregular hypofluorescence with late staining in the areas of the yellow placoid lesions. He started a regimen of 60 mg of oral prednisone daily. Two weeks later, a serologic fluorescent treponemal antigen absorption test was positive for Ig G and Ig M. He was referred to an infectious disease specialist for antibiotic therapy. A week later, he returned, having stayed on prednisone only and not having taken the internist's antibiotic prescription. Meanwhile, the chorioretinitis in his right eye, which had initially been at a more advanced stage, was resolved with the use of steroids. The chorioretinitis in his left eye, which was aggravated at an earlier stage, ultimately recovered. Our case had atypical courses such that one eye improved and the other worsened during the same steroid treatment period. This result was inconsistent with that of previous reports showing that oral steroid influences the clinical course of acute syphilitic posterior placoid chorioretinitis.
Acute syphilitic posterior placoid chorioretinitis (ASPPC) is a variation of posterior segment involvement caused by syphilis.1 Penicillin is the mainstay of treatment for ocular syphilis. However, because it is not always easy to diagnose ocular syphilis at the early stage of chorioretinitis, systemic steroids are sometimes prescribed before a serologic report is obtained. Corticosteroids are potentially harmful to patients with infectious uveitis. Some researchers have suggested that the clinical appearance of posterior placoid chorioretinitis in a patient with syphilis may be modulated by the immune status of the patient.2 We describe the atypical clinical course of a patient with bilateral ASPPC at different stages who incidentally had taken oral steroids without proper antibiotics.
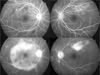
A 48-year-old man presented with visual dimness in his right eye, which had developed over the two weeks prior to the visit to the ophthalmology clinic. His medical, family, and social history was unremarkable. His visual acuity (VA) was 20/50 in the right eye (OD) and 20/20 in the left eye (OS). The anterior segments were clear on slit-lamp biomicroscopy. The pupils were reactive in each eye without notable irregularity or afferent pupillary defects. Dilated fundus examination showed few vitreous cells and numerous yellow, placoid lesions in both eyes (OU) (Fig. 1 A and B). Only the OD had more severe serous retinal detachment involving the macula. Fluorescein angiography demonstrated early irregular hypofluorescence with late staining in the areas of the yellow placoid lesions (Fig. 2). Serologic tests were ordered, and the patient was monitored without medication.
The patient returned 7 days later with worsening vision in his left eye. His right VA was unchanged. Serous retinal detachment of the macula decreased in OD. In OS, VA decreased to 20/30 and yellow, placoid lesions increased to involve the macula. He was started on a regimen of 60 mg (1.2 mg/ kg of his body weight) of prednisone daily.
One week after prednisone treatment, his right VA increased to 20/30 and the retinal lesions improved. However, the left VA deteriorated to 20/40, and the placoid lesions were aggravated. We discovered that the patient did not follow our recommendation for serologic work-up. The serologic tests were ordered again, and his blood sample was sent for laboratory work-up. Prednisone was tapered down to 50 mg daily, and he returned 1 week later with improved VA of 20/20 and completely resolved chorioretinal lesions in the OD. However, his left VA decreased to 20/70 and macular edema increased (Fig. 1 C and D). Serologic testing was positive for Venereal Disease Research Laboratory antigen and negative for HIV titers. He had no other syphilitic manifestations. In order to avoid a possible rebound reaction to prednisone withdrawal, prednisone was rapidly tapered to 30 mg daily, and the patient was referred to an infectious disease specialist for antibiotic therapy. He returned 1 week later with improved VA of 20/20 in the OD and 20/30 in the OS. Fundoscopy showed resolution of the chorioretinal lesions in the OS. A serologic fluorescent treponemal antigen absorption test was positive for Ig G and Ig M. However, the patient was not taking any antibiotics yet, because he refused to follow the internist's recommendation of admission to the hospital and commencement of an antibiotic prescription. He had received only 30 mg of prednisone without antibiotic coverage. Prednisone was tapered to 10 mg, and he was sent for medical consultation again. One week later, he returned and still had not begun antibiotics. His vision was 20/20 in OU and he had no visual complaint. The previous lesions disappeared completely. However, new multiple focal chorioretinal lesions were noted outside the inferior retinal vascular arcades of the OS. Prednisone was discontinued, and he was referred again to the Infectious Disease Department. After medical examination, including a cerebrospinal fluid (CSF) study, he was started on ceftriaxone, 2.0 g intravenously for 14 days, and returned with resolution of the focal chorioretinitis. The CSF study result was negative. There was no recurrence in OU for the next five months.
The most common posterior segment involvement of ocular syphilis is chorioretinitis.3 To denote a variation of posterior segment involvement, Gass1 coined the term "Syphilitic Posterior Placoid Chorioretinitis". The findings show large, placoid, yellowish lesions with faded centers at the level of the retinal pigment epithelium in the macular and juxtapapillary areas, which show similar angiographic patterns, specifically early hypofluorescence and late staining. It has been supposed that this particular finding might be a direct result of the modification of the host immune response to syphilis by the HIV virus. Tran et al.4 suggested that syphilitic uveitis in HIV-infected patients seems to have a more severe course. Erol and Topbas5 described a case of ASPPC after an intraviteal triamcinolone acetonide injection. Moreover, Zamani and Garfinkel2 reported the relationship between oral prednisone and the appearance of ASPPC. In their case, ASPPC developed after treatment with oral prednisone and resolved when the corticosteroid was discontinued. They suggested that its clinical appearance might be modulated by the immune status of the patient and that if corticosteroids are given without systemic treatment for syphilitic manifestations at the same time or shortly thereafter, the number of treponemes may increase and new lesions may appear. However, the results from our case do not support their suggestions. In our case, the patient took only oral prednisone without simultaneous coverage by the proper antibiotics, because he refused to follow the internist's recommendation. At initial presentation, the chorioretinitis in his right eye was at a more advanced stage. His right eye had improved during the prednisone therapy, while the left eye was aggravated. This implies that his chorioretinitis had a clinical course unresponsive to the use of prednisone. Instead, its clinical course was more like that of APMPPE. Chorioretinitis recurred after tapering the dosage of prednisone but was resolved after treatment with antibiotics. It is not clear whether prednisone influenced the course of chorioretinitis. However, chorioretinitis at different stages had the same clinical course (onset-aggravation-resolution), regardless of treatment with prednisone. It suggests that ASPPC has its own clinical course and is not influenced by systemic steroid use. Another possibility is that the anti-inflammatory effect of prednisone had appeared late in treatment because the chorioretinitis of both eyes resolved at the end of the prednisone treatment. However, the latter is less likely because one eye improved and the other was aggravated during the same treatment period. Our case had an atypical course for this disease, and it was not consistent with the hypothesis that a particular fundus finding of ASPPC may be the direct result of a patient's altered immune response to syphilis, especially induced by corticosteroid therapy started before the initiation of antimicrobial therapy.
Figures and Tables
Fig. 1
(A, B) At initial presentation, numerous yellow, placoid lesions were noted in both eyes. Serous retinal detachment involving only the macula in the patient's right eye was observed. (C, D) Two weeks after treatment with prednisone, lesions of the right eye completely resolved. However, macular edema in the left eye increased.

References
1. Gass JD, Branunstein RA, Chenoweth RG. Acute syphilitic posterior placoid chorioretinitis. Ophthalmology. 1990. 97:1288–1297.
2. Zamani M, Garfinkel RA. Corticosteroid-induced modulation of acute syphilitic posterior placoid chorioretinitis. Am J Ophthalmol. 2003. 135:891–894.
3. Samson CM, Foster CS. Foster CS, Vitale AT, editors. Syphilis. Diagnosis and Treatment of Uveitis. 2001. Philadelphia: WB Saunders;237–243. chap.15.
4. Tran TH, Cassoux N, Bodaghi B, et al. Syphilitic uveitis in patients infected with human immunodeficiency virus. Graefes Arch Clin Exp Ophthalmol. 2005. 243:863–869.
5. Erol N, Topbas S. Acute syphilitic posterior placoid chorioretinitis after an intravitreal triamcinolone acetonide injection. Acta Ophthalmol Scand. 2006. 84:435.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download