Abstract
Purpose
To compare the predicted and actual refractive errors of hydrophilic, one-piece, C-flex®570C (C-flex) intraocular lens (IOL) implantation in simultaneous vitrectomy and lens extraction in various conditions.
Methods
One hundred fifty-nine eyes of patients who had lens extraction between March 2004 and September 2005 were enrolled in a retrospective study. Group 1 had lens extraction and IOL implantation, and Group 2 had lens extraction and IOL implantation with vitrectomy. IOL calculation was done with axial length and keratometry measurements. The actual and predicted refractive errors were compared at 1 and 6 months postoperatively. The factors influencing the postoperative refractive outcomes were analyzed.
Results
The mean refractive predictive error (i.e., the actual minus predicted spherical equivalent) was +0.19±0.39 D (Diopter) and -0.26±0.45 D at 1 and 6 months postoperatively (all: p<0.001) in group 1, and -0.22±0.39 D and -0.06±0.62 D at 1 and 6 months postoperatively (p=0.013, p=0.399 respectively). In group 2, all surgical factors related to refractive errors were not statistically significant (all: p>0.05).
Conclusions
Refractive errors in combined surgery showed myopic shift of -0.50 D and -0.32 D at 1 and 6 months postoperatively compared with C-flex IOL implantation alone. With the hyperopic tendency of IOL and myopic tendency of vitrectomy, the combined surgery made postoperative refractive errors near emmetropia.
As vitreoretinal disorders and cataracts frequently appear simultaneously in elders, the incidence of a combined surgery of vitrectomy, lens extraction and intraocular lens (IOL) implantation has increased. The combined surgery is more time consuming and technically difficult procedure, but reduces recovery time and costs.1 And also the results of combined surgery improved with newly developed surgical techniques and IOLs.2-5 In performing the combined surgery, achieving the best uncorrected visual acuity (BUVA) patients needed would be more important than achieving the best corrected visual acuity (BCVA), because in that way, the patients can be freed from the glasses. Thus, it is crucial to achieve the exact postoperative refractive errors, close to expected ones.
C-flex®570C (C-flex, Rayner, UK) is an one-piece, hydrophilic acrylic IOL 12.0 mm in total length and 5.75 mm of optic, equiconvex in both sides (Fig. 1).6 A combined complex of hydrophilic HEMA (hydroxyethyl methacrylate) and hydrophobic MMA (methylmethacrylate), named as Rayacryl, contains 26% of water and 1.46 of refractive power. An edge enhancement around the optic was designed to reduce posterior capsular opacity, and an opened C-loop to resist against posterior capsule contraction.7,8 With a single handled customized injector, the insertion is easy and safe.9 A specially designed haptic made it to fix easily to sclera,10 and it is frequently used in vitreoretinal surgery due to its minimal adherence to silicone oil.11
A few studies had been reported about the changes of axial length and anterior chamber depth, and the myopic shift resulting from replacement of vitreous by aqueous humor in a combined surgery of vitrectomy and cataract extraction in retinal disorders. But, no study has yet been reported about the estimation of refractive error after either C-flex IOL implantation alone or a combined surgery with vitrectomy. The purpose of this retrospective study was to evaluate the difference between predicted and actual refractive error (RE) in both C-flex IOL implantation alone and a combined surgery with vitrectomy.
We reviewed the medical records of 159 patients (159 eyes) who underwent C-Flex IOL implantation from March 2004 to September 2005 retrospectively. The patients who received phacoemulsification with 3 mm incision and had at least 6 months follow-up period were included. Group 1 (n=85 eyes) was defined as the patients with cataract extraction and IOL implantation, and group 2 (n=74 eyes) was defined as the patients with cataract extraction, IOL implantation and vitrectomy. Vitreoretinal disorders in group 2 which need vitrectomy surgery were as follows: epiretinal membrane (28 eyes, 27.8%), diabetic retinopathy (18 eyes, 24.3%), branched retinal vein occlusion (14 eyes, 18.9%), macular hole (12 eyes, 16.2%) and uveitis (2 eyes, 2.6%)(Table 1).
To minimize the bias affecting RE before and after the surgery, the patients with the axial length of <21.0 mm or ≥27.0 mm and the patients whose keratometry values were <41.0 diopter (D) or ≥47.0 D were excluded. The eyes with history of trauma, scleral encircling, or silicone oil were excluded also. The cases with posterior lens capsule rupture during the surgery were also excluded.
Before the surgery, the patients underwent preoperative evaluation by a single, well-trained examiner. Automatic keratometer (Humphrey division, Germany) was used to measure keratometric values and ultrasonic A scan biometry (Paradigm, USA) was used to measure the axial length. A SRK/II formula was used for the eyes with axial length between 21.0 mm and 25.0 mm, and a SRK/T for over 25.0 mm. The targeted RE was within -0.5 D in most cases, and in 10 eyes, various targeted RE up to -4.0 D were applied according to the RE of fellow eyes.
The surgery was performed by one author (S.J.Lee), and a sutureless 3.0 mm clear cornea incision was made at the 10 o'clock position in group 1, and a 3.0 mm scleral tunnel with 10-0 nylon suture at the 10 o'clock position in group 2. Conventional 3 port vitrectomy was performed, and the IOL was implanted in-the-bag in all of the cases.
The manifested refraction using an automatic refractometer (Humphrey division, Germany) was measured by optometrists at 1 and 6 months after the surgery. The spherical equivalent (SE) value of manifested refraction value was defined as RE, and the expected RE before the surgery and the actual RE after the surgery were compared. A paired t-test was used for the statistical comparison within the group, and the student t-test for between the groups. And with the results from group 2, the correlation of the presence of the internal limiting membrane removal, macular hole, epiretinal membrane and macular edema to the results was analyzed with paired t-test. The statistics were analyzed using SPSS (SPSS for windows version 15.0, SPSS Inc. Chicago, USA) software.
The mean age of Group 1 was 63.1±10.4 years old and Group 2 was 66.1±9.2 years old. The difference of the mean ages was not significant between the two groups (p=0.054). The mean axial lengths were 23.10±0.99 mm and 23.16±1.00 mm in groups 1 and 2 respectively, which showed no significant difference (p=0.715). The mean corneal refractive powers were 44.45±1.35 D and 44.64±1.55 D in groups 1 and 2 respectively without a statistical difference (p=0.430). (Table 2)
At 6 months postoperatively, the difference between the predicted and actual RE within 0.5 D was counted in 72 eyes (84.7%) and 57 eyes (77.0%) in groups 1 and 2. The difference within 1.0 D was 81 eyes (95.3%) and 65 eyes (87.8%) in groups 1 and 2. (Table 3)
In group 1, the mean predicted RE before the surgery was -0.28±0.20 D, and the mean actual RE at 1 month postoperatively was -0.10±0.39, showing a hyperopic difference of +0.19±0.39 D (p<0.001). The difference increased to +0.26±0.45 D at 6 months postoperatively (p<0.001). In group 2, the mean predicted RE before the surgery was -0.27±0.23 D, and the mean actual RE was -0.49±0.70 D and -0.33±0.58 D at 1 and 6 months postoperatively, which made the difference of -0.22±0.74 D and -0.06±0.62 D respectively. The actual REs at 1 and 6 months postoperatively were more myopic than expected, and a statistical significance was noted at 1 month postoperatively (p=0.013). The difference between the groups was statistically significant at both 1 and 6 months after the surgery (p<0.001). (Table 4) In summary, the mean actual REs were shifted more hyperopically than predicted at 1 and 6 months after the surgery in group 1, and in group2, the difference was more myopic at 1 month, and shifted into more hyperopic than the predicted at 6 months after the surgery, which showed no statistical significance compared with that of predicted. (Fig. 2)
The influence of vitreoretinal disorder or surgery such as gas injection, internal limiting membrane removal, macular hole, epiretinal membrane or macular edema on the difference between the expected and actual RE was evaluated in group 2, and none of factors affected on the difference significantly (p>0.05). (Table 5)
Due to improvements of cataract surgery technique and IOL, the complications related to the cataract extraction surgery had been decreased with shorter period of recovery.12-14 With precise biometric measurements and calculations, more accurate refractive error can be calculated before the surgery. These improvements opened a way to meet the variety of patients' needs, with emplasis on BUCV.
To achieve the accurate predicted RE before the surgery, the biometric measurements including the keratometric value must be accurate, IOL calculation must be well applied, and IOL's characteristics must be well acknowledged. Above all, the biometric measurements are thought to be the most important, because an error of 1 mm would result in 2.5 D difference, and error of 1 D of corneal refractive power, in 1 D difference.15-17
Holladay et al.18 defined the guideline on 'good' IOL by predicted RE within 0.5 D from predicted in 50% at least, 1.0 D in 90% at least. In our study, the difference from predicted within 0.5 D turned out to be 84.7% and 77.0% in groups 1 and 2, and within 1.0 D by 95.3% and 87.8% respectively. The C-flex IOL showed tolerable predictability in both cataract extraction surgery and a combined surgery with vitrectomy, according to previous studies.
Several studies revealed the various changes of RE affected by the materials and shape of IOL. Assia et al.19 reported a PMMA (polymethyl methacrylate) IOL being more stable in RE than polypropylene. Chang et al.20 reported the hyperopic shift by using SI20NB (AMO, USA) with polypropylene haptics, and Kim et al.21 reported the myopic shift by SI40NB (AMO, USA) with PMMA haptics. This phenomenon was thought to be an effect of polypropylene which has low shape memory and high flexibility. Na et al.22 used Centerflex® (Rayner, UK), similar to C-flex, and experienced the hyperopic shift of +0.20 D, and Nishi et al6 reported +0.30-+0.50 D hyperopic shift, similar with the results from our study. Kim and Tchah23 reported a myopic shift of -0.41 D at 6 months postoperatively by using hydrophilic acrylic IOL (ACR6D, CORNEAL®, France). From these studies, we can see that the materials and shapes of IOL highly influence the difference between the predicted and actual RE, thus knowledge of the specific RE predictive value for each IOL would be crucial to acquire an accurate surgical outcome.
In our study, the difference of surgical wound approach (clear cornea incision in group 1, scleral tunnel incision in group 2) may influencethe result on RE, and may be thought to be a limitation of our study. But, Kim et al.24 previously reported no significant difference by surgical approach.
Danjo et al.25 reported the cause of myopic shift after the vitrectomy to be the replacement of vitreous with aqueous humor with lower refractive index (vitreous: 1.334, aqueous humor: 1.333) and the change in anterior chamber depth. The difference of refractive index is reported to affect about -0.13 D in myopic shift. Suzuki et al.26 experienced a myopic shift of -1.0 D after the vitrectomy. Concerning the anterior chamber depth change by vitrectomy, Shioya et al.27 reported the contracture of posterior lens capsule after vitrectomy, inducing myopia by -0.05 D with an anterior positioning of IOL. In the other hand, Nishigaki et al.28 reported the hyperopic shift after vitrectomy by deepening the anterior chamber depth. If the contracture of posterior capsule does decrease anterior chamber depth influenced by material and shape of IOL, the postoperative RE would be affected by anterior chamber depth.
Kim et al.29 explained the development of myopia after the vitrectomy and gas injection by anterior disposition of IOL by prone position and gravity. Choi et al.30 performed the vitrectomy with gas injection to the patients with macular hole, and reported -0.71 D of myopic shift, and -0.65 D in additional cataract extraction surgery. In our study, +0.03 D of RE was noted in the patients without gas injection where -0.15 D in the patients with gas injection, and this difference was not significant. (p>0.05)
Jeoung et al.31 revealed the difference of axial length by retinal detachment of macula, affecting postoperative RE. Kovacs et al.32 reported the difference of postoperative RE from predicted by -0.79 D in patients with the combined surgery of cataract extraction, vitrectomy and epiretinal membrance removal, due to lengthened axial length by decreased macular thickness. But, in our study, none of vitreoretinal technique or disorders such as internal limiting membrane removal, macular hole, epiretinal membrane or macular edema had significant effect on the postoperative RE (Table 6).
The authors showed the postoperative RE close to the predicted value in 85.9% with the use of C-flex IOLs in the cataract extraction surgery alone, but C-flex may manifest +0.26 D of hyperopic shift than predicted. Also, we revealed a combined surgery with vitrectomy would induce -0.22 D difference from the predicted. From the results, we found that vitrectomy may induce 0.46 D of myopic shift compared with cataract extraction surgery. And also, the myopic effect of a combined surgery of cataract extraction and vitrectomy and the hyperopic effect of vitrectomy would equalize postoperative RE, thus maintaining postoperative RE near the predicted value. Vitrectomy and various techniques in vitreoretinal surgery which turned out to be not significant in our study are thought to induce myopic effect on postoperative RE. Knowledge of these effects on the postoperative RE after C-flex IOL implantation may produce more accurate postoperative results.
Figures and Tables
Fig. 1
The C-flex 570C IOL with an enhanced 360-degree, square-edged design. (From Nishi Y et al. J Cataract Refract Surg 2007;33:227-31)

Fig. 2
Changes of predicted SE and actual SE in Group 1 and Group 2 at 1 month and 6 months postoperatively. Group 1 was shifted more hyperopic than predicted values at 1 month and 6 months. Group 2, on other hand, was shifted more myopic at 1 month but more hyperopic at 6 months. Group 2 was closer to predicted refractive errors.
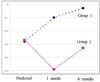
Table 3
Distributions of refractive prediction errors in Group 1 and Group 2 at postoperative 1 month and 6 months

Table 4
Predicted and actual spherical equivalent (SE) and refractive prediction errors in Group 1 and Group 2 at 1 month and 6 months postoperatively

Table 5
Predicted and actual SE and refractive prediction errors as parameter in Group 2 at 6 months postoperatively

*SE=spherical equivalent; †Prediction Error=Actual minus Predicted SE; ‡ILM=Inner limiting membrane; §ERM=Epiretinal membrane; Predicted SE versus actual SE (paired t test, p<0.05); There is no significant difference between all parameters (paired t test, p=0.193, p=0.907, p=0.484, p=0.315, p=0.941).
References
1. Demetriades AM, Gottsch JD, Thomsen R, et al. Combined phacoemulsification, intraocular lens implantation and vitrectomy for eyes with coexisting cataract and vitreoretinal pathology. Am J Ophthalmol. 2003. 135:291–296.
2. Senn P, Schipper I, Perren B. Combined pars plana vitrectomy, phacoemulsification and intraocular lens implantation in the capsular bag: a comparison to vitrectomy and subsequent cataract surgery as a two-step procedure. Ophthalmic Surg Lasers. 1995. 26:420–428.
3. Honjo M, Ogura Y. Surgical results of pars plana vitrectomy combined with phacoemulsification and intraocular lens implantation for complications of proliferative diabetic retinopathy. Ophthalmic Surg Lasers. 1998. 29:99–105.
4. Scharwey K, Pavlovic S, Jacobi KW. Combined clear corneal phacoemulsification, vitreoretinal surgery, and intraocular lens implantation. J Cataract Refract Surg. 1999. 25:693–698.
5. Koenig SB, Han DP, Mieler WF, et al. Combined phacoemulsification and pars plana vitrectomy. Arch Ophthalmol. 1990. 108:362–364.
6. Nishi Y, Rabsilber TM, Limberger IJ, et al. Influence of 360-degree enhanced optic edge design of a hydrophilic acrylic intraocular lens in posterior capsule opacification. J Cataract Refract Surg. 2007. 33:227–231.
7. Vyas AV, Narendran R, Bacon PJ, Apple DJ. Three-hundred-sixty degree barrier effect of a square-edged and an enhanced-edge intraocular lens on centripetal lens epithelial cell migration; Two-year results. J Cataract Refract Surg. 2007. 33:81–87.
8. Werner L, Mamalis N, Pandey SK, et al. Posterior capsule opacification in rabbit eyes implanted with hydrophilic acrylic intraocular lenses with enhanced square edge. J Cataract Refract Surg. 2004. 30:2403–2409.
9. Kleinmann G, Apple DJ. Evaluation of a new soft tipped injector for the implantation of foldable intraocular lenses. Br J Ophthalmol. 2007. 91:1070–1072.
10. Taskapili M, Gulkilik G, Engin G, et al. Transscleral fixation of a single-piece hydrophilic foldable acrylic intraocular lens. Can J Ophthalmol. 2007. 42:256–261.
11. Oner FH, Saatci OA, Sarioğlu S, et al. Interaction of intraocular lenses with various concentrations of silicone oil: an experimental study. Ophthalmologica. 2003. 217:124–128.
12. Steinert RF, Brint SF, White SM, Fine IH. Astigmatism after small incision cataract surgery: a prospective, ramdomized, multicenter comparison of 4-and 6.5-mm incisions. Ophthalmology. 1991. 98:417–424.
13. Levy JH, Pisacano AM, Chadwick K. Astigmatism changes after cataract surgery with 5.1mm and 3.5mm sutureless incision. J Cataract Refract Surg. 1994. 20:630–633.
14. Menapace R, Yalon M. Exchange of IOGEL hydrogel one piece foldable intraocular lenses for bag-fixated J-loop poly (methylmethacrylate) intraocular lens. J Cataract Refract Surg. 1993. 19:425–430.
15. Olsen T. Sources of error in intraocular lens power calculation. J Cataract Refract Surg. 1992. 18:125–129.
16. McEwan JR, Massengil RK, Friedel SD. Effect of keratometer and axial length measurement errors in primary implant power calculations. J Cataract Refract Surg. 1990. 16:61–70.
17. Hoffer KJ. Modern IOL power calculations: Avoiding error and planning for special circumstances. Focal Point. 1999. 17:12.
18. Holladay JT. Standardising constants for ultrasonic biometry, keratometry and intraocular lens power calculations. J Cataract Refract Surg. 1997. 23:1356–1370.
19. Assia EI, Legler UFC, Castaneda VE, Apple DJ. Loop memory of posterior chamber intraocular lenses of various size, and loop materials. J Cataract Refract Surg. 1992. 18:541–546.
20. Chang JH, Lim SJ, Kim HB. Clinical evaluation of AMO Phacoflex SI-30NB in the aspect of A-constant. J Korean Ophthalmol Soc. 1999. 40:987–994.
21. Kim YE, Cho BJ, Lee KS. The evaluation of the difference between the calculated estimated post-operative refraction and the real post-operative refraction for five types intraocular lenses. J Korean Ophthalmol Soc. 2003. 44:1059–1065.
22. Na SJ, Park JS, Choi SK. Clinical Results of Centerflex® intraocular ocular lenses and Acrysof® intraocular ocular lenses in bilateral cataracts. J Korean Ophthalmol Soc. 2004. 45:1066–1074.
23. Kim JY, Tchah HW. The clinical results of hydrophilic acrylic lens. J Korean Ophthalmol Soc. 2001. 42:1562–1570.
24. Kim JH, Kang SM. Comparison of scleral tunnel and clear cornea incision in phacoemulsification combined with pars plana vitrectomy. J Korean Ophthalmol Soc. 2006. 47:1583–1588.
25. Danjo Y, Matsuda H, Maeno T, et al. Catatact surgery for avitreous eyes-postoperative refractive prediction folia. Ophthalmologica Japonica. 1993. 44:1243–1247.
26. Suzuki Y, Sakuraba T, Mizutani H, et al. Postoperative refractive error after simultaneous vitrectomy and cataract surgery. Ophthalmic Surg Lasers. 2000. 31:271–275.
27. Shioya M, Ogino N, Shinjo U. Change in postoperative refractive error when vitrectomy is added to intraocular lens implantation. J Cataract Refract Surg. 1997. 23:1217–1220.
28. Nishigaki S, Inaba I, Minami H, et al. The postoperative change of depth of anterior chamber, refraction and anterior capsulorhexis size after intraocular lens implantation. Nippon Ganka Gakkai Zasshi. 1996. 100:156–158.
29. Kim DH, Kim SK, Koh HJ, Kwon OW. Postoperative refractive error in combined operation of vitrectomy and intraocular lens implantation. J Korean Ophthalmol Soc. 2002. 43:1644–1648.
30. Choi YJ, Kim CG, Kim SH. Postoperative refractive error after vitrectomy in macular hole patients. J Korean Ophthalmol Soc. 2003. 44:1813–1817.
31. Jeoung JW, Chung H, Yu HG. Factors influencing refractive outcomes after combined phacoemulsification and pars plana vitrectomy Results of a prospective study. J Cataract Refract Surg. 2007. 33:108–114.
32. Kovács I, Ferencz M, Nemes J, et al. Intraocular lens power calculation for combined cataract surgery, vitrectomy and peeling of epiretinal membranes for macular oedema. Acta Ophthalmol Scand. 2007. 85:88–91.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download