Abstract
Purpose
To investigate the effect of unilateral medial rectus muscle resection for recurrent exotropia after bilateral lateral rectus muscle recession for intermittent exotropia
Methods
A retrospective analysis was made of thirtypatients who underwent unilateral medial rectus resection for recurrent exotropia. All had prior bilateral lateral rectus recession for intermittent exotropia. Data were collected for age, the preoperative deviation, the postoperative deviation at 2 weeks, 3 months, 6 months and the last visit, and the amount of medial rectus resection performed.
Results
The average preoperative deviation was 27.0±3.6 PD. After unilateral medial rectus resection, average deviation at distance was 2.8 PD at postoperative 2 weeks, 4.5 PD at 3 months, 5.1 PD at 6 months and 5.8 PD at last visit. The average deviation corrected per millimeter of medial rectus resection was 3.53±0.17 PD/mm.
The intermittent exotropia [X(T)] can be cured mainly through surgery but significant portion of patients have undercorrection or recurrence of exotropia at postoperative follow-up.1,2 The rate of recurrence or undercorrection of X(T) is increasing with time and these patients are usually treated by bilateral medial rectus (MR) resection, re-recession of previously recessed lateral rectus (LR) or unilateral LR recession and MR resection (R&R), according to the methods of the previous surgery.3-6
The one muscle surgery has advantages of requiring less time, less anesthesia and placing only one eye at risk for any possible surgical complication.3 Furthermore, there are more risks of overcorrection in the second surgery than the first surgery because of the smallerdeviation of the recurred X(T).7-9 It has been reported that the unilateral MR or LR recession is effective and predictable surgical method for small to moderate angle deviations.10,11
Therefore, we performed this study to evaluate the efficacy of the unilateral MR resection for the patients of recurred X(T) who had undergone bilateral LR recession as their previous surgery.
A retrospective analysis was made of all the patients who had undergone unilateral MR muscle resection between March 1995 and February 2007 for recurred X(T), which developed after bilateral LR recession.
There are 5 exclusion criteria for this retrospective study. These parameters were: (1) presence of other ocular disease (central nervous system abnormalities or anatomic abnormalities of the eye), (2) presence of amblyopia which include more than two lines of visual acuity difference, (3) presence of paralytic strabismus, (4) presence of dissociated vertical deviation or dysfunction of oblique muscles, and (5) infantile exotropia were excluded from this study.
The following parameters were reviewed and analyzed: patient age, gender, deviation before 1st surgery, deviation before 2nd surgery, postoperative deviations according to follow-up duration, ocular motility and the amount of surgery performed.
All patients in this study had a complete ophthalmologic examination prior to surgery. A cycloplegic refraction was performed using 1% cyclopentolate and 0.5% tropicamide. Visual acuities were measured by Snellen's chart or 'E' chart. The distant and near deviation angles were measured at 6 and 0.33 m by alternate prism cover test, if not possible, by Krimsky methods. The angle measurements of the preoperative deviation and the postoperative deviation at 1 day, 2 weeks, 3 months, 6 months and the last visit were done. Titmus ring test was performed preoperatively and at 3 months postoperatively.
Unilateral MR resections were performed on the non-fixating eye or on the left eye if the patient had an alternative fixation behavior by one of the authors (JYK). Under the general anesthesia, surgeon made a limbal incision, exposed and resected the MR muscle 5 to 7 mm according to their deviation angle.
We defined the success of the surgery as being orthophoric or having deviation angle less than 10 PD of distant manifest deviation at postoperative 6 months of follow-up. We defined the recurrence as 10 PD or more exodeviation at distance and the overcorrection as 10 PD or more esodeviation at distance at postoperative 6 months of follow-up. The survival was defined as the duration until developing exodeviation more than 10 PD after unilateral MR resection and made Kaplan-Meier survival analysis.
Thirty patients who had undergone unilateral MR resection for recurred XT after bilateral LR recession were included in this study. The descriptive data of these subjects are demonstrated in Table 1. The mean age at bilateral LR recession was 7.2±5.1 year and 9.1±5.4 year at unilateral MR resection. The median time interval between the previous surgery and the recurrence of exodeviation was 9 months (range 3 to 72 months). The mean deviation angle before bilateral LR recession was 41.2±5.8 PD at distance and 39.5±4.8 PD at near. And the mean deviation angle before unilateral MR resection was 27.0±3.6 PD at distance and 24.5±4.2 PD at near. No close relationship was found between deviation angles before bilateral LR recession and those before unilateral MR resection (p>0.05). All of the patients were diagnosed as intermittent exotropia of basic type. No patient demonstrated a noticeable limitation of abduction.
The amount of the unilateral MR resection was decided as 5.0 mm for 20~24 PD, 6.0 mm for 25~29 PD, 6.5 mm for 30~34 PD and 7.0 mm for 35~39 PD. However, there was intraoperative adjustment of the amount of MR resection. For example, if MR muscle seemed to be thinner or looser than usual, the surgeon added 0.5 mm to the planned amount of resection. If MR was found slightly tighter than usual, the surgeon subtracted 0.5 mm from planned resection. In addition, if recurrence of exotropia had occurred early (≤3 months) after previous surgery, the surgeon added 0.5 mm to the planned MR resection and subtracted 0.5 mm when overcorrection was specially concerned due to patients' young age (≤4 years). Among 30 patients, 19 patients had no adjustment to planned amount of MR resection. The surgeon added 0.5 mm to the amount of planned MR resection to 2 patients having 30~34 PD and 3 patients having 25~29 PD, and subtracted 0.5 mm from 6 patients having 25~29 PD.
Table 2 shows the average amount of corrected exodeviation per millimeter of resection performed on the unilateral MR. The average amount of MR resection was 6.1 mm (range 5.0 to 7.0 mm). The average deviation corrected per millimeter of MR resection was 3.53±0.17 PD/mm.
There was no statistically meaningful correlation between the amount of previous LR recession and the amount of MR resection (Pearson's correlation r=0.212, p=0.261).
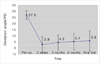
Fig. 1 demonstrates the distribution of the distant deviation angle after the unilateral MR resection for recurred X(T). Postoperative mean deviation angle at distance was 2.8 PD at 2 weeks, 4.5 PD at 3 months, 5.1 PD at 6 months and 5.8 PD at last follow-up. Postoperative mean deviation angle at near was 1.5 PD at 2 weeks, 3.8 PD at 3 months, 4.1 PD at 6 months and 5.1 PD at last follow-up.
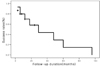
At 6 months postoperatively, 24 (80%) patients had successful outcome, whose ocular alignments within 10 PD of orthophoria, 6 (20%) patients were undercorrected, whose ocular alignment was more than 10 PD of exodeviation, but no patient showed overcorrection more than 10 PD of esodeviation (Table 3). Fig. 2 demonstrates the success rate according to follow-up duration after unilateral MR resection. According to this Kaplan-Meier survival analysis, the mean survival duration was 38 months (3~96 months) and success rate showed a tendency of stepwise decrease during follow-up. After 16 months of unilateral MR resection, success rate decreased to 75% (among 13 patients), 50% after 29 months (among 5 patients) and 29.1% after 48 months (among 3 patients).
Statistical analysis was made to demonstrate the correlation of clinical characteristics between the patients with successful outcome and the patients with undercorrection after unilateral MR resection for recurred X(T). There was no statistical difference of the age of unilateral MR resection, the duration from the recurrence to reoperation, the deviation angle of bilateral LR recession and the deviation angle of unilateral MR resectionbetween the patients of successful outcome and the patients of undercorrection (p>0.05). Preoperative mean streopsis was 67.7 arc secs and increased to 58.3 arc secs postoperatively, but there was no statistically meaningful difference after surgery (p>0.05).
In the present study, the efficacy of the unilateral MR resection were evaluated in the patients of recurred X(T) who had undergone bilateral LR recession. Our data shows that the success rate of this procedure was 80% at postoperative 6- month follow-up and 76.7% at last visit (mean 16.4 months). According to the Kaplan-Meier survival analysis, the mean duration from this procedure to having exodeviation more than 10 PD was 38 months (3~96 months) and success rate showed a tendency of stepwise decrease during follow-up.
Surgical results of the present study are in close agreement with those of several authors who reported their success rates of the unilateral MR resection for recurred X(T) were 82% to 82.9% at 6 months follow-up.12,13 However, Kim and Kim13 included the patients who had undergone not only bilateral LR recession but also unilateral R&R, unilateral R&R with fellow eye LR recession and unilateral MR resection as previous surgeries of X(T). Our study focused specially on patientsof recurred X(T) who had undergone only bilateral LR recession to have a homogenous baseline characteristics of subjects of this study.
The success rate of this study is slight different from the result of Olitsky et al.3 who reported the success rates of unilateral MR resection as a reoperation of undercorrected or recurrent exotropia were 95.2% at 6-month follow-up. We speculate that the reason for their higher success rate may be their smaller preoperative deviation angle (mean 16.6 PD) and larger number of the previous surgeries (average 1.2 times). Furthermore, the surgical methods of previous surgeries were not clarified in their studies.
Postoperative mean deviation angle at distance after unilateral MR resection was 2.8 PD at 2 weeks, 4.5 PD at 3 months, 5.1 PD at 6 months and 5.8 PD at last follow-up (mean 16.4 months). The patient who had been overcorrected over 10 PD was not found in this study. These results are consistent with those of the earlier studies. Kim and Chang9 reported exodrift of 2.7 PD after unilateral LR recession at postoperative 3 months. Kim and Kim13 reported exodrift of 5.4 PD after unilateral MR resection at postoperative 6 months and Hahm et al.8 reported that there was exodrift of 5.6 PD after unilateral R&R at postoperative 18 months. Although many different surgical methods had been used, nevertheless, there were similar amount of exodrift after surgeries of recurred X(T).8,9,13
In this study, preoperative mean deviation angle was 27.0±3.6 PD and there was no meaningful relationship between preoperative deviation angles of bilateral LR recession and those of unilateral MR resection (p>0.05). Result of the present study is correspond with earlier studies which reported that the amount of exodeviation of the second surgery is significantly smaller than the first surgery of X(T).7,9 And this is the basis of performing unilateral MR resection to recurred or undercorrected X(T).
The average deviation corrected per millimeter of MR resection was 3.53±0.17 PD/mm. Our results were not very different from those of Kim and Kim13 who reported that their average deviation corrected was 3.41±0.60 PD/mm. Olitsky et al.3 reported that there was some variability in the amount of correction obtained per millimeter of muscle resected. They explained that this variability might be related to the methods and the amount of previous surgery which were not obtainable by authors. Table 2 shows that there was no statistically apparent variability in the amount of deviation corrected per millimeter of the MR resection in regard of total amount of MR resection (Pearson's correlation r=-0.225, p=0.232). We speculate that these results may be due to the uniform method of previous surgery and the absence of ocular motility restriction which could affect surgical results of this procedure.
However, we cannot draw conclusions that our results of unilateral MR resection are even and predictable because of its small sample size, retrospective design and slight different amount of MR resection among patients having same deviation angle. In addition, we did not take into consideration of the amount of previous LR recession and only decided the amount of MR resection by deviation angle of recurred exotropia. Authors are planning further study regarding the effect of the amount of previous LR recession to results of unilateral MR resection to develop a predictable nomogram of this procedure for recurred X(T). Furthermore, it might be necessary to compare success rates and surgical complications between the patients who underwent unilateral MR resection and those who underwent bilateral MR resection as reoperation of recurred X(T) after bilateral LR recession.
In conclusion, unilateral MR resection may be an effective surgical method for the treatment of recurrent exotropia after bilateral LR recession, and this procedure has the merit of limiting surgery to only one eye. We recommend this procedure in patients with recurrent exotropia with small to moderate deviation angles.
Figures and Tables
Fig. 1
Distribution of the mean deviation angle according to follow-up duration after unilateral MR resection for recurrent exotropia.
References
1. Scott WE, Keech R, Marsh AJ. The postoperative results and stability of exodeviations. Arch Ophthalmol. 1981. 99:1814–1818.
2. Hahm KH, Shin MC, Sohn MA. The change in deviation angle with time cource after surgical correction of intermittent exotropia. J Korean Ophthalmol Soc. 2002. 42:2220–2226.
3. Olitsky SE, Kelly C, Lee H, Nelson LB. Unilateral rectus resection in the treatment of undercorrected or recurrent strabismus. J Pediatr Ophthalmol Strabismus. 2001. 38:349–353.
4. Parks MM, Mitchell PR. Tamsan W, Jaeger E, editors. Concomitant exodeviations. Clinical ophthalmology. 1991. vol. 1. Philadelphia: JB Lippincott;chapter 13.
5. Yazdian Z, Ghiassi G. Re-recession of the lateral rectus muscles in patients with recurrent exotropia. J AAPOS. 2006. 10:164–167.
6. Kang SJ, Jang JH. Motility restriction after resection of an extraocular muscle. Korean J Ophthalmol. 2001. 15:133–136.
7. Sohn JH, Chang BL. Management for reoperation in recurrent exotropia. J Korean Ophthalmol Soc. 1994. 36:2661–2665.
8. Hahm IR, Yoon SW, Baek SH, Kong SM. The clinical course of recurrent exotropia after reoperation for exodeviation. Korean J Ophthalmol. 2005. 19:140–144.
9. Kim JY, Chang BL. The effect of unilateral lateral rectus recession in recurrent exotropia. J Korean Ophthalmol Soc. 1995. 36:2261–2265.
10. Grin TR, Nelson LB. Large unilateral medial rectus muscle recession for the treatment of esotropia. Br J Ophthalmol. 1987. 71:377–379.
11. Olitsky SE. Early and late postoperative alignment following unilateral lateral rectus recession for intermittent exotropia. J Pediatr Ophthalmol Strabismus. 1998. 35:146–148.
12. Mims JL 3rd. Outcome of 5 mm resection of one medial rectus extraocular muscle for recurrent exotropia. Binocul Vis Strabismus Q. 2003. 18:143–150.
13. Kim SC, Kim MM. The efficacy of unilateral rectus resection in the reoperation of strabismus. J Korean Ophthalmol Soc. 2003. 44:904–910.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download