This article has been
cited by other articles in ScienceCentral.
Abstract
Purpose
To analyze postoperative results of intermittent exotropia as a function of the difference in strabismic angles measured immediately and another time prior to the surgery.
Methods
We reviewed the clinical records of intermittent exotropia patients who received surgery and had differences greater than or equal to 10 prism diopters (PD) between the last preoperative measurement of strabismic angle and another previous measurement. After applying various exclusion criteria, 66 patients were entered into our study. At the last follow-up visit after surgery, we divided postoperative results into 3 categories: (1) poor; with greater than 10 PD of esotropia or angle of exodeviation of 20 PD or more (2) moderate; with 6-10 PD of esophoria/tropia or 10-19 PD exodeviation, or (3) good; with 1-5 PD of esophoria / tropia or an angle of exodeviation less than 10 PD, or orthophoria.
Results
Good results were higher in patients where the difference in strabismic angle was 10 PD or greater between the last measurement and any other earlier measurement.
Conclusions
In cases of Intermittent exotropia where the last preoperative value of strabismic angle was greater than any previous preoperative measurement, surgical dosage based on the last preoperative measurement yielded better results.
Keywords: Intermittent exotropia, Strabismic angle, Surgical results
The aim of strabismus surgery is to straighten the eyes in the primary position. The outcome of strabismus surgery shows great variability among patients.
1 Although most patients with intermittent exotropia show a stable exotropic angle with the repeated preoperative measurements, some patients show variable angles of exotropia. According to Pritchard,
2 the simplest and most obvious potential explanation for a high rate of recurrence of intermittent exotropia is that we are not operating at the full angle of deviation. Variability in the measurement of exotropia from one examination to the next examination supports this idea. This study was designed to analyze postoperative results of intermittent exotropia in patients with 10 or more prism diopters (PD) difference between any other preoperative measurements and the last preoperative measurement taken on the day of admission, or the day before. We hypothesize that preoperative variability in the measurement of exotropia could influence the postoperative results and could serve as the strongest predictor for a successful surgical outcome.
Materials and Methods
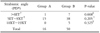
Patients with 10 or more prism diopters (PD) difference in strabismic angle between the preoperative and any other previous measurement were retrospectively reviewed. These were clinical patients with intermittent exotropia who had received their surgery in the ophthalmology department of Yeungnam University Hospital since 1988. Patients with a last preoperative measurement of strabismic angle of 10 PD or less than any other previous measurement comprised group A, and patients with a last preoperative measurement of strabismic angle of 10 PD or more than any previous measurement comprised group B. All patients were measured and operated on by one surgeon (MMK), who made each measurement at least 4 times. Before surgery, we calculated the correction using the alternative prism cover test according to surgical dosage as indicated in
Table 1. The surgery was done following the last preoperative measurement which was performed the day before. All patients were treated by lateral rectus recession in both eyes or recession and resection in one eye under general anesthesia. For the purpose of this study, only those patients who had pure intermittent exotropia were included. Excluded were all patients age 14 or older, patients with amblyopia, or a postoperative follow-up less than 6 months, manifest or latent nystagmus, extraocular muscle palsy, dissociated strabismus complex, mechanical cause for strabismus, concomitant vertical muscle surgeries, neurologic abnormalities, developmental delay, mental retardation, any organic lesion of the orbit or eye, or any form of incomitant deviation including an A- or V-pattern deviation or oblique muscle dysfunction. At the last follow-up visit after surgery, postoperative results were separated into 3 categories according to the magnitude of postoperative deviations to represent the quality of postoperative results: (1) poor, with values of greater than 10 PD for esotropia or exodeviation of 20 PD or more (2) moderate, with 6-10 PD for esophoria/tropia or 10-19 PD exodeviation, or (3) good, with values of 1-5 PD for esophoria/tropia or exodeviation less than 10 PD.
Data was analyzed using SPSS/PC (version 10.0). Tests for significance included the chi-square test and Fisher's exact test for categorical data and the unpaired t-test for interval and continuous data. Values of P<.05 were considered statistically significant.
Results
A total of 66 patients satisfied the entry requirements for this study. Patients were divided into two groups to analyze postoperative results of intermittent exotropia based on differences in preoperative measurement of strabismic angle as described above. There were 16 subjects in group A, and 50 subjects in group B. The mean age at the first detection of strabismus was 26 months old (5-72 months) in group A, and 28 months old in group B (3-96 months). Patients underwent strabismic surgery at the average age of 79 months in group A (49-129 months), and 78 months in group B (44-159 months). The sex ratio (male : female) was 3:13 in group A, and 22:28 in group B. The average follow-up time after surgery was 31 months in group A, and 30 months in group B.
The last measurement of strabismic angle was on the day of, or the day before surgery, as listed in
Table 2. Surgery was undertaken following the last preoperative measurement. Short-term results the first week after surgery showed the following. Group A had 1 patient with esotropia of 6 PD or more, 15 patients with a range of esotropia of 5 PD to 9 PD for exotropia, but no patients in the exotropia range of 10 to 19 PD. In group B, there were 7 patients who had an esotropia PD value of 6 or more, 38 patients with esotropia PD values between 5 PD esotropia to 9 exotropia, and 5 patients with exotropia PD values between 10and 19 (
Table 3). Long-term results of the surgery from the last follow-up visit are given in
Table 4. The follow-up duration was at least 6 months. There were no patients in group A and B with estropia strabismic angle values of 6 PD or greater. For Strabismic angles from 5 PD esotropia to 9 PD exotropia, there were 3 patients in group A and 22 in group B. For Strabismic angles from 10 to19 PD exotropia, there were 10 patients in group A and 14 in group B. There are 3 patients in group A and 14 patients in group B who had strabismic angles of 20 PD exotropia or more. Of these, 3 cases were classified as poor, 10 cases were moderate, and 3 cases were good in the postoperative results of group A. In the group B, poor cases accounted for 14 cases, while 14 cases were moderate and 22 cases were good. The incidence of good cases was higher in group B (44.0%) than in group A (18.8%), but there was no statistical significance (
Table 5) (P=0.083).
After the first week of surgery, there was one patient in group A with esotropia of 6 PD or more and this case were good (100%) at the last follow up. In range of esotropia of 5 PD to 9 PD exotropia, there were 15 patients and among them, 2 cases became good (13%). In Group B with esotropia of 6 PD or more, there were 7 patients and all of these cases were good (100%) at the last follow up. In the range of esotropia of 5 PD to exotropia of 9 PD exotropia, there were 38 patients and among them, 15 cases were good (39%). There were no good cases among the 5 patients whose strabismic angles were in range of 10 PD exotropia to 19 PD exotropia.
Discussion
There have been many assumptions about factors that affect the surgical outcomes of intermittent exotropia. Keenan and Willshaw
3 discussed the factors affecting the final outcomes including age of onset, age at the time of surgery, preoperative and post-operative amblyopia, refractive error, anisometropia, surgical procedure used, and postoperative ocular alignment. Several authors have suggested an interrelation between good postoperative results and initial postoperative overcorrections.
4-
6 Because the preoperative deviation is presumed to be an important determinant for strabismus surgery in intermittent exotropia, the correct measurement of preoperative angles of deviation would be expected to influence the final results, and thus, the surgery should be performed for the largest angle measured.
7-
8 Kim and Hwang
9 suggested that the surgical dosage for intermittent exotropia should be based on the largest angle ever measured. The extent to which an exodeviation is controlled by fusion depends not only on the size of the angle but also to a large extent on the general health, alertness, attention span, and the level of anxiety of the patient at the time of examination.
10-
13 This can also explain the variability of measurements as well as the intermittency of exodeviation. Von Noorden
13 suggested that considerable variation in the degree of fusional control from one examination to another is not a surprising finding. It is less likely that such variability is due to simple error of measurement such as a patient's voluntary convergence with accommodative spasm, because all measurements were repeatedly performed by the same strabismologist at the same distance using the same accommodative targets.
9 There could be considerable variability in exotropic angle even when measured by the same observer. Although the exact mechanism of the variability is not known, the determination of the optimum surgical dosage in such cases is a critical and practical issue for all strabismic surgeons. Our idea is that surgical dosage based on the last preoperative measurement could be safe in intermittent exotropes with the last measurement of strabismic angles 10 or more PD units larger or 10 or more PD units smaller than that of earlier preoperative measurements. As far as we know, this hypothesis has never been tested. Our study was designed to evaluate the safety of this approach by assessing the postoperative results. When the surgical dosage was determined according to the last preoperative measurement, there were two troublesome issues, the risk of persistent overcorrection and undercorrection.
14-
15 In this study, there was no overcorrection of more than 6 PD of esotropia distal or proximal in the final follow-up and there were only 3 patients with under-correction such that the last preoperative measurement of strabismic angle was smaller than that of earlier preoperative measurements. The incidence of good cases in patients with the last measurement of strabismic angle of 10 PD or larger than an earlier preoperative measurement were higher than the incidence of good in patients where the last measurement of strabismic angle was 10 PD or less than a preoperative measurement. We defined a good case as one where the surgery was successful. There was 1 patient in group A where the early postoperative overcorrection was greater than 6 PD esotropia and 7 such patients in group B. This can be explained by the differences in early postoperative overcorrection between the two groups, and the lowered surgical dosage used for group A. Thus, we analyzed the ratio of good outcomes at the last follow up visit for each strabismic angle in the first week after surgery between the two groups. As we mentioned previously, despite the lack of statistical significance. group B had better surgical outcomes. However, the study needs to be viewed in light of prospective and randomized further work-ups.
In conclusion, in cases of Intermittent exotropia where the last preoperative value of strabismic angle was greater than any previous preoperative measurement, surgical intensity based on the last preoperative measurement yielded better results.






 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download