Abstract
Simulated Brown syndrome is a term applied to a myriad of disorders that cause a Brown syndrome-like motility. We encountered a case of acquired simulated Brown syndrome in a 41-year-old man following surgical repair of fractures of both medial orbital walls. He suffered from diplopia in primary gaze, associated with hypotropia of the affected eye. We performed an ipsilateral recession of the left inferior rectus muscle as a single-stage intraoperative adjustment procedure under topical anesthesia, rather than the direct approach to the superior oblique tendon. Postoperatively, the patient was asymptomatic in all diagnostic gaze positions.
Brown syndrome, a congenital or acquired, ocular motility disorder, is characterized by impaired elevation in the adduction of the affected eye. This syndrome is believed to be secondary to restriction of the superior oblique muscle in the trochlea/tendon complex that causes a tethering of the muscle when the eye is adducted.1,2 Currently, the term "Brown syndrome" is often broadly applied to a myriad of disorders that cause a Brown syndrome-like motility pattern. Such disorders, better collectively termed "simulated Brown syndrome",4 have been reported from a wide variety of causes, including autoimmune inflammatory conditions, infections, and orbital trauma. Surgical trauma may also lead to Brown syndrome, and various cases have occurred following sinus surgery, blepharoplasty, retinal detachment surgery, glaucoma drainage implants and peribulbar local anesthesia.3-6 Herein we present a patient who developed simulated Brown syndrome following surgical repair of fractures of both medial orbital walls.
A 41-year-old man presented to our institution with a 7-month history of vertical diplopia. Eight months before he had been struck in the region of both orbits by a man's fist while wrestling. He was examined at his local hospital where he was diagnosed with bilateral medial orbital wall fractures and 1 week after the injury he underwent surgical repair of the fractures with porous polyethylene implants (Medpor®) insertion bilaterally by a plastic surgeon. He stated that he had had diplopia from 1 week after the operation and had not felt any improvement since then. He complained of vertical diplopia in primary, straight up, right, and right up gaze positions. He also had pain in the region of the left trochlea on attempted elevation in adduction.
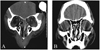
On examination, visual acuity of both eyes was 20/20. Eye movement of the left eye was markedly limited on elevation in adduction. The diplopia was most obvious in that gaze position. Horizontal and downward ductions of the left eye were full. Extraocular motility in the right eye was normal. Prism cover test at distance fixation revealed 6 prism diopters (PD) of left hypotropia in primary position, which increased to 12 PD in horizontal right gaze, 20 PD in straight upgaze, and a further 30 PD in right upgaze (Fig. 1). He was orthophoric in other gaze positions. Forced duction test of the left eye demonstrated restricted elevation in adduction. Computerized tomography (CT) scan of the orbits showed adequate reduction of the fractures, but they also suggested questionable thickening of the left trochlear area and adjacent superior oblique tendon (Fig. 2). A porous polyethylene sheet was observed directly overlying the region of the left trochlea. Anterior segment and fundus examinations were unremarkable. A diagnosis of acquired simulated Brown syndrome was made.
Initially, we recommended him to wear prism glasses, but he remained uncomfortable with these and was not willing to wear them any longer. The diplopia was most troublesome to him while looking up, and it interfered significantly with his ability to work as a construction worker. He therefore strongly wished to undergo surgery.
Since the primary aim of treatment was the symptomatic relief of the troublesome diplopia while looking up, we chose left inferior rectus weakening surgery rather than superior oblique tendon surgery. We performed a 2-mm recession of the left inferior rectus muscle as a single-stage intraoperative adjustment procedure under topical anesthesia, at 9 months after the initial surgical repair of the orbital wall fracture. One month after this strabismus surgery, the patient remained asymptomatic and orthophoric in all diagnostic gaze positions except right upgaze (Fig. 3), in which he had only a small amount of vertical deviation which was within the fusible range. Forced duction test was negative. His results remained satisfactory for 8 months of follow-up.
Surgical procedures to repair a medial orbital wall fracture are considered a possible cause of simulated Brown syndrome. Because of its anatomical proximity, the superior oblique is at risk of surgical trauma, especially during medial orbital wall or sinus surgery. The superior oblique muscle or tendon may be damaged directly or indirectly during surgical procedures, and may later be fibrosed by cicatricial adhesions.2 The authors postulate that the development of the acquired simulated Brown syndrome in this case was possibly related to a variety of perioperative complications. Not only direct or indirect trauma by the porous polyethylene sheet, but also edema, inflammation, or hemorrhage may have played a role in the pathogenesis of this characteristic ocular motility disorder near the superior nasal quadrant, involving the trochlea and superior oblique tendon. In contrast to the marked limitation of elevation in primary position and adduction, the absence of any elevation deficiency in the abducted position suggests the pathology of the superior oblique/trochlear complex rather than that of the inferior rectus muscle.
Surgery for Brown syndrome is indicated if diplopia is present in primary gaze, is associated with hypotropia of the affected eye, or if there is an abnormal head position assumed by the patient to maintain single binocular vision.7 Superior oblique weakening surgery has remained a mainstay in the treatment of Brown syndrome despite the high postoperative incidence of superior oblique palsy.2,7 More recently, a lengthening procedure for the superior oblique tendon using a silicone band has been popularized and has led to a remarkable advance in the treatment of Brown syndrome.8,9
We performed a small amount of recession of the ipsilateral inferior rectus muscle instead of taking a direct approach to the superior oblique tendon. Although we were apprehensive that this surgical act might be carried out on an irrelevant "messenger" while the "message" itself was not necessarily addressed our primary surgical aims were to correct hypotropia in the primary position, improve elevation, and, thereby, relieve the troublesome diplopia while looking up, as opposed to the complete reversal of this complicated pathology. We expected, therefore, that the inferior rectus recession could also work. Fortunately, this was the case and the patient needed no further surgery. It seems highly probable that there was some degree of contracture of the inferior rectus due to the chronically hypodeviated position of the involved eye. We guess that the contracture must have been relieved by the inferior rectus recession, which, in consequence, played a significant role in the correction of the overall state of the ocular motor abnormality.
Brown syndrome can be simply defined as an inability of elevation in adduction. This syndrome describes the effect, but not the cause. Actually, anything that limits this movement can be said to cause Brown syndrome. It would be prudent for the treatment to be applied on an individual basis according to the diagnosed etiology, especially in cases of acquired simulation caused by various mechanisms.
In conclusion, surgical procedure to repair medial orbital wall fracture should be considered as a possible cause of acquired simulated Brown syndrome. Various causes and complex mechanisms may be involved in the development of this syndrome. Careful assessment is absolutely essential for proper treatment and successful outcome.
Figures and Tables
Fig. 1
Preoperative photographs of eye movements demonstrate the limited elevation of the left eye in adduction and primary position with normal elevation in abduction. The limitation of elevation is greatest in adduction.

References
1. Brown HW. Allen JH, editor. Congenital structural anomalies of the muscle. Symposium on strabismus, Trans New Orleans Acad Ophthalmol. 1950. St Louis: CV Mosby;205–236.
2. Wilson ME, Eutis HS Jr, Parks MM. Brown's syndrome. Surv Ophthalmol. 1989. 34:153–172.
3. Erie JC. Acquired Brown's syndrome after peribulbar anesthesia. Am J Ophthalmol. 1990. 109:349–350.
4. Zipf RF, Trokel SL. Simulated superior oblique tendon sheath syndrome following orbital floor fracture. Am J Ophthalmol. 1973. 75:700–705.
5. Lauer SA, Sauer H, Pak SM. Brown's syndrome diagnosed following repair of an orbital roof fracture: a case report. J Craniomaxillofac Trauma. 1998. 4:20–22.
6. Baker RS, Conklin JD. Acquired Brown's syndrome from blunt orbital trauma. J Pediatr Ophthalmol Strabismus. 1987. 24:17–21.
7. Crawford JS. Surgical treatment of true Brown's syndrome. Am J Ophthalmol. 1976. 81:289–295.
8. Wright KW. Superior oblique silicone expander for Brown syndrome and superior oblique overaction. J Pediatr Ophthalmol Strabismus. 1991. 28:101–107.
9. Stager DR Jr, Parks MM, Stager DR Sr. Long-term results of silicone expander for moderate and severe Brown syndrome (Brown syndrome "plus"). J AAPOS. 1999. 3:328–332.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download