Abstract
Purpose
To evaluate the effectiveness of Ahmed valve implantation for refractory glaucoma following pars plana vitrectomy.
Methods
Seventeen eyes of 15 patients suffering from secondary glaucoma following pars plana vitrectomy underwent Ahmed valve implantation. All the eyes were in critical condition, and intraocular pressure could not be controlled with anti-glaucoma medications. Success was characterized by an intraocular pressure less than 22 mmHg and greater than 6 mmHg, regardless of anti-glaucoma medication usage.
Results
The total success rate was 83.4% at 6 months and 76.4% at the final visit. The reduction in intraocular pressure and the number of medications used postoperatively were both statistically and clinically significant (p<0.005). Postoperative complications included: transiently increased intraocular pressure, transient hyphema, early postoperative hypotony, choroidal detachment, malposition of the valve tip, and phthisis bulbus.
In the early 1970s, retinal surgery was dramatically advanced when Machemer introduced closed system vitrectomy.1,2 Indications of vitrectomy include: proliferative diabetic retinopathy, retinal detachment, uveitis, endophthalmitis, vitreous hemorrhage, vitreous opacity, ocular perforation, macular disease, and complication of anterior segment operation. As surgical techniques such as intraocular photocoagulation, intraocular gas tamponade and intraocular silicon oil infusion have developed, the indications of vitrectomy have been expanded.3-5
Possible postoperative complications of vitrectomy include: lens opacity, retinal detachment, vitreous hemorrhage, iris neovascularization, and glaucoma.5,6 Despite these complications, glaucoma device implantation is preferred when medications cannot control intraocular pressure (IOP).
Molteno, Baerveldt, Krupin-Denver, Joseph, and Ahmed glaucoma valves have been used as glaucoma devices. Specifically, the Ahmed valve is easy to insert, has a wide filtration area, and prevents low intraocular pressure by functioning only when the IOP is over 8 mmHg.7,8
Several studies have demonstrated that Ahmed valve implantation has a high success rate in IOP control and a low complication rate.9-11 However, these results were not found in all cases of glaucoma following pars plana vitrectomy. This study aimed to evaluate the results and complications of Ahmed valve implantation in refractory glaucoma patients following vitrectomy.
In this study, we analyzed the medical records of patients at the Chosun University Hospital Ophthalmology Department from February 2002 to January 2004. Seventeen eyes of 15 patients suffering from secondary glaucoma following pars plana vitrectomy were treated with Ahmed valve implantation. IOP could not be controlled with anti-glaucoma agents for at least two weeks of treatment. Nine male and six female patients were included in this study. The mean patient age was 47.4 years and the average follow-up period was 14.9 months (Table 1). Reasons for performing vitrectomy included: diabetic vitreous hemorrhage, tractional retinal detachment due to diabetic retinopathy, vitreous opacities due to Behcet's disease, rhegmatogenous retinal detachment, and vitreous hemorrhage due to central retinal vein occlusion (Table 2).
Under retrobulbar anesthesia, a fornix-based conjunctival Tenon's capsule flap was made in either the superior nasal or superior temporal quadrant to expose the scleral bed. A sponge soaked with 0.04% mitomycin C was placed under the dissected flap of the Tenon's capsule for five minutes. The space between the conjunctiva and the episclera was thoroughly irrigated with balanced salt solution. The external plate was tucked posteriorly into the sub-Tenon's space and sutured to the sclera with 8-0 prolene with the anterior border 10 mm posterior to the limbus. We made a limbal-based scleral flap to avoid tube erosion and then cut the tube bevel-up to permit its extension 2 to 3 mm into the anterior chamber. We entered the anterior chamber through the limbal area with a 23-gauge needle parallel to the iris plane. The tube was inserted into the anterior chamber via the needle track and then sutured with 10-0 nylon. After closing the scleral flap, the conjunctiva was sutured back to its original position using vicryl sutures. Subconjunctival steroids and antibiotics were injected into a quadrant away from the surgical site. After the operation, levofloxacin and 1% prednisolone ophthalmic solutions were applied.
Intraocular pressure, which is critical to the success of the operation, was checked at each follow-up and compared to the patient's IOP from their last visit. Preoperative IOP was measured on the day before the operation.
The success of the operation was determined based on the IOP of the patient's final follow-up visit. The operation was considered successful if the IOP at the final visit was maintained between 6 and 21 mmHg, regardless of anti-glaucoma medication usage.
The operation was considered to be a failure if the IOP was over 22 mmHg, when an additional operation or Ahmed valve removal was necessary, or if serious complications such as phthisis buibi developed. The variations in IOP and the number of anti-glaucoma agents used were analyzed using a paired Student's t-test.
Ahmed valve implantation was performed a mean of 240.8 days (range, 31-551 days) following pars plana vitrectomy. The IOPs of all of the patients in the study had been continuously increasing, and the average IOP before the operation was 47.5 mmHg (range, 25-66 mmHg). The average IOP steadily increased following the operation: 11.1 mmHg (range, 4-18 mmHg) at one day, 12.1 mmHg(range, 5-35 mmHg) at seven days, 18.8 mmHg (range, 7-40 mmHg) at one month, 14.4 mmHg (range, 5-35 mmHg) at three months, and 13.8 mmHg (range, 3-22 mmHg) at six months postoperatively. Overall, postoperative IOP was significantly decreased compared to preoperative IOP (p<0.005) (Fig. 1).
The number of anti-glaucoma agents used steadily decreased after the operation: 1.76 before the operation, 0.12 at one day after, 0.24 at seven days, 0.53 at one month, 0.29 at three months, and 0.35 at six months postoperatively. These values were statistically significant compared to the preoperative values (p<0.005) (Fig. 2).
Regarding postoperative complications, we found transiently increased IOP in seven eyes, postoperative hypotony in two eyes, choroidal detachment in one eye, malposition of valve tip in one eye, and phithisis bulbus in one eye (Table 3).
Anti-glaucoma agents controlled the IOP in all the seven eyes with transiently increased IOP and thus, these patients did not require an additional operation. Five out of six eyes with hyphema did not develop other complications and the hyphema was naturally resolved. However, in the remaining one eye, hyphema was resolved after tissue plasminogen activator was injected into the anterior chamber. One of the two eyes with postoperative hypotony recovered within one week after the operation without treatment, and the chamber shallowing in the other eye was treated by chamber reformation with viscoelastics. Although one eye developed choroidal detachment, it was naturally resolved within one to two weeks following the operation. Because the one eye with valve malposition did not function after the reconstructive operation, the valve was removed and a new Ahmed glaucoma valve was inserted.
Transient or continual IOP increase after pars plana vitrectomy, which is caused by various mechanisms, is a common postoperative complication and requires aggressive medical or surgical treatment.12 Hwang et al.13 reported that early (within 7 days of pars plana vitrectomy) and late postoperative IOP elevation occurred in 40.3% and 40.7% of patients, respectively. According to Dennis et al.14, acute (within 48 hours of surgery) postoperative IOP elevation occurred in 61.3% of patients and late postoperative glaucoma occurred in 26.0% of patients. When treatment with medication proves ineffective, in controlling IOP, glaucoma implantation is preferable because of the low success rate of traditional trabeculectomy.
Various glaucoma implant devices have been developed and used since the Molteno glaucoma implant was introduced in 1969.15 All drainage devices have the same basic design, which consists of a silicone tube that extends from the anterior chamber to a plate beneath conjunctiva and the Tenon's capsule. A fibrous capsule forms a filtering bleb around the plate.16
The Ahmed glaucoma valve, the device used in this study, directs aqueous flow through the silicone tube and between two thin silicone elastomer membranes which allow one-way regulation of the flow, with the goal of keeping the IOP between 8 and 10 mmHg in the early postoperative period.17
Some clinical results of Ahmed valve treatment in refractory glaucoma patients from previous studies are as follows. Kim et al. reported that the accumulated success rate was 85% at 12 months after the operation. However, they also observed the following postoperative complications: hypotony (6.7%), transiently increased intraocular pressure (6.7%), hyphema (6.7%), valve clogging (6.7.%), and inflammatory membrane in the anterior chamber (3.3%) on the day after the operation.18 Kim et al. reported that the success rate at one year after the operation was 83.1%, and 64.5% at two years after the operation. According to their report, the number of anti-glaucoma agents used after the operation decreased, and postoperative complications included early postoperative hypotony (10.3%), bullous keratopathy (5.2%), and fibrotic membrane (17.2%).11
In this study, the success rate was 83.4% at six months after the operation and 76.4% at the patients' final visits. The number of anti-glaucoma agents used was 1.76 before the operation and 0.29 at the patient's final postoperative visit, which is a similar to the results of previous studies.
In our study, postoperative complications included: transiently increased intraocular pressure in seven eyes, hyphema in three eyes, postoperative hypotony in two eyes, choroidal detachment in one eye, malposition of the valve tip in one eye, and phthisis bulbus in one eye.
The hypertensive phase following glaucoma implantation was first reported by Molteno.19 During the hypertensive phase, which can occur at four to six weeks after the operation, intraocular pressure increases due to the decrease in the transmission ability of the filtering bleb, which had become thick by inflammatory reaction and fibrosis around the body of the glaucoma implant.20 In this study, the postoperative IOP was increased to 18.8 mmHg, at 1 month. This increase was statistically higher than 13.8 mmHg, at 6 month. The postoperative IOP was over 22 mmHg in seven of 17 eyes (41.1%). This result is similar to the report of 50% by Heo et al.8 but is lower than the report of 82% by Ayyala et al.20
During the hypertensive phase, a layer of fibrous tissue appears in the deepest layers of the bleb, and the bleb becomes distended with aqueous humor. During the first 1 to 4 weeks of this stage, congestion and inflammation of the bleb wall occurs and IOP increases to 30 to 50 mmHg. The bleb wall congestion and inflammation gradually subside and the bleb becomes well-circumscribed and thick-walled with IOP stabilization.6,20
According to Ayyala et al., the hypertensive phase occurs inversely proportional to the body size of the valve, and IOP can be controlled at 70% by needling with an anti-glaucoma agent with 5-FU.20 Heo et al. reported that IOP can be controlled at 80% by needling with 5-FU.8 However, in this study, we found that anti-glaucoma agents alone could control the intraocular pressure in seven eyes with an intraocular pressure over 22 mmHg.
In conclusion, Ahmed glaucoma valve implantation in patients with refractory glaucoma following pars plana vitrectomy effectively decreases intraocular pressure and has a low incidence of postoperative complications. Thus, this procedure can be considered as primary treatment for refractory glaucoma following vitrectomy.
Figures and Tables
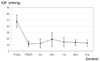 | Fig. 1Mean Intraocular Pressure before and after ahmed valve implantation following pars plana vitrectomy. |
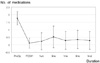 | Fig. 2Mean number of anti-glaucoma medications before and after ahmed valve implantation following pars plana vitrectomy. |
References
1. Machemer R, Parel JM, Buettner H. A new concept for viterous surgery. Instrumentation. Am J Ophthalmol. 1972. 73:1–7.
2. Machemer R, Buettner H, Nerton EWD. Vitrectomy ; a pars plana approach. Trans Am Acad Ophthalmol Otolaryngol. 1971. 75:813–820.
3. Coleman DJ, Lucas BC, Rondeau MJ, et al. Management of intraocular foreign bodies. Ophthalmology. 1987. 94:1647–1653.
4. Kim SD, Kim SM. Clinical Evaluation of Surgical Treatments for Displaced lens : Transfixation and pars plana Technique. J Korean Ophthalmol Soc. 1990. 31:27–33.
5. Kim HK, Chung HY, Chung YT. The clinical evaluation of pars plana vitrectomy in various ocular disease. J Korean Ophthalmol Soc. 1997. 38:2020–2027.
6. Jung BY, Shin JP, Kim SY. Surgical outcome and postoperative complications of vitrectomy for diabetic retinopathy. J Korean Ophthalmol Soc. 2002. 43:1635–1643.
7. Coleman Al, Hill R, Wilson MR. Initial clinical experience with the Ahmed glaucoma valve implant. Am J Ophthalmol. 1995. 120:23–31.
8. Huh KC, Kee CW. A clinical analysis of the Ahmed glaucoma valve implant with or without partial ligation of silicone tube. J Korean Ophthalmol Soc. 2000. 41:2611–2617.
9. Krupin T, Podos SM, Becker B. Valve implants in filtering surgery. Am J Ophthalmol. 1976. 81:232–235.
10. Joseph NH, Sherwood MB, Trantas G, et al. A one-piece drainage system for glaucoma surgery. Trans Ophthalmol Soc UK. 1986. 105:657–664.
11. Lee JH, Kim SS, Hong YJ. A clinical study of the Ahmed valve implant in refractory glaucoma. J Korean Ophthalmol Soc. 2001. 42:1003–1010.
12. Detru-Morel M. Glaucoma secondary to surgery of the posterior eye segment. Bull Soc belge Ophthalmol. 2003. 288:65–74.
13. Hwang JJ, Kim YY, Huk K. Risk factors of intraocular pressure elevation after pars plana vitrectomy. J Korean Ophthalmol Soc. 2000. 41:945–950.
14. Dennis PH, Hilel L, Fred HL, et al. Mechanisms of intraocular pressure elevation after pars plana vitrectomy. Ophthalmology. 1989. 96:1357–1362.
15. Molteno ACB. New implant for drainage in glaucoma : Clinical trial. Br J Ophthalmol. 1969. 53:606–615.
16. Coleman AL, Hill R, Wilson MR, et al. Initial clinical experience with the Ahmed glaucoma valve implant. Am J Ophthalmol. 1995. 120:23–31.
17. Kook MS, Jeon SK, Kim MJ, Yoon YH. Combined pars plana vitrectomy and Ahmed implantation for refractory glaucoma. J Korean Ophthalmol Soc. 1998. 39:559–565.
18. Kim SD, Lee JH. Clinical experience with the Ahmed glaucoma valve implant. J Korean Ophthalmol Soc. 1999. 40:1067–1077.
19. Minckler DS, Heuer KD, Hasty B. Clinical experience with the single-plate Molteno implant in complicated glaucomas. Ophthalmology. 1988. 95:1181–1188.
20. Ayyala RS, Zurakowski D, Smith JA, Monshizadeh R. A Clinical study of the Ahmed glaucoma valve implant in advanced glaucoma. Ophthalmology. 1998. 105:1968–1976.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download