Abstract
Purpose
There is currently no treatment proven effective for central retinal vein occlusion (CRVO). Radial optic neurotomy (RON) has recently surfaced as a new treatment for the disorder, however, and we compare here the visual acuity (VA) and arteriovenous transit time (AVTT) following RON and panretinal photocoagulation (PRP).
Methods
We conducted a retrospective, uncontrolled study of 27 patients. Of 27 eyes diagnosed with CRVO, 16 were treated with panretinal photocoagulation (PRP) and 11 with RON. VA and fluorescein angiography were used to monitor the evolution of CRVO, and for follow-up.
Results
All patients underwent PRP or RON with no major complications. The difference between pre- and post-operative VA was not statistically significant for either group (p=0.092 on PRP; p=.0081 on RON). The change in AVTT was also not statistically significant for either group (p= 0.024 on PRP; p=0.027 on RON). Ultimately, we found no statistically-significant difference in comparing VA and AVTT for the two groups (p=0.074 on VA; p=0.510 on AVTT)
Central retinal vein occlusion (CRVO) is a common retinal vascular disorder with no known effective treatment.1-2 According to the Central Vein Occlusion Study, final visual acuity (VA) depends on a patient's initial VA, with VA stabilizing in 65% of patients with an initial VA of 20/40 or better and worsening or remaining unchanged in 85% of patients with an initial VA of 20/200 or worse. In patients with intermediate VA (20/25-20/200), 44% generally show VA stabilization, while 37% show VA deterioration.1 While there is no known effective treatment for CRVO, various treatments have been or are currently being tested.3-5 Recently, Opremcak et al. reported that surgical decompression of the central retinal vein by radial incision of part of the lamina cribrosa, in 11 eyes diagnosed with CRVO, led to VA improvement by five to eight lines on the standard vision test.6 Yet only a few cases of such improvements have so far been reported, and the efficacy of radial optic neurotomy (RON) remains in doubt. Here we compare RON and panretinal photocoagulation (PRP) in terms of VA and arteriovenous transit time (AVTT) in eyes with CRVO.
A retrospective, uncontrolled, interventional study was performed on 27 eyes from 27 patients diagnosed with CRVO. Of these, 16 were treated with PRP and 11 with RON.
On their first visit, all patients were examined for VA, intraocular pressure, existence of neovascularization, and relative afferent pupillary defect (RAPD). Fundus examination, fundus photography, and fluorescein angiography were performed for all patients, and visual field examination was also included for three of the 11 patients treated with RON.
All 16 eyes treated with PRP were diagnosed with nonperfused CRVO, reflecting the decision to use PRP in cases lacking follow up but for which neovascularization had not yet developed. PRP was always performed within one week of the diagnosis of CRVO, at an interval of at least 4 days. The treatment was repeated at least three times on each eye, and disease progression was monitored regularly.
Of 11 patients who underwent RON, eight had nonperfused CRVO, two had perfused CRVO, and one was indeterminate. Fundus examination was performed prior to the operation, and the incision site was chosen on the nasal side of the optic disc so as to minimize damage to the papillomacular nerve fiber bundle. All operations were performed by a single surgeon using the following procedure. With patients under general anesthesia, three-port pars plana vitrectomy (PPV) and mild endolaser (400-881 coagulates with 0.2-second duration of 200 mW in a scatter pattern within the peripheral retina, avoiding the retinal hemorrhage) were performed. The infusion bottle was then raised in order to increase intraocular pressure to approximately 25 mmHg and thereby minimize hemorrhage. The tip of the microvitreoretinal blade (MVR blade, 20 Ga.) was placed at the edge of the optic disc and directed toward the pre-operativelyselected incision site. The blade was drawn posteriorly into the optic nerve so that equal portions of the cribriform plate and adjacent sclera were incised The incisied into the optic nerve was made deep incised so that the MVR blade intruded just beyond the widest portion of the diamond-shaped tip. After that the infusion bottle was lowered to decrease the intraocular pressure. The degree of hemorrhage was checked and the scleral openings were to sutured to mark completion of the operation.
VA and fundus examinations were performed at 1 day, 1 and 2 weeks, and 1, 2, 4, 6, and 12 months after the operation, as well as on patients' last visits. Fluorescein angiography was performed in two cases for which the patient's last visit was at 2 months post-PRP or post-RON. Postoperative visual field examination was possible in three cases. In all cases, intraocular pressure, presence of neovascularization, RAPD, and associated systemic diseases were examined.
The average age of patients was 55 years (range, 23-77 years) for the PRP group and 52 years (range, 23-69 years) for the RON group. Of the 16 PRP patients, five were male and 11 were female. The RON group was composed of 11 males and six females.
The mean interval from onset of symptoms to time of operation was 2.25 months (range, 0.5-6 months) for the PRP group and 2.13 months (range, 0.5-5 months) for the RON group. The post-operative follow-up period for the PRP group ranged from 4 to 24 months (mean follow-up period, 19 months), while that for the RON group ranged from 18 to 30 months (mean, 21 months).
Pre-PRP VA ranged from LP to 20/125 (mean, 20/250; median, 20/200), while pre-RON VA ranged from HM to 20/80 (mean, 20/200; median, 20/200). Pre-PRP AVTT ranged from 19 to 42 (mean, 29.06; median, 28.5), and pre-RON VA ranged from 13 to 28 (mean, 21.91; median, 23).
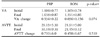
Of the 16 PRP patients, diabetes mellitus was present in four, hypertension in four, and chronic pulmonary obstructive disease in one. For the RON group, diabetes mellitus was present in one patient and hypertension in two. RAPD was found in ten of the 16 eyes that underwent PRP and in five eyes that underwent RON, four with nonperfused CRVO and one with perfused CRVO. RAPD was also found in the one indeterminate eye. Neovascular glaucoma (NVG) developed in two eyes that had undergone PRP but not in any eyes from the RON group. Patients' demographic data are listed in Table 1. Hemorrhaging at the incision site occurred in all patients during the RON procedure, but every case was controlled by increasing the intraocular pressure and was prevented from becoming a significant complication. Slight vitreous hemorrhage was observed during the early post-operative period in one RON patient, but this cleared spontaneously within 2 weeks. Fundus examinations showed reduction of congestion and of retinal hemorrhage in two eyes that had undergone PRP and in five eyes that had undergone RON. The degree and time taken for such improvement varied by patient.
At 6 months after PRP, VA ranged from HM to 20/80 (mean, 20/250; median, 20/500). VA for the same time after RON ranged from LP to 20/50 (mean, 20/200; median, 20/400). Of the 16 PRP eyes, two showed improvement of more than two lines of vision, ten showed no change, and four showed deterioration of VA. Of the 11 RON eyes, three showed improvement, six showed no change, and two showed deterioration of VA. The VA change (difference between pre- and post-operative VA at 6 months) was not statistically significant for either group (p = 0.092, Spearman rank correlation value, r=0.435 for the PRP group p=0.081, r=0.806 for the RON group; Fig. 1).
Fluorescein angiography showed the AVTT change (difference between pre- and post-operative AVTT at 6 months) to be 0.450±6.67 seconds (mean, 29.06; median, 29.43 seconds) for the RON group and 0.710±6.0 seconds (mean, 21.90; median, 21.45) for the PRP group. The AVTT change was not statistically significant for either group (p= 0.024, r=0.786 on PRP group p=0.027, r=0.694 on RON group). Improvement in AVTT was seen in one eye from the PRP group and in three eyes from the RON group. For all other eyes, the AVTT either did not change or worsened (Fig. 2).
Neither VA change (p=0.074) nor AVTT change (p=0.510) showed a significant difference between the PRP and RON groups (Table 2). But, VA change was statistically related to AVTT change within each group (p=0.005, r=-0.656 on PRP group p=0.001, r=-0.656 on RON group). There seemed to be a tendency to achieve better VA when AVTT decreased during follow-up (Fig. 3). Two of the three eyes showing improved VA and AVTT had perfused CRVO and were from the RON group. In the RON group, segmental temporal visual field loss was seen in one eye, patient 7 (Fig. 4). Three patients (27.2%) developed a cataract during the follow-up period.
CRVO is, comparatively, a prevalent retinal vascular disorder. Disease onset generally occurs in patients in their early 60's and is accompanied by retinal hemorrhage, cotton-wool spot, retinal edema, capillary nonperfusion, neovascularization, and vitreous hemorrhage.1,7 Although non-perfused vein occlusion has a self-limiting prognosis, it causes severe loss in VA due to the chronic macular edema and macular ischemia that accompany it. Non-perfused vein occlusion is the most difficult form of the disease from which to recover. Moreover, there is a high risk of NVG due to neovascularization in cases of non-perfused vein occlusion.7-8 PRP is generally used to prevent NVG development, as is grid-pattern photocoagulation to reduce macular edema.1,7-9
Various treatments have been tested, but none has yet proven effective. Vasco-Posada and Opremcak et al. operated from the belief that the bottleneck-like configuration of the scleral outlet and the consequent neurovascular compression cause central retinal vein occlusion.10 In an attempt to relieve the neurovascular compression, Vasco-Posada approached the eye-ball posteriorly and incised portions of the scleral ring, scleral outlet, and dural sheath of the optic nerve, as all of these anatomical structures could impede circulation of retinal vessels. In contrast, Opremcak et al. achieved neurovascular decompression by radially incising the lamina cribrosa and its surrounding scleral outlet after performing a standard three-port vitrectomy. This group reported improvement in VA by more than five lines of vision in eight of 11 eyes on which they operated.6
Marcin et al. reported that papilledema, axonal nerve fiber loss, and gliosis developed in 14 normal swine eyes three weeks after RON was performed and they concluded that RON is a traumatic procedure whose efficacy and safety have yet to be shown.11 Hayreh et al. reported that surgical decompression of the optic disc has no effect on central retinal vein occlusion and rather presents several risks of harm.12 First, the site of occlusion is not necessarily at the lamina cribrosa but instead, varies depending on the type of CRVO. In perfused CRVO, the site of occlusion is actually in the optic nerve, at a variable distance posterior to the lamina cribrosa. Its collateral circulation thus remains unhindered, and perfused CRVO has a better prognosis than does nonperfused CRVO in which there is complete occlusion of CRV behind the lamina cribrosa. Using eyes blinded by CRVO with associated neovascular glaucoma, Opremcak et al. concluded that occlusion occurs pathohistologically at the lamina cribrosa.6 But the overall prevalence of NVG in CRVO is less than 10%, as NVG occurs in only 45% of cases of ischemic CRVO and does not occur at all in cases of non-ischemic CRVO unless there is associated DR or ischemia. Hence, the eye samples used by Opremcak et al. do not represent the majority of CRVO eyes, and the conclusion made from that study is not universal. The second risk of surgically decompressing the optic disc arises from the anatomic proximity of the central retinal vein to the central retinal artery and to the surrounding common fibrous tissue capsule. The lamina cribrosa is a compact structure that consists of non-elastic collagen tissues. Radial incision of a part of this structure cannot, in fact, result in decompression of the central retinal vein, although such incision does introduce the risk of cutting or damaging the central retinal artery. Surgical decompression is also risky because, by the time symptoms appear, the retinal vein is completely occluded by thrombus and immediately undergoes organization. For this reason and those outlined above, Hayreh et al. argue that the RON procedure is both anatomically and pathologically inappropriate. Likewise, 25 US clinical facilities that performed optic nerve decompression surgery for non-arteritic anterior ischemic optic neuropathy reported no difference in VA between the treatment and non-treatment groups after six months of observation. These centers concluded that the RON procedure is ineffective and could even be harmful.12
There are yet other complications and risk factors associated with RON that makethis procedure unwarranted. First, the circle of Zinn and Haller is known to supply blood to the optic nerve, and accidental incision of this structure may cause ischemia of the optic disc.13 Opremcak et al. noted in their report that they had not considered the circular artery of Zinn and Haller and reported that the effect of cutting this structure could not be determined.6 It is also possible for severance of the optic nerve by RON, which would result in visual field defects of the corresponding areas.14-15 Third, there is a risk of serous retinal detachment in the RON operation area.16 Moreover, RON poses the risk of postoperational development of chorioretinal anastomosis, although it has been reported that development of chorioretinal anastomosis has no significant effect on improvement of VA.17-18 A recent report was made of a case in which CRVO developed in an eye previously operated on by RON, a fifth risk of the RON procedure.19 And finally, as many as 43% of RON patients have been reported to develop cataracts during the post-operational follow-up period.20
Our findings in this study suggested several trends. First, VA was correlated with AVTT. Second, two of the three eyes showing improved VA and AVTT in the RON group had been diagnosed with perfusion-type CRVO. Third, there was no statistical significance in the difference of VA and AVTT between the two groups. We assumed that the results we observed were caused by natural history, mechanical alleviation of retinal traction by posterior hyaloid peeling, or PPV. Ko et al. reported improvement in VA, reduction in AVTT, and improvement in macular edema as seen by optical coherent tomography.14 Glacet-Bernald et al. reported that VA depends on the blood flow consistently available.21 According to a study of the activity of carbon anhydrase, which accumulates in and around Muller cells, exchange of metabolites between the vitreous cavity and retina was facilitated, and macular edema was reduced after PPV was performed.22 Both of these may have been due to a beneficial effect of PPV by which the vitreous cavity fluid acted as a carrier of oxygen from unaffected retinal or ciliary body tissue to the ischemic retina.13
Surgical decompression of CRVO via RON is both anatomically and pathophysiologically unsupported and may indeed be an ineffective procedure. The present study is a retrospective, randomized clinical study including only a limited number of patients. Nevertheless, vitreoretinal surgeons performing RON cannot ignore this controversy, and further investigation regarding the effectiveness and safety of this procedure should be made.
Figures and Tables
Fig. 1
The correlation between the preoperative and postoperative visual acuity in each group: A (PRP group, r=.435, p=.092*), B (RON group, r=.806, p=.081*). *Statistics by Spearman rank correlation analysis.

Fig. 2
The correlation between the preoperative and postoperative arteriovenous transit time in each group: A (PRP group, r=.786, p=.024*), B (RON group, r=.694, p=.027*). *Statistics by Spearman rank correlation analysis.

Fig. 3
In each group, visual acuity was negatively correlated with the arterioveouns transit time. A (PRP group, r=-0.656, p=.005*). B (RON group. r=-0.869, p=.001*). *Statistics by Spearman rank correlation analysis.

Fig. 4
The preoperative (A) and postoperative (B) visual fields of the patient 7. The wedge-shaped defect and this finding was correlated with the incision site in the radial optic neurotomy

Table 1
Patient characteristics

M: male, F: female, DM: diabetes mellitus, HBP: high blood pressure, NVG: neovascular glaucoma, NVI: neovascularization of the iris, RAPD: relative afferent pupillary defect, P: perfused, N: nonperfused, I: indeterminate, Preop: preoperative, Postop: postoperative, CF: couning fingers, HM: hand motions, LP: light perception.
References
1. The Central Vein Occlusion Group. Natural history and clinical management of central retinal vein occlusion. Arch Ophthalmol. 1997. 115:486–491.
2. Oh DR, Park YH, Hahn DH. Visual outcome of central retinal vein occlusion. J Korean Ophthalmol Soc. 1998. 39:1468–1477.
3. Weiss JN, Bynoe LA. Injection of tissue plasminogen activator into a branch retinal vein in eyes with central retinal vein occlusion. Ophthalmology. 2001. 108:2249–2257.
4. Elman MJ. Thrombolytic therapy for central retinal vein occlusion: results of a pilot study. Trans Am Ophthalmol Soc. 1996. 94:471–504.
5. Mcallister IL, Constable IJ. Laser-induced chorioretinal venous anastomosis for treatment of nonischemic central retinal vein occlsion. Arch Ophthalmol. 1995. 113:456–462.
6. Opremcak ME, Bruce RA, Lomeo MD. Radial optic neurotomy for central retinal vein occlusion: a retrospective pilot study of 11 consecutive cases. Retina. 2001. 21:408–415.
7. The Central Vein Occlusion Group. Baseline and early natural history report: The Central Vein Occlusion Study. Arch Ophthalmol. 1993. 111:1087–1095.
8. Hayreh SS. Management of central retinal vein occlusion. Ophthalmologica. 2003. 217:167–188.
9. The Central Vein Occlusion Study Group. M Report. Evuluation of grid pattern photocoagulation for macular edema in central retinal vein occlusion. Ophthalmology. 1995. 102:1425–1433.
10. Vasco-Posada J. Modification of the circulation in the posterior pole of the eye. Ann Ophthalmol. 1972. 4:48–59.
11. Cazjka MP, Cummings TJ, McCuen BW. Radial Optic Neurotomy in the porcine eye without retinal vein occlusion. Arch Ophthalmol. 2004. 122:1185–1189.
12. Ischemic Optic. Optic Nerve decompression surgery for nonarteritic anterior ischemic optic neuropathy(NAION) is not effective and may be harmful. JAMA. 1995. 272:625–632.
13. Hayreh SS. Radial Optic Neurotomy for central retinal vein occlusion. Retina. 2002. 22:374–377.
14. Ko BY, Kim JW. Follow up results after radial optic neurotomy for central retinal vein occlusion. J Korean Ophthalmol Soc. 2003. 44:2784–2795.
15. Williamson TH, Poon W, Whitefield L, et al. A pilot study of pars plana vitrectomy, intraocular gas, and radial neurotomy in ischaemic central retinal vein occlusion. Br J Ophthalmol. 2003. 87:1126–1129.
16. Michael AS, Uday RD, Cristian BG. Peripapillary retinal detachment after radial optic neurotomy for central retinal vein occlusion. Retina. 2003. 23:580–583.
17. Jang KC, Cho NC, Ahn M, et al. The Efficacy of radial optic neurotomy for central retinal vein occlusion. J Korean Ophthalmol Soc. 2003. 44:1797–1805.
18. Weizer JS, Stinnett SS, Fekrat S. Radial optic neurotomy as treatment for central retinal vein occlusion. Am J Ophthalmol. 2003. 136:814–819.
19. Shuichi Y, Yoko T, Eiju S, et al. Central retinal artery occlusion after radial optic neurotomy in a patient with central retinal vein occlusion. Am J Ophthalmol. 2005. 139:206–207.
20. Jose GA, Anna B, Vicente MC, et al. Chorioretinal anastomosis after radial optic neurotomy for central retinal vein occlusion. Arch Ophthalmol. 2003. 121:1385–1391.
21. Glacet-Bernard A, Coscas G, Chabanel A, et al. Prognostic factor for retinal vein occlusion: prospective study of 175 cases. Ophthalmology. 1996. 103:551–560.
22. Musser GL, Rosen S. Localiazation of carbonic anhydrase activity in the vertebrate retina. Exp Eye Res. 1973. 15:105–119.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download