Abstract
Purpose
To investigate the factors that affect final vision following photodynamic therapy (PDT) for idiopathic subfoveal choroidal neovascularization (CNV).
Methods
A retrospective review of 16 patients whose eyes were diagnosed as idiopathic subfoveal CNV and were followed up for a minimum of 9 months. Statistical analysis was performed to investigate relationships between sex, age, size of the lesion, and initial vision compared to final vision.
Results
In the PDT group (10 eyes), the mean age of the patients was 34 years, mean size of the lesion was 1300 µm, mean initial vision was 20/60, and 7 of the 10 patients (70%) showed more than a two-line improvement in vision. Factors affecting final vision were sex (p=0.049), initial vision (p=0.0455), and size of the lesion (p=0.006). In the observation group (6 eyes), the mean age of the patients was 39 years, mean size of the lesion was 575 µm, mean initial vision was 20/32, and 5 of the 6 patients (83%) showed more than a two-line improvement in vision.
Conclusions
The prognosis of idiopathic CNV was favorable as was reported in other studies. In the PDT group, statistically significant factors affecting final vision were initial vision, size of the lesion, and sex. However, since the number of patients sampled was insufficient and the average size of the lesions in the female patients was smaller, the size of the lesion seems to be the most important factor.
Idiopathic choroidal neovascularization (CNV) is a CNV that develops at a young age, which is not related to any other ophthalmologic disorders.1 The most common cause of CNV in patients under the age of 50 is high myopia, and other causes include angioid streak and inflammatory diseases.2
Cases of parafoveal or extrafoveal CNV may be treated with laser photocoagulation, but cases of subfoveal CNV may develop a central scotoma and show high recurrence rates following laser photocoagulation.3,4 Other treatments for subfoveal CNV such as radiotherapy, submacular surgery, macular translocation, transpupillary thermotherapy have been attempted, but these treatments seem to be limited due to the high risk of complications and vision damage.5-8
Recently, verteporfin in photodynamic therapy (PDT) has been shown to induce degradation of the neovascularization and is effective in the treatment of age-related macular degeneration (AMD) or myopic CNV.9,10
Prognosis of idiopathic CNV has been shown to be good when proper followed-ups are administered. In addition, it has been reported that more cases degenerate spontaneously compared to other diseases.11
Therefore, we investigated the outcomes of a PDT group and an observation group of idiopathic subfoveal CNV, and examined the factors that affect final visual acuity in PDT group.
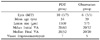
Sixteen patients whose eyes were diagnosed as idiopathic subfoveal CNV and were followed up for a minimum of 9 months participated in the study (Table 1). PDT was performed in cases of a greater than two-line decline compared with initial vision and an increase in size of the lesion compared with the first visit following a minimum of a 3-month follow-up period.12 The PDT group consisted of 10 patients of which 3 were male and 7 were female, with age ranging from 26 to 50 years and an average of 34 years. The observation group consisted of 6 patients of which 3 were male and 3 were female, with age ranging from 24 to 50 years and an average of 39 years. The follow-up period of the PDT group ranged from 9 to 49 months (mean 25.6 months) and the observation group ranged from 9 to 24 months (mean 18 months).
Corrected vision and size of CNV for the 16 patients were investigated retrospectively by reviewing medical records. Statistical analysis was performed to investigate the relationship between age, sex, size of the lesion and initial vision compared to final vision. To investigate these relationships the T-test and, Chi-square test were performed using SPSS 10.0 software.
Initial and final vision was measured using the Snellen chart. The largest linear dimension of the lesion was measured with a transparent millimeter ruler through a funduscopy, and fluorescein funduscopy, and the size of the lesion on the fundus was evaluated by dividing the camera lens ratio (2.5 in 35 degree, 1.8 in 50 degree). The spot size of the laser was determined by adding 1000 µm to the initial size, and 6 mg per surface area of verteporfin was injected with a velocity of 3 ml/min for exactly 10 minutes. An Opal Photoactivator which is a nonthermo-diode laser with a wavelength of 689 nm was used and was irradiated for exactly 15 minutes after the verteporfin injection for 83 seconds, to achieve irradiation of 50 J/cm2.
A diagnosis of idiopathic CNV was made only in the patients under 50 years of age at the date of the initial examination with vision under -6.0 D on refractometry, no history of traumatic choroidal rupture or familial dystrophy, no history of laser therapy, no atrophic choroidal lesion on funduscopy, and no degenerative myopia or peripapillary fundus change found on fluorescein funduscopy.
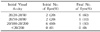
The lesions of all 16 patients were in the subfovea. Mean lesion size for the PDT group was 1300 µm, mean initial vision was 20/60, mean final vision was 20/32, and 7 of the 10 patients (70%) showed more than a two-line improvement in vision.
Mean lesion size for the observation group was 575 µm, mean initial vision was 20/32, mean final vision was 20/20, all patients were 20/20, and 5 of the 6 patients (83%) showed more than a two-line improvement in vision (Table 2).
The PDT group was divided into two groups, with group A consisting of the 7 patients who showed more than a two-line improvement and group B consisting of the 3 patients who did not show improvement and the relationship between age, sex, size of the lesion and the initial vision compared to final vision (two-line improvement) was analyzed.
Age was not predictive of final visual acuity or a significant change in vision (p=0.188). The patients in the PDT group ranged in age from 26 to 50 (mean, 34 years). Five patients were 30 years of age or younger and 5 were older than 30 years of age. There was no significant difference in final visual acuity between patients 30 years of age and younger and those older than 30 years of age.
There was no correlation between visual change greater than two Snellen lines and age (p=0.1079). Patients older than 30 years of age were equally as likely to have more than a two-line improvement (3 of 5), stable (1 of 5), decline (1 of 5) in vision as patients 30 years of age and younger (improvement, 4 of 5; decline, 1 of 5).
There was a significant difference in final visual acuity between male and female patients. Final visual acuity in male patients were good (20/60 or better;1 of 3), intermediate (20/70-20/100; 0 of 3), poor (20/100 or worse ; 2 of 3) compared with female patients (good, 6 of 7; intermediate, 0 of 7; poor, 1 of 7).
There was a correlation between visual change of more than two Snellen lines and sex (p=0.049). Male patients were less likely to have more than a two-line improvement (1 of 3), stable (1 of 1), decline (1 of 1) in vision, compared to female patients (improvement, 6 of 7; stable, 0 of 7; decline, 1 of 7).
In addition, the mean lesion size of the men was 2133.33 µm, while the mean lesion size of the women was 942.86 µm.
In the relation of final visual acuity on a standard of initial visual acuity 20/60, there were correlations to visual change greater than two Snellen lines (p=0.0455, Pearson chi-square test). The 4 patients (40%) that had a initial visual acuity above 20/60 all showed visual change of more than a two-line improvement, but of the 6 patients (60%) that had initial visual acuity of less than 20/60, 3 patients showed an improvement, 1 patient remained stable, and 2 patients showed a decline (Table 3).
There was a statistically significant relationship between the size of CNV and final vision (p=0.006). Seven patients had CNV of 1 disc area or smaller (small lesion), whereas three patients had CNV of greater than 1 disc area (large lesion). None of the lesions were larger than 2 disc areas in size. The mean lesion size for group A (two-line improvement) was 914.29 µm (SD=409.99), and mean lesion size for group B (stable or decline) was 2200.00 µm (SD=700.00).
Size of CNV had correlations to visual change greater than two Snellen lines (p=0.033). Seven patients with CNV of 1 disc area or smaller all showed good final visual acuity of above 20/60, and 3 patients with CNV of greater than 1 disc area all showed poor final visual acuity of 20/200 or worse (Table 4).
Idiopathic CNV is a CNV that develops at a young age, which is not related to any other ophthalmologic disorders.1 Cohen et al reported that the etiology of CNV in patients under the age 50 to be high myopia in 62% of cases, angioid streak in 5%, others such as genetic, traumatic, or inflammatory disorders in 4%, and idiopathic in 17%.2
The results of the study by Cohen et al showed that 67% of the cases of idiopathic CNV were in females, the mean age was 36.7 years and the prevalence of idiopathic CNV in both eyes was 10%.2 In our study, 62.5% of the patients were female, the mean age was 36.7 years, and there were no patients with both eyes affected.
Recently, studies using indocyanine green (ICG), have been reported localized dilatation of choroidal veins and choroidal hyperpermeability around the neovacularization, which suggests a localized choroidal circulation disorder, as the cause of idiopathic CNV.13,14
The natural progress of idiopathic CNV is known to have better outcomes compared to AMD or myopic CNV. Ho et al investigated 19 patients with idiopathic subfoveal CNV for a mean follow up period of 87 months and reported 95% of the patients had stable or improved vision, 21% had final visual acuity above 20/40, 63% above 20/100, and 16% showed a decrease in visual acuity, and the size of CNV was the only variable associated with long-term final visual acuity.11 Ahn et al investigated 14 patients with idiopathic CNV for a mean follow up period of 45 months and reported 57% of the patients had more than a two-line improvement, 36% of the patients remained stable, 7% of the patients experienced a decline and initial visual acuity was significantly correlated with final visual acuity.15 The present study also showed a good prognosis for patients in the observation group with all patients showing final visual acuity of 20/20, and 5 of the 6 patients (83%) had more than a two-line improvement and one patient had initial and final visual acuity of 20/20. Although the number of patient samples was insufficient, prognosis for patients in the observation group seemed to be favorable because of good initial vision and small size of the lesion.
Types of treatment used to treat idiopathic CNV are laser therapy, subretinal surgery and PDT.3,4,16 Laser photocoagulation is performed when central visual acuity decreases due to exudative change of CNV in the juxtafovea or when the patient is in danger of central visual acuity failure.3,4 In a report of the MPS Group, argon laser treatment was performed on 30 patients with idiopathic CNV, and 21 patients (70%) in the treatment group showed vision improvement, a significant curative effect compared to the control group (51%).3 Subretinal surgery has been performed in some cases of CNV in the subfovea and has been reported to have a better outcome than CNV caused by AMD. This is thought to be because the location of idiopathic CNV development is between the retinal pigment epithelial cell (RPE) and neuroretina and the RPE is well preserved.17,18 However, these treatments are limited because they can cause serious retinal damage and an eventually permanent decrease in vision.11
Recently, PDT has been used often and it has been shown to be effective in treating classic CNV of AMD and myopic CNV, and is known to have the least amount of possible complications compared to other types of treatment being performed at the present time.9,10 In this study the mean initial vision of the 10 patients treated with PDT was 20/60 and the mean final vision was 20/32, showing a significant improvement in vision of more than a two-line, 7 of the 10 patients (70%) showed more than a two-line improvement, 1 patient (10%) remained stable, and 2 patients (20%) experienced a decrease. Also, the final visual acuity was above 20/40 in 60% of the patients.
Idiopathic CNV is reported to show characteristics of two types of CNV that proliferate between the sensory retina and retinal pigment epithelium. Idiopathic CNV is not accompanied by massive subretinal hemorrhage or exudate compared to AMD, and shows natural degeneration.19-22 The reason why vision loss is not accompanied with atrophic degeneration is due to the recovery mechanism of RPE which suppresses neovascularization.23 In patients affected by idiopathic CNV at young ages, due to the normal functions of the surrounding retina, the suppressive effect of RPE is greater in the balance of proliferation and suppression. Moreover, RPE proliferates around the neovascularization blocking vessel growth and plays a role in maintaining the blood-retinal barrier which accelerates the degeneration of the neovascularization.24,25 In this study, the mean size of the CNV was 1300 µm in the PDT group, with 7 patients (70%) having a lesion of less than 1 disc area and 3 patients (30%) having a lesion of more than 1 disc area. Final visual acuity in all cases with less than 1 disc area was above 20/60, and final visual acuity in all cases with greater than 1 disc area was under 20/200, showing significant correlations with the final vision (p=0.006). The mean size of the observation group was 575 µm, with all 6 patients having a lesion of less than 1 disc area. Therefore, the smaller the size of the CNV, the better the prognosis for final visual acuity is.
In a recent study using optical coherence tomography (OCT), it was reported that 25% of cases of idiopathic CNV did not grow into the subretinal space, were observed as fusiform type and the idiopathic CNV did not show any changes during an average follow up period 6 months. In 75% of the patients the idiopathic CNV was observed initially as a protruding type in the outpatient department and during an average follow up period of 7 months, 90% changed to fusiform type.13 In the cases of idiopathic CNV, visions seem to be stable or improved because of these patterns.
In this study, the PDT group and the observation group both showed a good prognosis for final visual acuity. Prognosis of idiopathic CNV is relatively good because it occurs in patients at a relatively young age and it is similar to typical CNV which has the best response to PDT.26 Both the PDT group and the observation group, showed significant final vision improvement compared to initial vision. 70% of the PDT group and 83% of the observation group showed more than a two-line improvement.
In conclusion, statistically significant factors affecting final visual acuity (more than a two-line improvement) were initial visual acuity (p=0.0455), size of the lesion (p=0.006), and sex (p=0.049). However, since the number of patients sampled was insufficient and the average size of the lesions in the female patients was smaller, the size of the lesion seems to be the most important factor.
Figures and Tables
References
1. Cleasby GW. Idiopathic focal subretinal neovascularization. Am J Ophthalmol. 1976. 81:590–596.
2. Cohen SY, Laroche A, Leguen Y, et al. Etiology of choroidal neovascularization in young patients. Ophthalmology. 1996. 103:1241–1244.
3. Macular Photocoagulation Study Group. Argon laser photocoagulation for idiopathic neovascularization. Results of a randomized clinical trial. Arch Ophthalmol. 1983. 101:1358–1361.
4. Macular Photocoagulation Study Group. Krypton laser photocoagulation for idiopathic neovascularization. Results of a randomized clinical trial. Arch Ophthalmol. 1990. 108:832–837.
5. Thomas MA, Grand MG, Williams DF, et al. Surgical management of subfoveal choroidal neovascularization. Ophthalmology. 1992. 99:952–968.
6. Fujii GY, Pieramici DJ, Humayun MS, et al. Complication associated with limited macular translocation. Am J Ophthalmol. 2000. 130:751–762.
7. Reichel E, Berrocal AM, Ip M, et al. Transpupillary thermotherapy of occult subfoveal choroidal neovascularization in patients with age-related macular degeneration. Ophthalmology. 1999. 106:1908–1914.
8. Spraide RF, Guyer DR, McCormick B, et al. External beam radiation therapy for choroidal neovascularization. Ophthalmology. 1998. 105:24–30.
9. Treatment of Age-related Macular Degeneration with Photodynamic Therapy (TAP) Study Group. Photodynamic therapy of subfoveal choroidal neovascularization in age-related macular degeneration with verteporfin: one-year results of 2 randomized clinical trial - TAP report. Arch Ophthalmol. 1999. 117:1329–1345.
10. Verteporfin In Photodynamic Therapy Study Group. Verteporfin therapy of subfoveal choroidal neovascularization in age-related macular degeneration: two-year results of a randomized clinical trial including lesions with occult with no classic choroidal neovascularization - verteporpin in photodynamic therapy report 2. Am J Ophthalmol. 2001. 131:541–560.
11. Ho AC, Yannuzzi LA, Pisicano K, et al. The natural history of idiopathic choroidal subfoveal neovascularization. Ophthalmology. 1995. 102:782–789.
12. Verteporfin round table 200 and 2001 participants. Treatment of age-related macular degeneration with photodynamic therapy (TAP) study group principal investigators. Verteporfin in photodynamic therapy (VIP) study principal investigators. Guideline for using verteporfin (visudyne) in photodynamic therapy to treat choroidal neovascularization due to age-related macular degeneration and other causes. Retina. 2002. 22:6–18.
13. Iida T, Hagimura N, Kishi S, et al. Indocyanine green angiographic features of idiopathic submacular choroidal neovascularization. Am J Ophthalmol. 1998. 126:70–76.
14. Saari M. Disciform detachment of the macular, fluorescein and ICG fluorescence of angiographic findings in juvenile hemorrhage macular choroidopathy. Acta Ophthalmol. 1077. 55:530–538.
15. Ahn JK, Chung H, Yu HG. Natural history and visual prognosis of idiopathic choroidal neovascularization. J Korean Ophthalmol Soc. 2003. 44:665–662.
16. Thomas MA, Dickinson JD, Melberg NS, et al. Visual results after surgical removal of subfoveal choroidal neovascular membranes. Ophthalmology. 1994. 101:1384–1396.
17. Melberg NS, Thomas MA, Burgess DB. The subfoveal removal of subfoveal choroidal neovascularization. Retina. 1996. 16:190–195.
18. Shiraga F, Shiragami C, Matsuo T, et al. Identification of ingrowth site of idiopathic subfoveal choroidal neovascularization by indocyanine green angiography. Ophthalmology. 2000. 107:600–607.
19. Gass JDM. Biomicroscopic and histopathologic considerations regarding the feasibility of surgical excision of subfoveal choroidal neovascular membranes. Am J Ophthalmol. 1994. 118:285–298.
20. Grossniklaus HE, Gass JD. Clinicopathologic correlations of surgicallyexcised type 1 and type 2 submacular choroidal neovascular membranes. Am J Ophthalmol. 1998. 126:59–69.
21. Grossniklaus HE, Hutchinson AK, Capone A, et al. Clinicopathologic features of surgically excised choroidal neovascular membranes. Ophthalmology. 1994. 101:1099–1111.
22. Campochiaro PA, Morgan KM, Conway BP, Stathos J. Spontaneous involution of subfoveal neovascularization. Am J Ophthalmol. 1990. 109:668–675.
23. Itagaki T, Ohkuma H, Kato N. Studies on experimental subretinal neovascularization: Regression of new vessels. Nippon Ganka Gakkai Zashi. 1985. 89:941–948.
24. Miller H, Miller B, Ryan SJ. The role of retinal pigment epithelium in the involution of subretinal neovascularization. Invest Ophthalmol Vis Sci. 1986. 27:1644–1652.
25. Glaser BM, Campochiaro PA, Davis JL Jr, et al. Retinal pigment epithelial cells release inhibitors of neovascularization. Ophthalmology. 1987. 94:780–784.
26. Spaide RF, Martin ML, Slakter J, et al. Treatment of idiopathic subfoveal choroidal neovascular lesions using photodynamic therapy with verteporfin. Am J Ophthalmol. 2002. 134:62–68.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download