Abstract
Purpose
To evaluate the results of nasolacrimal polyurethane stent implantations for the treatment of primary acquired nasolacrimal duct obstruction, and to determine the effects of various surgical procedures, including stent removal, in subsequent nasolacrimal duct obstruction.
Methods
This study included 15 patients who had nasolacrimal polyurethane implantations for the treatment of primary acquired nasolacrimal duct obstruction. Occluded stents were removed either by nasal endoscopy or during dacryocystorhinostomy (DCR). Cultures and biopsies were performed on the removed stents, and the results of the secondary DCR were analyzed for a 6-month follow-up period.
Results
During stent removal surgery, various degrees of chronic inflammatory reaction and fibrous tissue formation were detected in the lacrimal sac and nasolacrimal duct. Formations of granuloma and fibrous tissue were found in 15 eyes, and culture-positive reaction were found in nine of the 15 eyes. Conventional dacryocystorhinostomy surgery was performed in nine of the 15 eyes and a silicone tube was located at the canaliculi. Subjective and objective outcome were favorable in 13 of the 15 eyes.
Conclusions
The success rate of nasolacrimal polyurethane stent implantation for the treatment of primary acquired nasolacrimal duct obstruction is low. This may result from a chronic inflammatroy reaction. Despite the low success rate of nasolacrimal polyurethane stent implantation, the success rate of endonasal DCR as a subsequent surgery is favorable.
The nasolacrimal system, which permits the drainage of tear fluids from the eye into the nasal cavity, may develop obstructions resulting from various pathologic conditions, such as traumatic disruption or infections of the eyes or nose, the formation of scar tissue or lithiasis, or congenital malformations.1 These lacrimal duct obstructions may lead to excessive tearing known as epiphora; purulent secretion, which is especially visible with pressure on the lacrimal canals; or recurring lacrimal sac inflammation.2
The usual treatment for nasolacrimal obstruction external dacryocystorhinostomy. The disadvantages of this treatment include facial scarring, excessive hemorrhaging, and the disruption of the medial canthal anatomy.
Recently, two types of interventional procedures, balloon dilation and expandable metallic stent or plastic stent placement, have been advocated for the treatment of epiphora. These procedures offer several advantages over invasive surgical procedures, including the: general anesthesia is not needed, the procedures are simple and safe, no facial scar is produced, bleeding is less problematic, substantial anatomic alteration is minimized, and the procedures are more easily tolerated by patients. Technical and clinical success rates of balloon dilation of between 56 and 95% have been described in the literature; however, the long-term effectiveness of balloon dacryocystoplasty is not encouraging in cases of complete obstruction of the lacrimal system, with a recurrence rate higher than 50% at one year.3-9
In 1995, as an alternative to dacryocystorhinostomy, Song et al. designed a polyurethane stent; in 1998 they described its retrograde placement under fluoroscopic guidance.10 The early results of stent treatment were promising. In several studies with a follow-up period of less than one year, the success rate of the procedure ranged from 85% to 98%. However, the long-term results achieved using polyurethane stents have not been as encouraging.11-21
After the removal of an occluded stent, dacryocystorhinos tomy and silicone tube intubation have been advocated for lacrimal duct obstruction.
The purpose of this retrospective study was to determine the long-term durability of nasolacrimal polyurethane stents and to determine the effectiveness of various surgical procedures after occluded stent removal.
Between July 2002 and August 2004, polyurethane stents were removed from the lacrimal drainage systems of 15 patients who had recurrent acquired nasolacrimal duct obstruction after the insertion of a polyurethane stent. Endonasal dacryocystorhinostomies were performed for epiphora correction by the Department of Ophthalmology at Busan Paik Hospital of Inje University. The patient group (n=15) consisted of 5 men and 10 women who ranged in age from 40 to 72 years (mean age, 57.53±9.95 years).
All patients had severe epiphora. Nasolacrimal duct obstruction was confirmed using the prolonged dye retention test and lacrimal irrigation. The mean interval between the insertion of the polyurethane stent and the presentation of severe epiphora (grade III-IV on Munk's scale) was 5.93±1.33 years.
After the removal of the occluded polyurethane stent, we performed an endonasal dacryocystorhinostomy on each patient. Clinical examinations were performed one day and one week after the occluded stent removal, and again at 1, 3, 6, and 12 months. Dacryocystography and flushing with saline solution were carried out only if patients reported the recurrence of epiphora. The average follow-up period was 13.6±2.2 months.
Epiphora was evaluated subjectively according to the scale of Munk et al: grade 0 indicates no epiphora; grade 1 indicates occasional epiphora requiring drying or dabbing less than twice a day; grade 2 indicates epiphora that requires drying two to four times a day; grade 3 indicates epiphora that requires drying five to 10 times a day; grade 4 indicates epiphora that requires drying more than 10 times a day; and grade 5 indicates constant tear overflow. The criterion for inclusion in the study group was grade 3-4 epiphora despite polyurethane stent implantation. Upon a patient's final visit, we defined a successful outcome as grades of 0 or 1 on both Munk's scale and the dye (2% fluorescein) disappearance test. Upon removal of the polyurethane nasolacrimal stent, endoscopic monitoring and a biopsy were performed if the lacrimal sac and mucosal layer exhibited inflammation, granulation, or fibrotic change. Histopathologic evaluations of the biopsy specimens were performed.
Topical decongestant (10% cocaine liquid-soaked pledgets) was applied to the nasal cavity and the lateral nasal wall anterior to the middle turbinate was infiltrated with anesthetic (Xylocaine, Astra Pharmaceuticals, N. Ryde, Australia). The 0° Storz endoscope (Storz, St. Louis, Mo., U.S.A.) was used if an submucosal resection was performed; otherwise, the 30° scope was used.
A scalpel was used to cut a mucosal flap trapdoor in the lateral nasal wall. The incision was started 8 mm above the insertion of the middle turbinate, and then anterior to the axilla of the middle turbinate for 8 mm. A vertical incision was made to just above the inferior turbinate insertion, which was taken posteriorly to the insertion of the uncinate process.
A suction Freer elevator (Martin, Tutligen, Germany) was used to elevate the mucosal flap in a layer of mucoperiosteum. The thin lacrimal bone was elevated off the posterior half of the lower lacrimal sac up to the insertion of the uncinate process. There is always approximately 3 to 4 mm of thin lacrimal bone overlying the posteroinferior portion of the sac before the origin of uncinate process. With the use of a Hajek-Koeffler forward-biting punch (Martin, Tutligen, Germany), the hard, thick bone of the frontal process of the maxilla was removed and the inferior half of the sac uncovered. Bone removal was continued upward for about 5 to 8 mm until the bone became too thick to remove with the punch and access was more difficult.
A Bowmans probe (Martin, Tutligen, Germany) was passed horizontally through the canaliculi and the medial wall of the sac was tented to ensure that all bone was removed over the lacrimal sac and common canaliculus opening. The eventual rhinostomy size was 15 mm×20 mm. The bone removed included parts of the frontal process of the maxilla and root of middle turbinate and all of the lacrimal bone. It was not necessary to remove the uncinate process of the ethmoid.
The probe was then used to tent the medial wall of the sac on its posterior aspect, while the sac was opened vertically along its entire length, creating a large anterior flap. The vertical cut was supplemented with cuts at the superior and inferior ends, allowing the anterior and posterior lacrimal sac flaps to open outward, away from the sac lumen. After trimming to leave only a rim of mucosa superiorly and inferiorly, the original nasal mucosa was reflected back onto the lateral nasal wall to meet the flaps from the lacrimal sac. This allowed the sac to heal without granulation tissue or scarring. The canaliculi were intubated and a "splint" of Gelfoam (Pharmacia, NSW, Austrailia) was placed to ensure flap apposition for the first few postoperative days.
Fifteen eyes with failed stents underwent dacryocystorhinostomy combined with silicone tube implantation at an average of 5.93±1.33 years after initial stent placement. Stent failure was confirmed by identifying re-obstruction using the dye disappearance test and irrigation with saline solution.
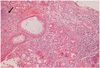
In surgery, the lacrimal sac was shrunk and firmly attached to the stent by fibrous bands in all eyes. Inflammation and granulation tissue growth were detected in the polyurethane nasolacrimal stents (Fig. 1). Tissue growth coverd and intruded into the mushroom heads of the stents. Because of these adhesions, the stents were removed with difficulty. The sac walls were thin, hyperemic, and fragile. Particular effort was made not to damage the sac walls during stent removal. Dacryocystorhinostomy was combined with silicone intubation to prevent the closure of the mucosal anastomosis due to possible excessive inflammatory response and scarring.
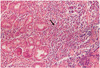
Histologic examinations of tissue samples obtained from the removed stents and from the lacrimal sac biopsy specimens showed chronic inflammation, granulomatous inflammation, and the variable loss of differentiated epithelial cells ranging from a denuded epithelium to basal cell hyperplasia, which is often associated with squamous metaplasia (Fig. 2).
Of the 15 samples, nine (60%) yielded a positive microbial culture. Of the patients with positive culture results, all had pure cultures with a single pathogen; there were no mixed cultures. All of the microorganisms in our study were gram-negative bacteria. The most frequently observed bacterial species was Pseudomonas aeruginosa, which was isolated from 40% (six) of the 15 samples and represented 66.6% of the total culture-positive bacterial isolates (Fig. 3, Table 1).
During patients' final visits, objective and subjective improvements were reported in 13 out eyes of 15 eyes.
Epiphora is a very common condition in ophthalmologic practice, constituting an important portion of lacrimal ophthalmologic practice. It is an annoying disability and, when untreated, tends to result in a vicious cycle including chronic irritative lacrimal conjunctivitis and, sometimes, an eczematous condition on the eyelids. Treatment options for epiphora include; probing, silicone tubing, dacryocystorhinos tomy, and radiologic intervention such as ballon dacryocystoplasty and lacriamal duct stent placement.
Song et al attempted to demonstrate the value of an expandable metallic stent in the lacrimal system, but the metallic stent had some limitations. First, it could be removed only by surgery; second, it lacked longitudinal flexibility; and finally, it was easily obstructed by granulation tissue.10,22-28
Plastic-nylon stents, which overcome these disadvantages, have gained favor. However, previous balloon dilation is required for these stents and in many cases, the stent needs to be cut or shortened, because its rigidity causes discomfort when it rests on the base of the nasal fossa.
These limitations induced Song et al to design the new, soft, polyurethane stent.10 The polyurethane nasolacrimal stent has advantages over external dacryocysto rhinostomy in the treatment of nasolacrimal duct obstruction. The nasolacrimal stent implantation is an interventional radiologic procedure rather than an invasive surgery. In nasolacrimal stent implantation, the total procedure time is short, the administration of general anesthesia is not necessary, patient discomfort and bleeding are minimal, facial skin incisions and osteotomy are not needed, and the natural pathway of tear drainage is preserved.
The early results of polyurethane stent placement were comparable with the results of external dacryocystorhinostomy. Success rates ranged from 85% to 98% in studies with follow-up periods of less than one year.11-19 Subsequent studies with longer follow-up periods; however, reported lower success rates.19-21 Kang et al reported that the long-term success rate of polyurethane stents decreased to 12.3% after three years and 5.3% after five years.20 In our study, the mean interval between the insertion of a polyurethane stent and the presentation of severe epiphora (Grade III-IV on Munk's score) was 5.93±1.33 years; all the patients were diagnosed using a dye disappearance test and DCG.
Despite low success rates in long-term observations, there are few reports regarding dacrycystorhinostomy after occluded stent removal is insufficient.25-34 In 1996, Song et al observed that stents did not seem to disturb subsequent dacryocystorhinostomy.11 However, Yazici et al. reported that the lacrimal sac was shrunken in all eyes that underwent external dacryocystorhinostomies ducts because of stent failure.21
In the largest study reporting on the microbiology of the adult dacryocystitis, which involved 236 patients from a previous study, gram-positive bacteria accounted for 54.0% of the overall microbial studies.35 Song et al. observed the growth of granulation tissue in stent cavities in 65% of the occluded stents.13 However in our study, the relative frequency of gram-negative bacteria was accounted high. Also, P. aeruginosa accounted for 66.6% of the gramnegative bacteria.
In conclusion, polyurethane stent implantation did not seem to be the primary choice for treatment of lacrimal obstruction, and long-term prognoses were not favorable due to long-term occlusion from detritus or the growth of inflammatory tissue.
Our study suggests that most of the adult patients with polyurethane stent implantation harbor microorganism in their lacrimal sacs.
After the removal of the occluded polyurethane stent, shrinkage and contracture of the lacrimal sac might have a negative effect on the subsequent operative procedure and the results of the operation. Although these alterations may cause difficulties in subsequent DCR, epiphora can still be relieved with meticulous surgery. In patients with nasolacrimal polyurethane stents implantation and evidence of nasolacrimal duct obstruction, it is recommended endonasal dacryocystorhinostomy with silicone tube implantation and antimicrobial prophylaxis.
Figures and Tables
Fig. 1
Inflammation (a. arrow) and granulation tissue (b. arrow) in Polyurethane nasolacrimal stent lumen were detected.

Fig. 2
Dense infiltration of lymphoplasma cells (arrow) observed beneath the detached epithelium (H&E, ×100)
References
1. Kim BO, Jin KH, Oh JH. Clinical observation on nasolacrimal duct stent intubation on obstruction of nasolacrimal system. J Korean Ophthalmol Soc. 1995. 36:994–999.
2. Paul L, Pinto I, Vincente JM. Treatment of complete obstruction of the nasolacrimal system by temporary placement of nasolacrimal polyurethane stents: preliminary results. Clinical Radiology. 2003. 58:876–882.
3. Berkefeld J, Kirchner J, Muller HM, et al. Ballon dacryocystoplasty: indications and contraindicstions. Radiology. 1997. 205:785–790.
4. Liermann D, Berkefeld J, Fries U, et al. Balloon dacryocystoplasty: an alternative treatment for obstructed tear ducts. Ophthalmologica. 1996. 10:319–324.
5. Song HY, Ahn HS, Park ChK, et al. Complete obstruction of the nasolacrimal system. Treatment with Balloon dilatation. Radiology. 1993. 186:367–371.
6. Lee JM, Song HY, Han YM, et al. Balloon dacryocystoplasty: results in the treatment of complete and partial obstructions of the nasolacrimal system. Radiology. 1994. 192:503–508.
7. Fenton S, Clearly PE, Horan E, et al. Balloon dacryocystoplasty study in the management of adult epiphora. Eye. 2001. 15:67–69.
8. Rosen N, Shamir M, Moverman DC, Rosner M. Dacryocystorhinostomy with silicone tubes: evaluation of 253 cases. Ophthalmol Surg. 1989. 20:115–119.
9. Yazici Z, Yazici B, Parlak M. Treatment of obstructive epiphora in adults by balloon dacryocystoplasty. Br J Ophthalmol. 1999. 83:692–696.
10. Song HY, Jin YH, Kim JH, et al. Nonsurgical placement of a nasolacrimal polyurethane stent. Radiology. 1995. 194:233–237.
11. Song HY, Jin YH, Kim JH, et al. Nonsurgical placement of a nasolacrimal polyurethane stent: long-term effectiveness. Radiology. 1996. 200:759–763.
12. Pulido-Duque JM, Reyes R, Carreira JM, et al. Treatment of complete and partial obstruction of the nasolacrimal system with polyurethane stents: initial experience. Cardiovasc Intervent Radiol. 1998. 21:41–44.
13. Song HY, Lee DH, Ahn H, et al. Lacrimal system obstruction treated with lacrimal polyurethane stents: outcome of removal of occluded stents. Radiology. 1998. 208:689–694.
14. Lee JS, Jung G, Oum BS, et al. Clinical efficacy of the polyurethane stent without fluoroscopic guidance in the treatment of nasolacrimal duct obstruction. Ophthalmology. 2000. 107:1666–1670.
15. Yazici B, Yazici Z, Parlak M. Treatment of nasolacrimal duct obstruction in adults with polyurethane stent. Am J Ophthalmol. 2001. 131:37–43.
16. Pabon IP, Diaz LP, Grande C, de la Cal Lopez MA. Nasolacrimal polyurethane stent placement for epiphora: technical long-term results. J Vasc Interv Radiol. 2001. 12:67–71.
17. Perena MF, Castillo J, Medrano J, et al. Nasolacrimal polyurethane stent placement: preliminary results. Eur J Ophthalmol. 2001. 11:25–30.
18. Lanciego C, De Miguel S, Perea M, et al. Nasolacrimal stents in the management of epiphora: medium-term results of a multicenter prospective study. J Vasc Interv Radiol. 2001. 12:701–710.
19. Paul L, Pinto I, Vicente JM, et al. Nasolacrimal stents in the treatment of epiphora: long-term results. J Vasc Interv Radiol. 2002. 13:83–88.
20. Kang SG, Song HY, Lee DH, et al. Nonsurgically placed nasolacrimal stents for epiphora: long-term results and factors favoring stent patency. J Vasc Interv Radiol. 2002. 13:293–300.
21. Yazici Z, Yazici B, Parlak M, et al. Treatment of nasolacrimal duct obstruction with polyurethane stent placement: long-term results. Am J Roentgenol. 2002. 179:491–494.
22. Munk PL, Lin DT, Morris DC. Epiphora: treatment by means of dacryocystoplasty with balloon dilation of the nasolacrimal drainage apparatus. Radiology. 1990. 177:687–690.
23. Janssen AG, Mansour K, Krabbe GJ, et al. Dacryocystoplasty: treatment of epiphora by means of balloon dilation of the obstructed nasolacrimal duct system. Radiology. 1994. 193:453–456.
24. Ilgit ET, Yuksel D, Unal M, et al. Transluminal balloon dilatation of the lacrimal drainage system for the treatment of epiphora. Am J Roentgenol. 1995. 165:1517–1524.
25. Berkefeld J, Kirchner J, Muller HM, et al. Balloon dacryocystoplasty: indications and contraindications. Radiology. 1997. 205:785–790.
26. Lee JM, Song HY, Han YM, et al. Balloon dacryocystoplasty: results in the treatment of complete and partial obstructions of the nasolacrimal system. Radiology. 1994. 192:503–508.
27. Yazici Z, Yazici B, Parlak M, et al. Treatment of obstructive epiphora in adults by balloon dacryocystoplasty. Br J Ophthalmol. 1999. 83:692–696.
28. Fenton S, Cleary PE, Horan E, et al. Balloon dacryocystoplasty study in the management of adult epiphora. Eye. 2001. 15:67–69.
29. Song HY, Ahn HS, Park CK, et al. Complete obstruction of the nasolacrimal system, II: treatment with expandable metallic stents. Radiology. 1993. 186:372–376.
30. Ilgit ET, Yuksel D, Unal M, et al. Treatment of recurrent nasolacrimal duct obstructions with balloon-expandable metallic stents: results of early experience. Am J Neuroradiol. 1996. 17:657–663.
31. Tucker N, Chow D, Stockl F, et al. Clinically suspected primary acquired nasolacrimal duct obstruction: clinicopathologic review of 150 patients. Ophthalmology. 1997. 104:1882–1886.
32. Mauriello JA Jr, Palydowycz S, DeLuca J. Clinicopathologic study of lacrimal sac and nasal mucosa in 44 patients with complete acquired nasolacrimal duct obstruction. Ophthal Plast Reconstr Surg. 1992. 8:13–21.
33. Lee-Wing MW, Ashenhurst ME. Clinicopathologic analysis of 166 patients with primary acquired nasolacrimal duct obstruction. Ophthalmology. 2001. 108:2038–2040.
34. Bernardini FP, Moin M, Kersten RC, et al. Routine histopathologic evaluation of the lacrimal sac during dacryocystorhinostomy: how useful is it? Ophthalmology. 2002. 109:1214–1218.
35. Chaudhry IA, Shamsi FA, Al-Rashed W. Bacteriology of chronic dacryocystitis in a tertiary eye care center. Ophthalmic Plast Reconstr Surg. 2005. 21:207–210.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download