Abstract
Purpose
The authors hereby describe a case of Wernicke-Korsakoff syndrome with accompanying ocular findings that is caused by hyperernesis gravidarum.
Methods
We experienced a 27-year-old female at 12 weeks of pregnancy, who visited our clinic because of weight loss, gait disturbance, decreased mentality and dizziness after prolonged vomiting for 2 months. Neurological examination demonstrated ataxia of gait and loss of orientation. Ophthalmologic examination showed decreased visual acuity, upbeat nystagmus, diplopia and retinal hemorrhage.
Wernicke-Korsakoff syndrome is prevalent among thiamine-deficient patients, and its clinical symptoms include nystagmus, extraocular muscle paralysis, gait disturbance, and memory loss. The syndrome is common among alcohol abusers, patients with malignant tumor or gastrointestinal diseases, those who undergo hemodialysis or long-term peritoneal dialysis, pregnant women, women who breast-feed, and patients with hyperthyroidism.1
Nausea and hyperemesis are common between 4 to 8 weeks and 14 to 16 weeks of pregnancy with 70% of pregnant women who reporting such symptoms. The patient may have severe, pregnancy-related hyperemesis during the first trimester, and the condition requires hospitalization because of weight loss of more than 5%, dehydration, electrolyte imbalance, and ketonuria. Very severe cases may combine with liver and kidney dysfunction, immune depression, and psychological problems such as Wernicke-Korsakoff syndrome, and may even lead to death of the patient and fetus.2
Two cases of Wernicke-Korsakoff syndrome associated hyperemesis gravidarum were reported in Korea.3,4 The authors experienced a case of Wernicke-Korsakoff syndrome in a 27-year-old patient at 12 weeks of pregnancy who presented with severe, pregnancy-related hyperemesis, gait disturbance, decreased mentality, decreased vision, nystagmus, diplopia, optic neuropathy and retinal hemorrhage. The authors hereby report this rare case and provide a literature review.
A 27-year-old female patient at 12 weeks of pregnancy reported to the department of obstetrics with hyperemesis, weight loss of 14 kg, dizziness, and anorexia. The patient had been treated at a local clinic but the symptoms had worsened requiring hospitalization. The fetal conditions were good except for mild oligohydramnios.
Her hemoglobin level was 9.2 g/dl but all other blood tests were normal without any clotting disorder. Electrolyte tests were all normal with sodium 140 mmol/L, potassium 3.6 mmol/L, and chloride 109 mmol/L. Thyroid function tests showed decreased levels of TSH (0.03 µIU) and increased levels of free T4 (3.53 ng/dl) and T3 (240.6 ng/dl). Vitamin B12 (1302 pg/ml), and folate (3.50 ng/ml) levels were normal. The authors were not able to obtain her thiamine level at initial routine test because of the patient was suspected of having Graves' disease or thyroid-related hyperemesis gravidarum, but further tests were not performed because her guardian didn't consent.
The patient had clear mental status during the initial days of hospitalization, but then began to lose all perception of time, people, and places, and eventually she was unable to articulate her words and became bed-ridden.
Neurological exams showed dizziness, malaise, and symmetrical rigidity in both upper and lower limbs and vertical nystagmus consisting of spout-like, jerky, upbeat eye movements. The vestibular function test showed slightly low accuracy and velocity in saccadic exam and saccadic movements with left descending arm in pursuit exam. In addition, because the OKN test revealed low-gain instability in both eyes, the authors came to suspect pathology of the brain cortex. The patient had no strength to walk or even stand because of severe dizziness, but deep tendon reflexes of her elbows and knees were normal.
The patient was referred to the otolaryngology department because of dizziness and upbeat nystagmus, and was later referred to the neurology department because the doctors suspected central vertigo.
Her central nervous system exams, including CSF exam and electroencephalogram, were normal. The neurologist suspected Wernicke-Korsakoff syndrome, and performed MRI. T2-weighted MRI (T2WI) results showed high signal changes in both medial thalami, the third ventricle, and periaqueductal white matter. In diffusion-weighted images (DWI), the lesions showed bilateral and symmetrical high signal intensity, confirming the diagnosis of Wernicke's encephalopathy (Fig. 1).
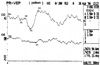
After eight days of hospitalization, the patient was referred to the department of ophthalmology with decreased vision. The patient had undergone LASIK surgery 1 year prior to the admission, and her first ocular exams showed no abnormal refractive findings with visual acuity of 5/20 in both eyes. Her intraocular pressures was 10 mmHg in both eyes and the patient showed no abnormalities in her external eyes. Pupil responses to light as well as her pupil sizes were all normal. Ocular motility evaluation demonstrated orthotropia in the primary and secondary position. On duction testing, her both eye showed mild limitation on attempted abduction. She felt binocular diplopia on both extreme lateral gazes. Upbeat nystagmus had disappeared by the time of the ocular examination, but fundus examination revealed peripapillary retinal hemorrhage and slightly pale optic disc in both eyes. The patient neither had neither hypertension nor clotting disorder which may have caused retinal hemorrhage. The amount of hemorrhage was less severe in her left eye and had all disappeared after three days when color photos of her eyes were taken (Fig. 2). Although retinal hemorrhages decreased, the patient complained of nystagmus and recurred decreased vision. Her eye sights was 20/100 in the right and 20/400 in the left, and visual evoked potential (VEP) exam showed increased latency and decreased amplitude in her left eye (Fig. 3).
Even though the patient's initial thiamine level was not determined, the authors decided on a diagnosis of Wernicke-Korsakoff syndrome after conducting the above-mentioned exams. The patient therefore received fluid infusion with multi-vitamins including thiamine and other electrolytes. Over the course of a week her symptoms slowly improved, including hyperemesis, inability to articulate, nystagmus, malaise, gait disturbance, memory loss, and perception of time, people, and places. On the other hand, the nystagmus and diplopia were resolved dramatically within 48 hours of the initiation of treatment. In addition, the visual acuity improved to 20/40 in the right and 20/80 in the left. Two days after the infusion of thiamine, her thiamine level had almost normalized at 1.85 µg/dl, which approached the normal range of 2 to 7.2 µg/dl. After being discharged from the hospital, the patient did not report back to the clinic, any without any follow-up examination the authors have not been able to determine her current physical status.
Wernicke-Korsakoff syndrome arises due to thiamine deficiency and is common among alcohol abusers, but it also appears in cases of malnutrition, malignant tumor, gastrointestinal dysfunction, pregnancy, and hyperthyroidism, and in patients who breast-feed and undergo hemodialysis or peritoneal dialysis.1 Thiamine is one of many essential vitamins, with a recommended daily dosage of 5 mg through various kinds of food as the human body accumulated 25 to 30 mg of thiamine. During pregnancy, the demand for thiamine increases three-fold, and 1.5 mg of supplemental thiamine ingestion is recommend daily.5 Free thiamine, which is converted into thiamine diphosphate after going through the blood-brain-barrier, is known as one of the cofactors which aid in energy metabolism within the brain. Thiamine deficiency causes deprivation of transketolase which is a thiamine-dependent enzyme in pentose phosphate pathway. As a result, pyruvic acid and lactic acid accumulate within the brain, causing changes in the energy metabolism, activation of cellular membranes, and concentration of nerve conduction molecules, thereby damaging the nervous system. Thiamine deficiency is known to cause Wernicke's syndrome, but its pathophysiology is still uncertain.6
Clinical syndromes due to thiamine deficiency can be classified into wet beri-beri which affects cardiovascular system and dry beri-beri or Wernicke-Korsakoff syndrome with neurological dysfunctions.7,12
The triad of Wernicke-Korsakoff syndrome symptoms includes paralysis of extraocular movement, gait disturbance, and disturbance of mentation and consciousness. These three symptoms can appear simultaneously, but one may precede the others by several days or several weeks.
After the syndrome phases to Korsakoff psychosis, the patient manifests symptoms quite different from Wernicke's encephalopathy such as memory loss, but Wernicke's encephalopathy and Korsakoff psychosis are known as acute and chronic phases in the clinical progression of the same syndrome, respectively.1,13,14
In the acute phase, necrosis of variable severity and hemorrhage can appear in certain occasions in the medial thalamus, mamillary body, hypothalamus, periaqueductal area of midbrain, floor of fourth ventricle, and upper cerebellar area. In the chronic phase, proliferation of glial cells and progression of vessels can occur, and, in cases of continuous memory loss, a lesion may appear in the medial aspect of the thalamus. When the syndrome is well progressed, the patient may experience complete paralysis of extraocular movement, although pupil responses are usually remain normal. However, the patient may report loss of pupil responses as well as miosis, and other ocular findings, such as ptosis, small retinal hemorrhage, involvement of the near-far focusing mechanism and evidence of optic neuropathy, occur occasionally.7 However, in under 5% of patients, the syndrome may also manifest as optic papillitis or papilledema which can even lead to loss of vision. Retinal hemorrhage is reported to be a common fundus finding, but its pathogenesis hasn't been determined yet.8 In acute stages of the disease, cerebral blood flow and cerebral oxygen and glucose consumption are reduced dramatically, causing ischemic damages, these changes may affect the blood vessel endothelium, and the combination of these effects may give rise to retinal hemorrhage and optic neuropathy.7,9,10 Another possible mechanism is thiamine, an essential cofactor in various stages of carbohydrate metabolism. Transketolase is a thiamine-dependent enzyme in the pentose phosphate pathway, and in Wernicke's encephalopathy the activity level is usually low.10 Recently there have been reports that the lipid-soluble, thiamine derivative, benfotiamine, can inhibit three pathways that are implicated in the pathogenesis of hyperglycemia-induced vascular damage: the hexosamine pathway, the advanced glycation end product (AGE) formation pathway and the diacylglycerol (DAG)-protein kinase C (PKC) pathway. These pathways are activated by increased availability of the glycolytic metabolites glyceraldehyde-3-phosphate and fructose-6-phosphate, as well as by hyperglycemia-associated, NF-kappaB activation, and by activating the pentose phosphate pathway enzyme transketolase, converts glyceraldehyde-3-phosphate and fructose-6-phosphate into pentose-5-phosphates and other sugars. In retinas of diabetic animals, benfotiamine treatment inhibited these three pathways, inhibited NF-kappaB activation by activating transketolase, and also prevented experimental diabetic retinopathy.11 Therefore, these above-mentioned reports, suggest that thiamine deficiency causes a decrease in transketolase activity, and that this may cause vascular damage, all of which can give rise to retinal hemorrhage.
The ocular muscle and gaze palsies are attributable to lesions of the sixth and third nerve nuclei, while the adjacent tegmentum and the nystagmus are due to lesions in the regions of the vestibular nuclei. In the absence of significant destruction of nerve cells in these lesions, the patient may show a high degree of recovery in oculomotor and vestibular functions.7
The physician may diagnose syndrome with typical history of malnutrition and characteristic findings such as paralysis of extraocular movement, gait disturbance, and disturbance of mentation and consciousness combined with memory loss. The diagnosis can be confirmed when clinical symptoms improve after ingestion of thiamine.
Radiological diagnosis can be made for Wernicke's encephalopathy when MRI shows high signal changes in the periaqueductal area and medial aspects of both thalami, and in the case of atrophy of papilla. For Korsakoff psychosis, the third ventricle appears to be expanded because of atrophy of the medial aspect of thalamus. Such radiological findings are evident in comatose patients but are dubious in patients with mainly ocular paralysis or gait disturbance. Such high signal changes can disappear after ingestion of thiamine.15
When Wernicke-Korsakoff syndrome due to pregnancy-related hyperemesis is suspected, thiamine should be administered immediately, thus halting the progression of the syndrome and promoting reversal of the brain lesion provided that irreversible structural changes have not occurred.
Ocular paralysis can improve after 2 to 3 mg of thiamine is given to a patient, but 50 mg of thiamine should be given IV or IM in order to promote continuous improvement until normal dietary intake is possible. Infusion of glucose in patients with depleted thiamine accumulation is known to cause progression of Wernicke's encephalopathy because thiamine demand increases in the metabolism of carbohydrates.7 With such supplements, ocular paralysis improves within several hours to a week, and horizontal nystagmus continues in 35% of patients. Confusion improves between several hours to several days after thiamine supplementation, and it usually disappears within a month. Gait disturbance may improve within several hours, but such recovery takes place in less than 50% of patients and in 35% of patients show no improvements. Up to 80% of patients may continue to have memory loss, whereas less than 25% of patients slowly recover their memories after several months.16
In the present case, the pregnant woman had hyperemesis with nausea of more than two-month duration, and initially had upbeat nystagmus, ocular findings such as retinal hemorrhage, optic neuropathy and paralysis of extraocular muscles, gait disturbance, disturbance in consciousness, and memory loss. Her MRI results corresponded to the diagnosis of Wernicke-Korsakoff syndrome. After the ingestion of thiamine and other multi-vitamins, her ocular, neurological and psychological dysfunctions were all improved except for a minute amount of retinal hemorrhage remaining.
As Wernicke-Korsakoff syndrome can be deadly when left untreated, the presence of severe hyperemesis in pregnant women who also show ocular findings such as extraocular paralysis and retinal hemorrhages should raise the suspicion of Wernicke-Korsakoff syndrome due to thiamine deficiency and should prompt doctors to perform appropriate treatment immediately.
Figures and Tables
 | Fig. 1MRI result (T2-weighted image, A) showing high signal changes in both medial thalami, 3rd ventricle, and periaqueductal white matter (arrow), and diffusion weighted image (DWI, B) with the lesions showing bilateral and symmetrical high signal intensity. |
References
1. Wilson JD. Isselbacher KJ, Braunwald E, Wilson JD, editors. Vitamin deficiency and excess. Harrison's principles of internal medicine. 1994. v. 1.:13th ed. New York: McGraw-Hill;chap. 77.
2. Levine MG, Esser D. Total parenteral nutrition for the treatment of severe hyperemesis gravidarum: maternal nutritional effect and fetal outcome. Obstet Gynecol. 1988. 72:102–107.
3. Lee JC, Jeong EH, Roh JS, et al. A case of Wernicke-Korsakoff syndrome associated with hyperemesis gravidarum. J Korean Obstet Gynecol. 1997. 40:429–433.
4. Kim YH, Lee SJ, Yoon JK, et al. Wernicke's syndrome induced by hyperemesis gravidarum. J Korean Ophthalmol Soc. 2001. 42:538–541.
5. The National Research Council Committee on Dietary Allowance. Food and Nutrition Board. Recommended Dietary Allowances. 1980. 9th ed. Washington, DC: National Academy of Science;178–185.
6. Davis R, Icke GC. Clinical chemistry of thiamin. Adv Clin Chem. 1983. 2:93–140.
7. Adams RD, Victor M, Ropper AH. Principles of Neurology. 2001. 7th ed. New York: McGraw-Hill;1205–1212.
8. Mumford CJ. Papilloedema delaying the diagnosis of Wernicke's encephalopathy in a comatous patient. Postgrad med J. 1989. 65:371–373.
9. Bergin PS, Harvey P. Wernicke's encephalopathy and central pontine myelolysis associated with hyperemesis gravidarum. BMJ. 1992. 305:517–518.
10. Peter JG. Wernicke's encephalopathy and hyperemesis gravidarum. BMJ. 1992. 305:1096.
11. Hammes HP, Du X, Edelstein D, et al. Benfotiamine blocks three major pathways of hyperglycemic damage and prevents experimental diabetic retinopathy. Nat Med. 2003. 9:294–299.
12. Maurice V, Martin JB. Isselbacher KF, editor. Nutritional and metabolic diseases of the nervous system. Harrison's principles of internal medicine. 1994. v. 2:13th ed. New York: McGraw-Hill;chap. 377.
13. Ohkoshi N, Ishii A, Shoji S. Wernicke's encephalopathy induced by hyperemesis gravidarum, associated with bilateral caudate lesions on computed tomography and magnetic resonance image. Eur neurology. 1994. 34:177–180.
14. Poloni M, Mazarello P, Laforenza U, et al. Thiamin contents of cerebrospinal fluid, plasma and erythrocytes in cerebellar ataxias. Eur Neurol. 1992. 32:154–158.
15. Victor M. MR in the diagnosis of Wernicke-Korsakoff syndrome. Am J Roentgenol. 1990. 155:1315–1316.
16. Burst JCM. Rowland LP, editor. Environmental neurology: Wernicke-Korsakoff syndrome. Merritt's textbook of Neurology. 2000. 10th ed. Philadelphia: Williams & Wilkins;chap. 157.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download