Abstract
Methods
This study involved 9 eyes from 9 patients who underwent laser photocoagulation coupled with fluid-gas exchange for reopened macular holes. The photocoagulation was performed at the center of the macular hole. Closure of the reopened hole was categorized by optical coherence tomography (OCT) according to the presence (type 1 closure) or absence (type 2 closure) of continuity in the foveal tissue. Best corrected visual acuity (BCVA), closure types, and complications were assessed.
Results
Upon final examination, all macular holes were found to have closed. Six eyes were classified as type 1 closure, and three were classified as type 2 closure. The mean BCVAs, before and after laser photocoagulation, were 0.11 and 0.31, respectively (P<.05). The eyes with type 1 closure were associated with shorter symptom durations and greater visual improvement than those with type 2 closure (P<.05).
The anatomical success rate of surgery for the treatment of idiopathic macular holes ranges from 58% to more than 90%, according to several published studies.1-5 The long-term incidence of macular hole reopening ranges from approximately 2% to 9.5%, depending upon the research cited.6-8 The pathophysiology of recurrent or persistent macular holes is not completely understood. Possible contributing factors include: insufficient relief of vitreous traction, incomplete removal or later development of the epiretinal membrane, inadequate provision of an interface for migration, the proliferation of glial cells resulting from insufficient gas tamponade and poor patient compliance with treatment.9,10
Several therapeutic modalities are available for patients with reopened macular holes. Some researchers have recommended repeat vitrectomies with peeling of the epiretinal or internal limiting membrane, coupled with the utilization of an adjuvant, such as transforming growth factor-beta.11-13 Previous studies have reported that closure of reopened macular holes, which is associated with subsequent vision improvements, can be accomplished with laser photocoagulation at the center of hole coupled with fluid-gas exchange.14-17 The procedure may be done on an outpatient basis.
In a previous report, postoperative appearances of closed macular holes were classified into two patterns by optical coherence tomography (OCT). The classification was based on the presence or absence of bare retinal pigment epithelium (RPE).18 Macular hole closure without bare RPE was associated with more pronounced visual improvement and less frequent recurrence than was the closure with bare RPE. Therefore, we concluded that macular hole closure without bare RPE is the optimal anatomic endpoint for an improved outcome.
The objective of this study was to determine the effects of laser photocoagulation at the center of reopened macular holes coupled with fluid gas exchange, with regard to visual outcome and closure type.
We retrospectively reviewed the medical records of patients who had been treated by laser photocoagulation at the center of reopened macular holes, coupled with gas tamponade for a recurrent or persistent macular hole after initial vitrectomy, in our hospital between June 2001 and October 2004.
All eyes had been initially treated by pars plana vitrectomy, epiretinal membrane peeling when indicated, internal limiting membrane peeling, and fluid-gas exchange with 14% C3F8 (5/9 of eyes) or 25% SF6 (4/9 of eyes) gas.
We used OCT to confirm the reopening of the macular hole during the follow-up period. We performed laser photocoagulation at the center of the reopened hole, coupled with fluid-gas exchange using 15% C3F8 (4/9 of eyes) or 25% SF6 (5/9 of eyes). These treatments were performed on the same day we detected the reopened macular hole in all patients except one. Treatment for this patient was delayed for 1 month due to infectious conjunctivitis. Laser photocoagulation at the center of the hole was conducted with the patient under topical anesthesia, using a fundus contact lens (TransEquator™ lens, Volk Optical Inc., Ohio), and a slitlamp laser delivery system (Novus Omni™; Coherent Inc., Palo Alto, CA) using an argon green wavelength. Three burns, 100 µm in size, 0.06 seconds duration, and 60-100 mW, were applied directly to the pigment epithelium at the center of the macular hole. Laser photocoagulation results in the appearance of subtle gray burns in a triangular configuration (Fig. 1). Fluid-gas exchange was performed after the completion of laser photocoagulation. Under topical anesthesia, the intravitreal fluid was removed and replaced with non-expansile gas using a series of consecutive push-pull maneuvers. After the procedure, patients were encouraged to remain in a facedown position as much as possible for at least ten days. Patients were asked to return two weeks after the procedure for a follow-up ophthalmic examination. The minimum follow-up period after re-treatment was 4 months.
The clinical information we obtained preoperatively included: age, gender, preoperative best-corrected visual acuity (BCVA) as assessed by the Early Treatment Diabetic Retinopathy Study (ETDRS) visual acuity chart, intraocular pressure, refractive error, lens status, and the results of a biomicroscopic examination of the fovea and vitreous. OCT (OCT 2000, Humphrey Instrument, division of Carl Zeiss, San Leandro, CA, USA) examinations, including the assessment of the diameter of the macular hole, were performed before the initial vitrectomy, and then before and after laser photocoagulation. The macular hole diameter was determined by averaging the vertical and horizontal diameters, both of which were measured at the minimal extent of the hole. The OCT appearances of the macular lesions after treatment were classified as either type 1 closure, type 2 closure, or reopened. Type 1 closure indicates the disappearance of the macular hole with no discontinuity of the foveal tissue. Bare RPE on OCT examination was not detected in the type 1 closure. Type 2 closure indicates discontinuity of the foveal tissue, although. The length of foveal discontinuity was reduced postoperatively and the circumference of the hole was flattened. Data, including symptom duration, preoperative hole size, final (BCVA), and the extent of visual improvement, were analyzed and compared between closure types. The BCVA was converted to a logMAR score for statistical analysis.
This study involved 9 eyes from 9 patients. There were 8 females and 1 male, ranging from 61 to 75 years of age, with a mean age of 67.0 years. The clinical characteristics and demographics of these patients are summarized in Table 1. The interval between the initial vitrectomy and the detection of reopening ranged from 2 weeks to 6 months with a mean of 62.4 days. The follow-up period was at least 4 months after the completion of laser photocoagulation (range, 4 to 38 months, mean, 12.9 months).
Upon final examination, all eyes showed closure of the macular hole. In all patients but one (Patient 9), the reopened macular holes were successfully closed with laser photocoagulation performed at the center of the hole, coupled with fluid gas exchange. In the one refractory case (Patient 9), we performed an additional laser photocoagulation to the margin of the hole, coupled with repeated fluid gas exchange, and achieved type 2 closure of the macular hole. Before the initial vitrectomy, this patient's symptoms had lasted 60 months, the longest of our subjects. The diameter of this macular hole was 675.5 µm.
Six eyes (66.7%) were classified as type 1 closure (Fig. 2), and 3 eyes (33.3%) were classified as type 2 closure based on OCT findings (Fig. 3). The data comparing the two groups are shown in Table 2.
The duration of symptoms before initial vitrectomy ranged from 1.5 to 60 months, with a median of 24.8 months. The mean duration of symptoms was 11.5 months in the type 1 closure group, and 51.6 months in the type 2 closure group. This difference was statistically significant (P=.024, Mann-Whitney test). The mean of the initial macular hole diameter in the type 2 closure group (775 µm) was larger than that of the type 1 closure group (588 µm), but this difference was not statistically significant (P= .17, Mann-Whitney test).
The mean BCVA before laser photocoagulation was 0.11, and after laser photocoagulation was 0.31 (P<.01, Wilcoxon signed rank test). No patients experienced a loss of visual acuity compared to pretreatment status (Fig. 4). The mean BCVA before initial vitrectomy was 0.10 in the type 1 closure group, and 0.14 in the type 2 closure group (P=.381). The mean and standard deviation of BCVA after laser photocoagulation with fluid gas exchange were 0.35±0.24 in the type 1 closure group and 0.20±0.00 in the type 2 closure group (P=.548). The mean extent of visual improvement was significantly increased in the type 1 closure than in the type 2 closure group (P=.027, Mann-Whitney test).
No serious complications, such as endophthalmitis or retinal detachment, were noted. A transient elevation in intraocular pressure was noted in 2 cases (Patients 3, 5). This was controlled by the administration of topical medication. The most commonly encountered postoperative complication was the development of nucleosclerotic cataracts, which was seen in 7 (87.5%) of the 8 phakic eyes. Four of these cases were treated with phacoemulsification by the implantation of an intraocular lens. The overall rate of pseudophakia was not significantly different between the two types of macular hole closures.
Because it is sometimes difficult to distinguish between a persistent macular hole and a recurrent hole, both cases were termed "reopened" macular holes in this study.
Several options are available for the treatment of reopened macular holes, such as fluid gas exchange,14,19 repeat vitrectomy (with or without peeling of internal limiting membrane), and adjuvant usage (such as transforming growth factor beta 2 or autologous serum).10,13 The retinal internal limiting membrane around the macular hole had already been removed in all of our patients. In addition, the patients had acceded to our instructions to maintain a facedown position as much as possible for 1 week after the initial vitrectomy. For these reasons, we believed that neither a repeat vitrectomy for the relief of hole traction, nor fluid gas exchange alone would have resulted in improved outcomes.
In this study, we closed the reopened macular hole in all cases using a combination of laser photocoagulation and fluid gas exchange. These results imply that laser photocoagulation strongly promotes closure of the macular hole. Several previous studies have demonstrated that laser photocoagulation at the center of the macular hole, when performed as an adjuvant therapy, promotes the closure of reopened macular holes and, as a result, improves visual outcomes.16,17 The rates of successful closure of reopened macular holes achieved in our study, as well as the resulting visual outcomes, are comparable to those reported in previous studies.
Remarkably, type 1 closure was noted in two-thirds of cases, despite the relatively large size of the macular holes. The mechanism by which macular hole closure is achieved via laser photocoagulation is still not clearly understood. However, it is suspected that laser photocoagulation leads to the production and release of cytokines, such as transforming growth factor beta 2 from the treated RPE.5,17,20 The production of cytokines by the RPE has been demonstrated to promote proliferation of glial cells3-5 and may eventually facilitate the type 1 closure of a macular hole.
OCT examinations revealed reductions in type 2 closure of reopened macular hole diameter, as well as flattening of the hole edge. Thus, we also considered type 2 closure of the macular hole to be a successful outcome. However, type 2 closure is associated with less pronounced visual improvement and a higher incidence of recurrence.18 Therefore, it is both significant and encouraging that laser photocoagulation, in conjunction with fluid gas exchange, accomplished the type 1 closure of reopened macular holes in the majority of cases.
This study demonstrated that type 1 closure of reopened macular holes was correlated with shorter symptom duration before the initial vitrectomy, and with greater visual improvement. Though several reports have asserted that shorter symptom duration correlates with better postoperative visual improvement, other reports have shown the opposite.21-23 This controversy may arise, in part, from the fact that many patients who suffer from a macular hole cannot recall precisely when the symptoms began. This is especially true with elderly patients whose other eye is unaffected. Although the number of subjects in this study is clearly too small to claim statistical significance, the mean preoperative macular hole diameters of the eyes of the type 2 closure group (775 µm) were larger than those of the type 1 closure group (588 µm). Since the degeneration of neural tissue in the fovea tends to be advanced in large macular holes due to the chronicity of the disease process, the absolute diameter of the neural tissue defects also tend to be large. These results imply that early treatment of idiopathic macular holes is crucial, and not only affects initial success, but also facilitates reopening at a later time. Johnson et al14 reported more than two lines of visual improvement in all cases that showed anatomical success within 8 weeks of the detection of a recurrent macular hole. All of our cases were treated as soon as possible, because we believed that early intervention would help prevent further degeneration of photoreceptor cells.
We made a few modifications to the procedure of laser photocoagulation used in previous cases. We applied three spots of 100 µm-sized laser burn, rather than one large laser spot. This was done due to the risk of excessive RPE damage at the center of laser burn which we felt could be circumvented by using three small spots rather than the one large spot.
Laser photocoagulation applied to the RPE within the center of the macular hole can potentially cause central scotoma because the integrity of the RPE beneath the fovea is essential for the recovery of central vision. According to a previous study, scanning laser ophthalmoscopic microperimetry after the application of laser photocoagulation for recurrent macular holes caused clinically insignificant changes in the visual field. As seen with the improved vision reported in our cases, laser photocoagulation does not necessarily result in significant scotoma. This contention is also supported by the improvement of visual outcomes reported in previous studies.5,16,24,25
Although there was one case involving a second reopening of the macular hole, closure was achieved in this case with a repeat of laser photocoagulation at the margin of the hole coupled with fluid gas exchange. Further investigation is required to determine the value of laser photocoagulation performed at the margin of a refractory macular hole.
Laser photocoagulation at the center of the macular hole is believed to have several advantages over other adjuvant therapies. It is simple to perform and caused no complications such as intraocular inflammation.26-28
Although the sample size in our study was too small to claim any definite conclusions, our results suggest that the combination of laser photocoagulation applied to the RPE at the center of the macular hole, coupled with fluid-gas exchange, appears to constitute a safe and effective therapeutic modality for the treatment of both recurrent and persistent macular holes. A long-term follow-up study will be necessary to confirm the safety and durability of this method. It also appears that laser photocoagulation is a potent tool for inducing the closure of macular holes. This procedure may prove to be a useful tool for the treatment of patients with macular holes that reopen despite the complete relief of traction, or for patients unwilling to return to the operating room for an additional procedure.
Figures and Tables
 | Fig. 1Diagram representation of the laser photocoagulation technique used for closing a reopened macular hole after vitreous surgery. Laser spots were applied directly to the RPE at the center of the reopened hole. |
 | Fig. 2Symptom duration in this case (case 1 in Table 1) was 2.3 months, and the hole diameter measured before vitrectomy was 696 µm (A). Type 2 closure of the macular hole was noted 14 days after vitrectomy (B). At 36 days after vitrectomy, we noted the reopening of the macular hole with a diameter of 812.5 µm (C). After laser photocoagulation and fluid gas exchange for the reopened macular hole, type 1 closure was achieved (D). Final visual acuity was 0.5. |
 | Fig. 3The symptom duration in this case (case 7 in Table 1) was 51 months, and the hole diameter measured before vitrectomy was 755.5 µm (A). The reopened macular hole with a diameter of 864.5 µm was noted in the optical coherence tomography 2 months after the procedure (B). Type 2 closure of the reopened macular hole is demonstrated after laser photocoagulation and fluid gas exchange (C). Final visual acuity was 0.2. |
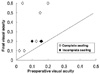 | Fig. 4The changes in the best corrected visual acuity according to the type of macular hole closure. |
References
1. Kelly NE, Wendel RT. Vitreous surgery for idiopathic macular holes. Results of a pilot study. Arch Ophthalmol. 1991. 109:654–659.
2. Wendel RT, Patel AC, Kelly NE, et al. Vitreous surgery for macular holes. Ophthalmology. 1993. 100:1671–1676.
3. Freeman WR, Azen SP, Kim JW, et al. The Vitrectomy for Treatment of Macular Hole Study Group. Vitrectomy for the treatment of full-thickness stage 3 or 4 macular holes. Results of a multicentered randomized clinical trial. Arch Ophthalmol. 1997. 115:11–21.
4. Thompson JT, Smiddy WS, Williams GA, et al. Comparison of recombinant transforming growth factor-beta-2 and placebo as an adjunctive agent for macular hole surgery. Ophthalmology. 1998. 105:700–706.
5. Min WK, Lee JH, Ham DI. Macular hole surgery in conjunction with endolaser photocoagulation. Am J Ophthalmol. 1999. 127:306–311.
6. Park SS, Marcus DM, Duker JS, et al. Posterior segment complications after vitrectomy for macular holes. Ophthalmology. 1995. 102:775–781.
7. Christmas NJ, Smiddy WE, Flynn HW Jr. Reopening of macular holes after initially successful macular hole surgery. Ophthalmology. 1997. 104:1648–1652.
8. Paques M, Massin P, Blain P, et al. Long-term incidence of reopening of macular holes. Ophthalmology. 2000. 107:760–766.
9. Paques M, Massin P, Santiago PY, et al. Late reopening of successfully treated macular holes. Br J Ophthalmol. 1997. 81:658–662.
10. Ezra E, Aylward WG, Gregor ZJ. Membranectomy and autologous serum for the retreatment of full-thickness macular holes. Arch Ophthalmol. 1997. 115:1276–1280.
11. Ie D, Glaser BM, Thompson JT, et al. Retreatment of full-thickness macular holes persisting after prior vitrectomy. Ophthalmology. 1993. 100:1787–1793.
12. Thompson JT, Sjaarda RN. Surgical treatment of macular holes with multiple recurrence. Ophthalmology. 2000. 107:1073–1077.
13. Smiddy WE, Sjaarda RN, Glaser BM, et al. Reoperation after failed macular hole surgery. Retina. 1996. 16:13–18.
14. Johnson RN, Mcdonald HR, Schatz H, Ai E. Outpatient postoperative fluid gas exchange after early failed vitrectomy surgery for macular hole. Ophthalmology. 1997. 104:2009–2013.
15. Del Priore LV, Kaplan HJ, Bonham RD. Laser photocoagulation and fluid-gas exchange for recurrent macular hole. Retina. 1994. 14:381–382.
16. Ikuno Y, Kamei M, Saito Y, et al. Photocoagulation and fluid-gas exchange to treat persistent macular holes after prior vitrectomy. A pilot study. Ophthalmology. 1998. 105:1411–1418.
17. Ohana E, Blumenkranz MS. Treatment of reopened macular hole after vitrectomy by laser and outpatient fluid-gas exchange. Ophthalmology. 1998. 105:1398–1403.
18. Kang SW, Ahn K, Ham DI. Types of macular hole closure and their clinical implications. Br J Ophthalmol. 2003. 87:1015–1019.
19. Schocket SS, Lakhanpal V, Miao XP. Laser treatment of macular holes. Ophthalmology. 1988. 95:574–582.
20. Matsumoto M, Yoshimura N, Honda Y. Increased production of transforming growth factor-beta 2 from cultured human retinal pigment epithelial cells by photocoagulation. Invest Ophthalmol Vis Sci. 1994. 35:4245–4252.
21. Willis AW, Garcia-Cosio JF. Macular hole surgery. Comparison of longstanding versus recent macular holes. Ophthalmology. 1996. 103:1811–1814.
22. Ullrich S, Haritoglou C, Gass C, et al. Macular hole size as a prognostic factor in macular hole surgery. Br J Ophthalmol. 2002. 86:390–393.
23. Amari F, Ohta K, Kojima H, et al. Predicting visual outcome after macular hole surgery using scanning laser ophthalmoscope microperimetry. Br J Ophthalmol. 2001. 85:96–98.
24. Nao-I N, Matsuura Y, Arai M, et al. Modified vitreous surgery for full-thickness macular hole. Jpn J Clin Ophthalmol. 1994. 48:1989–1994.
25. Sjaarda RN, Frank DA, Glaser BM, et al. Resolution of an absolute scotoma and improvement of relative scotomata after successful macular hole surgery. Am J Ophthalmol. 1993. 116:129–139.
26. Glaser BM, Michels RG, Kuppermann BD, et al. Transforming growth factor-beta2 for the treatment of full-thickness macular holes. A prospective randomized study. Ophthalmology. 1992. 99:1162–1172.
27. Paques M, Chastang C, Mathis A, et al. Effect of autologous platelet concentrate in surgery for idiopathic macular hole. Results of a multicenter, double-masked, randomized trial. Ophthalmology. 1999. 106:932–938.
28. Liggett PE, Skolik DS, Horio B, et al. Human autologous serum for the treatment of full-thickness macular holes. Ophthalmology. 1995. 102:1071–1076.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download