Abstract
This study was performed to evaluate the changes of tear film and ocular surface caused by smoking. Symptom scoring, tear film break-up time (BUT), basal tear secretion test, corneal sensitivity test, keratoepitheliopathy scoring, and conjunctival impression cytology were performed in 29 smokers (58 eyes) and 26 non-smokers (52 eyes). Tear film BUT, basal tear secretion, corneal sensitivity, and squamous metaplasia were 7.71±2.66 sec, 6.29±2.85 mm, 53.69±5.69 mm, and 2.45±1.26 in smokers and 9.62±3.14 sec, 10.04±3.87 mm, 56.46±4.79 mm, and 1.12±0.83 in nonsmokers, respectively (p<0.05). Symptom score, keratoepitheliopathy score, and goblet cell density were not significantly different between the two groups. Tear film BUT was shorter, basal tear secretion and corneal sensitivity were lower, and squamous metaplasia was higher in heavy smokers than in light smokers. In conclusion, smoking deteriorates the tear film and ocular surface with decreased quantity and quality of tear film, decreased corneal sensitivity, and squamous metaplasia, and this deterioration is related to the amount of smoking.
Cigarette smoke contains more than 4,000 compounds, which are toxic upon acute or chronic exposure and eventually poisonous to ocular tissues affecting the eye through ischemic or oxidative mechanism.1 Ophthalmologic disorders associated with cigarette smoking include cataract, age-related macular degeneration, retinal ischemia, anterior ischemic optic neuropathy, Graves' ophthalmopathy and tobacco-alcohol amblyopia.2,3 The conjunctival mucosa is highly sensitive to airborne chemicals, fumes, and irritative gases that originate in tobacco smoke, leading to conjunctival redness, excessive lacrimation and discomfort due to stimulation of the conjunctival-free nerve endings.4 Smoking cigarettes also increases the risk of dry eye syndrome and exacerbates existing conditions.5
Although cigarette smoking is known to cause conjunctival irritation, there have been insufficient studies to determine the specific effects of smoking on tear film and ocular surface including cornea and conjunctiva. This study aimed to investigate the effects of smoking on tear film and ocular surface.
The study was conducted from February to July, 2004. The smoking group comprised 29 male subjects (58 eyes) aged between 27 and 66 (mean age 47.3±10.0) year. All of them had smoked cigarettes for at least one year. The non-smoking group comprised 26 male subjects (52 eyes) aged between 21 and 72 (mean age 44.0±16.7) years. The smoking group was further divided into three subgroups according to the daily amount of smoking: Light smokers who smoke less than one pack (20 cigarettes), moderate smokers who smoke one pack and heavy smokers who smoke more than one pack. Informed consent was obtained from each subject, and the study was performed in accordance with the guidelines of the declaration of Helsinki.
The study excluded those who had a history of drug abuse, contact lens wear, those who had had ocular surgery within the previous three months, those who were using eye drops, those who had abnormalities in the cornea or conjunctiva, those with atopy or allergic diseases and those with secondary ocular or systemic disease. The non-smoking group was recruited after confirming that there were no smokers in their family members to rule out any effects associated with passive smoking. We evaluated symptom score, tear film break-up time (BUT), basic secretion test using Schirmer test strips, corneal sensitivity test, keratoepitheliopathy using fluorescein staining, and conjunctival impression cytology and then compared the parameters in the smoking group with those in the control group. The symptom score was graded on a numerical scale of 0 to 4, with 0 representing no symptoms, 1 representing mild symptoms with no discomfort, 2 representing moderate symptoms, 3 representing severe symptoms, and 4 representing very severe symptoms with discomfort and interfering activities. Tear film BUT and Schirmer test with topical anesthesia (basal tear secretion test) were measured as previously described.6,7 A BUT value of less than 10 sec and a tear secretion value of less than 5 mm were regarded as abnormal.
Corneal sensitivity was measured using a Cochet-Bonnet esthesiometer (Luneau Ophthalmologie, Chartres Cedex, France). The tip of the fully extended nylon filament was applied perpendicularly to the surface of the central cornea and advanced steadily. When the subject felt its presence, the length of the filament was recorded in millimeters. A measurement of less than 45 mm was considered low corneal sensitivity.6
Keratoepitheliopathy was evaluated by staining the cornea with fluorescein and scoring the area and density of staining.8 The severity of keratoepitheliopathy was scored by multiplying the area score by the density score, and this product was used as an index of corneal surface damage. The staining area was graded on a numerical scale of 0 to 3, with 0 representing no punctate staining, 1 representing less than one third, 2 representing one third to two thirds, and 3 representing more than two thirds staining. The staining density was also graded on a numerical scale of 0 to 3, with 0 representing no punctate staining, 1 representing sparse density, 2 representing moderate density, and 3 representing high density with overlapping lesions.
Impression cytology was performed as follows. After topical anesthesia with 0.5% proparacaine hydrochloride (Alcaine, Alcon, USA), 6.2-mm diameter strips of cellulose acetate filter paper (MFS membrane filters, Advantec MFS, USA) were applied, dull side down, to the lower nasal bulbar conjunctiva adjacent to the corneal limbus. The filter strips were pressed gently with blunt, smooth-tipped forceps for 2-3 seconds. They were then gently removed in a peeling motion, avoiding shearing. A solution containing three parts acetone and one part of a mixture of 1/4 95% methanol and 3/4 95% ethanol was freshly prepared. Immediately after pressing the filter strips onto the slides, the slides were placed horizontally in a glass Petri dish for 3-4 hours in the above solution. The slides were then fixed in absolute alcohol, stained with periodic acid - Schiff (PAS) and mounted. Photographs were taken using a light microscope fitted with a calibrated grid at a magnification of X400 and the degree of squamous metaplasia of conjunctival epithelial cells and goblet cell density were then evaluated. The degree of squamous metaplasia was graded from 0 to 3 according to Nelson's9 grading scheme and the goblet cell density was represented as the number of cells per square millimeter. Grade 2 or greater was regarded as abnormal.
Parameters between the groups were analyzed by the Student t-test and analysis of variance with SPSS software. The Mann-Whitney U test and Kruskal-Wallis test were used for the analysis of nonparametric values such as keratoepithelial score and grade of conjunctival squamous metaplasia. A P value of less than 0.05 was considered statistically significant.
There was no significant difference in age between the smoking and control groups. Among the 29 subjects (58 eyes) of the smoking group, there were 11 light smokers (38.0%), 9 moderate smokers (31%) and 9 heavy smokers (31.0%). In the smoking group, 45 eyes (77.6%) had an abnormal BUT value, 21 eyes (36.2%) had an abnormal basal secretion test value, and 5 eyes (8.6%) had low corneal sensitivity. Forty-one eyes (70%) had abnormal impression cytologic findings.
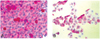
Comparison of tear film and ocular surface parameters between the two groups is shown at Table 1. The symptom score was 0.62±0.73 in the smoking group and 0.70±0.92 in the control group, showing no significant difference between the two groups (p=0.97). The tear film BUT was significantly higher in the smoking group at 7.71±2.66 seconds in the non-smoking group at 9.62±3.14 seconds (p<0.01). Basal tear secretion was significantly lower in the smoking group at 6.29±2.85 mm than in the control group at 10.04±3.87 mm (p<0.01). Corneal sensitivity was 53.69±5.69 mm in the smoking group, which was significantly lower than the 56.46±4.79 mm of the control group (p=0.04). However, there was no significant difference in fluorescein staining score between the smoking and control groups with 0.40±0.77 and 0.38±0.80, respectively (p=0.76). In impression cytologic analysis, the average grade of conjunctival squamous metaplasia was significantly higher in the smoking group (2.45±1.26) than in the control group (1.12±0.83) (p=0.02). There was no significant difference in goblet cell density between the smoking (131.82±125.53 cells/mm2) and control (206.67±155.78 cells/mm2) groups (p=0.23) (Fig. 1).
Comparison of tear film and ocular surface parameters among smokers subdivided by daily smoking amount is presented in Table 2. Tear film BUT decreased significantly with increasing smoking rate: 7.95±3.15 seconds, 7.83±1.92 seconds and 7.28±2.74 seconds for light, moderate and heavy smokers, respectively (p<0.01). The same significant decrease with increasing smoking rate also found for both basal tear secretion, 7.32±3.21 mm, 5.83±2.60 mm and 5.50±2.33 mm, respectively (p<0.01) and corneal sensitivity, 56.81±4.84 mm, 52.50±4.16 mm and 49.75±6.29 mm, respectively (p=0.04). Thus the tear film BUT, basal tear secretion and corneal sensitivity were negatively correlated with the amount of cigarettes smoked per day. However, the smoking rate had no effect on symptom score (p=0.53) and fluorescein staining score (p=0.36). In impression cytologic analysis, the average grade of conjunctival squamous metaplasia was 1.67±1.03 for light smokers, 2.50±1.22 for moderate smokers and 3.38±0.52 for heavy smokers (p=0.03), demonstrating a positive correlation with the amount of smoking. There was no significant relationship between goblet cell density and the amount of cigarettes smoked per day.
It is well known that smoking cigarettes increases the risks of systemic disease and ocular damage. However, there have been few studies investigating the effects of smoking on tear film and dry eye syndrome. Cigarette smoking is regarded as one of the risk factors for the development of dry eye symptoms, and cigarette smoke contain numerous compounds that can be irritative and toxic. Given this evidence, cigarette smoking may take its toll on tear film stability and ocular surface wetting, in addition to its irritative effect on the ocular surface, through the stimulation of the conjunctiva and cornea, ischemic or oxidative mechanism that involves inducing oxygen free radicals and decreasing antioxidant mechanisms.10
Two studies investigating the effects of smoking on tear film function and tear secretion reported that tear film BUT decreased in smokers and that tear film stability decreased in the eyes of aircrew members on smoking flights.5,11 Histopathological and ultrastructural examination of the rat conjunctiva after exposure to tobacco smoke revealed a deterioration of projections and loss of microvilli, which are important for stabilizing the tear film.12 Satici et al5 reported that Schirmer test values (without topical anesthesia) of smokers were higher than those of controls and that tear lysozyme concentrations of smokers were lower than those of controls. The low concentration level of tear lysozyme found in smoking individuals may be explained by the destruction of lysozyme in the conjunctival sac, the binding of the lysozyme locally by toxins in the smoke, the dilution developed due to excessive tearing in smokers, or the chemical conjunctivitis developed by smoke.5,13 Grus et al14 analyzed and compared electrophoretic patterns in the tears of smokers, severe smokers, and nonsmokers. Tear protein patterns in smokers and severe smokers were different from those of nonsmokers, and there was significantly more protein peaks in the severe smokers than in the nonsmokers. On the other hand, Gabela Merino et al15 reported that smoking did not seem to affect tear meniscus, Schirmer test with anesthesia, non invasive BUT, and slit lamp examination and fluorescein staining in a population of hydrogel contact lens wearers.
The smoking group in the present study had a shorter tear film BUT, a lower rate of basal tear secretion and reduced corneal sensitivity than the control group. It is likely that the negative impact of cigarette smoke on the lipid layer of the tear film is the main cause of such deterioration in tear film BUT. A decrease in basal tear secretion presented fresh evidence to support the findings of earlier studies that cigarette smoke increases reflex and that tear secretion increased among smokers according to Schirmer I test. Nowadays, it is assumed that cigarette smoke increases total tear secretion and reflex tear secretion but decreases basal tear secretion.5 There was, however, no significant difference in keratoepitheliopathy and symptom scores between the two groups. This result is explained by increased reflex tear secretion and reduced corneal sensitivity, both of which are common among smokers.
Smoking can cause ocular surface epithelium damage as smoke directly contacts with the ocular surface. Polymorphonuclear leukocytes and squamous epithelium cell counts were increased both before and after a workshift among tobacco workers, and tobacco smoke altered the conjunctival structure in rats by causing squamous metaplasia in the conjunctival surface epithelial layer.12,16 Satici et al5 reported that the degree of conjunctival squamous metaplasia of smokers was higher than that of controls, but that the goblet cell counts did not differ between two groups. The mechanism of squamous metaplasia may be inflammation associated with irritative and toxic agents and the absence of circulating and growth factors required for epithelial differentiation. In this study, the grade of squamous metaplasia was significantly higher in the smoking group than in the control group according to the impression cytology findings. Goblet cell density decreased slightly but not significantly in the smoking group. These results suggest that smoking is the major cause of the damage in conjunctival epithelial cells.
Analysis of these changes with the daily amount of smoking further confirmed that tear film BUT, basal tear secretion and corneal sensitivity were negatively correlated with the amount of smoking. However, there were no differences in keratoepitheliopathy and symptom scores among the smokers by smoking rate. In impression cytology analysis, the grade of squamous metaplasia was positively correlated with the amount of cigarettes smoked per day. However, goblet cell density was not related to the amount of smoking.
In conclusion, smoking cigarettes undermined the tear film and ocular surface by decreasing both the quantity and quality of tear secretion, reducing corneal sensitivity and inducing squamous metaplasia. It is therefore recommended that patients with dry eye syndrome and ocular surface disorders avoid smoking, even if they do not have severe dry eye presentation.
Figures and Tables
Fig. 1
Impression cytology (PAS, ×400). (A) Specimen from a nonsmoker shows PAS positive goblet cells and small, round epithelial cells with a nucleocytoplasmic ratio of 1:2. (B) Specimen from a heavy smoker shows a loss of goblet cells and large, polygonal epithelial cells with a nucleocytoplasmic ratio of 1:6.
References
1. Solberg Y, Rosner M, Belkin M. The association between cigarette smoking and ocular diseases. Surv Ophthalmol. 1998. 42:535–547.
2. Seddon J, Fong D. Introducing "Public health and the eye". Surv Opthalmol. 1994. 38:325.
3. Cheng ACK, Pang CP, Leung ATS, et al. The association between cigarette smoking and ocular disease. Hong Kong Med J. 2000. 6:195–202.
4. Cometto-Muniz JE, Cain WS. Sensory irritation. Relation to indoor air pollution. Ann N Y Acad Sci. 1992. 641:137–151.
5. Satici A, Bitiren M, Ozardali I, et al. The effects of chronic smoking on the ocular surface and tear characteristics: a clinical, histological and biochemical study. Acta Ophthalmol Scand. 2003. 81:583–587.
6. Dogru M, Katakami C, Inoue M. Tear function and ocular surface changes in noninsulin-dependent diabetes mellitus. Ophthalmology. 2001. 108:586–592.
7. Jones LT. The lacrimal secretory system and its treatment. Am J Ophthalmol. 1966. 62:47–60.
8. Miyata K, Amano S, Sawa M, Nishida T. A novel grading method for superficial punctate keratopathy magnitude and its correlation with cornea epithelial permeability. Arch Ophthalmol. 2003. 121:1537–1539.
9. Nelson JD. Impression cytology. Cornea. 1988. 7:71–81.
10. Moss SE, Klein R, Klein BE. Prevalence of and risk factors for dry eye syndrome. Arch Ophthalmol. 2000. 118:1264–1268.
11. Weislander G, Lindgren T, Norback D, Venge P. Changes in the ocular and nasal signs and symptoms of aircrew in relation to the ban on smoking on intercontinental flights. Scan J Work Environ Health. 2000. 26:514–522.
12. Avunduk AM, Avunduk MC, Evirgen O, et al. Histopathological and ultrastructural examination of the rat conjunctiva after exposure to tobacco smoke. Ophthalmologica. 1997. 211:296–300.
13. Sen DK, Sarin GS. Biological variations of lysozyme concentration in the tear fluids of healthy persons. Br J Ophthalmol. 1986. 70:246–248.
14. Grus FH, Sabuncuo P, Augustin A, Pfeiffer N. Effect of smoking on tear protein. Graefes Arch Clin Exp Ophthalmol. 2002. 240:889–892.
15. Gabela Merino M, Gonzalez Garcia MJ, Mayo Iscar A, Calonge Cano M. Dry eye signs and symptoms in hydrogel contact lens wearers: relation to smoking habit. Arch Soc Esp Oftalmol. 2003. 78:543–548.
16. Kjaergaard SK, Pederson OF. Dust exposure, eye redness, eye cytology, and mucous membrane irritation in a tobacco industry. Int Arch Occup Environ Health. 1989. 61:519–525.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download